Background
The evaluation of elderly patients presenting with abdominal pain poses a difficult challenge for the emergency physician. It will become an increasingly common problem because the elderly population in the United States is growing rapidly. The definition of elderly varies among authors, but for the purpose of this subject, age 60 years is a reasonable starting point.
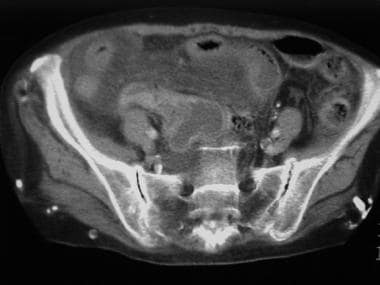
Studies published in the 1980s and 1990s demonstrated that, among elderly patients presenting to the ED with abdominal pain, at least 50% were hospitalized and 30-40% eventually had surgery for the underlying condition. These studies also showed that approximately 40% of these patients were misdiagnosed, contributing to an overall mortality rate of approximately 10%. The image below illustrates an inflammatory mass of an elderly woman with a ruptured appendix.
 Inflammatory mass in the right lower quadrant of an 84-year-old woman with mild abdominal pain of 2 days' duration. A ruptured appendix was found at surgery.
Inflammatory mass in the right lower quadrant of an 84-year-old woman with mild abdominal pain of 2 days' duration. A ruptured appendix was found at surgery.
In the period of time since the last of these studies was published, the availability and accuracy of emergency diagnostic techniques have improved dramatically. Computed tomography and ultrasonography were not widely used in most EDs before the mid 1990s. Today, it is relatively rare for a patient with significant abdominal pain to leave the ED without some type of advanced imaging. Diagnostic accuracy and presumably short-term mortality very likely have improved since the bulk of the studies on this subject were published. In fact, two newer studies showed that CT scanning significantly improved the certainty of diagnosis and altered therapy in elderly patients. [1, 2] Even though imaging has improved diagnostic accuracy, the risk for adverse outcome in this patient population remains high. The only studies published since the widespread use of advanced imaging showed that nearly 60% were hospitalized, and, in the following 2 weeks, 20% underwent surgery and 5% died. [3, 4]
Multiple factors contribute to the diagnostic difficulty and high incidence of complications seen in elderly patients. Immune function tends to decrease with advancing age. Many elderly patients have underlying conditions such as diabetes or malignancy, further suppressing immunity. Elderly patients often have underlying cardiovascular and pulmonary disease, which decreases physiologic reserve and predisposes them to conditions such as abdominal aortic aneurysm (AAA) and mesenteric ischemia. Elderly patients also have a high incidence of asymptomatic underlying pathology. Up to one half of elderly patients have underlying cholelithiasis, one half have diverticula, and 5-10% have AAA.
Understanding that elderly patients may present very differently than their younger counterparts also is important. Elderly patients tend to wait much longer to seek medical attention than younger patients, and they are much more likely to present with vague symptoms and have nonspecific findings on examination. Many elderly patients have a diminished sensorium, allowing pathology to advance to a dangerous point prior to symptom development. Elderly patients with acute peritonitis are much less likely to have the classic findings of rebound tenderness and local rigidity. [4] They are less likely to have fever, leukocytosis, or elevated C-reactive protein level. In addition, their pain is likely to be much less severe than expected for a particular disease.
Because of these factors, many elderly patients with serious pathology initially are misdiagnosed with benign conditions such as gastroenteritis or constipation. They also are at greater risk of being admitted to the wrong service (eg, internal medicine when a surgeon may be required).
A careful history and physical examination as well as a high index of suspicion are crucial to prevent missed diagnoses.
Mortality varies greatly depending on the underlying pathology. Approximately 30-40% of patients require surgery, and overall mortality is approximately 10%.
For patient education resources, see Digestive Disorders Center, as well as Abdominal Pain (Adults), Appendicitis, Diverticulitis (Diverticulosis), Gastroenteritis (Stomach Flu), Constipation (Adults), and Blood in the Urine.
Pathophysiology
Abdominal pain may be the presenting symptom in a wide range of diseases in elderly patients. Note that elderly patients with intra-abdominal pathology are more likely to present with symptoms other than abdominal pain, such as fever, fatigue, chest pain, or altered mental status.
Biliary tract disease
Biliary tract disease includes symptomatic cholelithiasis, choledocholithiasis, calculus and acalculous cholecystitis, and ascending cholangitis.
In some studies, biliary tract disease is the most common diagnosis among elderly patients presenting with abdominal pain.
Approximately 30-50% of patients older than 65 years have gallstones.
The mortality rate of elderly patients diagnosed with cholecystitis is approximately 10%. Cholecystitis is acalculous in approximately 10% of elderly patients with the condition. Classically, the diagnosis requires the presence of right upper quadrant pain associated with fever and leukocytosis. Unfortunately, 25% of elderly patients may have no significant pain, and less than one half have fever, vomiting, or leukocytosis. The diagnosis therefore can be difficult in this age group, requiring a high index of suspicion.
Complications of biliary tract disease include gallbladder perforation, emphysematous cholecystitis, ascending cholangitis, and gallstone ileus, which is responsible for approximately 2% of cases of small bowel obstruction in elderly patients.
Appendicitis
Appendicitis is a less common cause of abdominal pain in elderly patients than in younger patients, but the incidence among elderly patients appears to be rising. Only approximately 10% of cases of acute appendicitis occur in patients older than 60 years, whereas one half of all deaths from appendicitis occur in this age group.
The rate of perforation in elderly patients is approximately 50%, 5 times higher than in younger adults. This is largely because 75% of elderly patients wait more than 24 hours to seek medical attention.
The diagnosis can be difficult to make, since more than one half of patients in this age group do not present with fever or leukocytosis. Further confusing the picture, approximately one third do not localize pain to the right lower quadrant, and one fourth do not have appreciable right lower quadrant tenderness.
Only 20% of elderly patients present with anorexia, fever, right lower quadrant pain, and leukocytosis. The initial diagnosis is incorrect in 40-50% of patients in this age range.
All of the above factors contribute to delayed diagnosis and high complication rates. A 10-year retrospective review found that the diagnosis was delayed in 35% of patients. [5] Again, a high index of suspicion is necessary to avoid missing this diagnosis.
Diverticulitis
The formation of diverticula in the colon is largely a product of diet and age and is relatively rare in those younger than 40 years. In the United States, diverticula are present in approximately 50-80% of patients older than 65 years.
Diverticulitis results when diverticula become obstructed by fecal matter, resulting in lymphatic obstruction, inflammation, and perforation. By definition, diverticulitis involves at least microperforation of the colon.
Approximately 85% of cases occur in the left colon. Right-sided diverticulitis is often more difficult to diagnose and generally is more benign.
Elderly patients with diverticulitis are often afebrile, and an elevated WBC count is observed in less than one half. Only approximately 25% of patients have guaiac positive stool.
Mesenteric ischemia
Including mesenteric ischemia (see the image below) in the differential is important, even though it accounts for less than 1% of cases of abdominal pain in elderly patients. A study from Finland suggests that acute mesenteric ischemia may be an underestimated cause of acute abdomen. [6]
 CT scan of a 76-year-old woman with severe abdominal pain of 3 hours' duration. Note the ringlike enhancement of bowel wall in the posterior abdomen. Ischemic small bowel was resected at surgery.
CT scan of a 76-year-old woman with severe abdominal pain of 3 hours' duration. Note the ringlike enhancement of bowel wall in the posterior abdomen. Ischemic small bowel was resected at surgery.
Mortality ranges from 70-90%, and any delay in diagnosis increases the risk of death.
Patients classically present with severe abdominal pain despite having little tenderness on examination. Vomiting and diarrhea are often present.
Risk factors for the development of mesenteric ischemia include atrial fibrillation, atherosclerotic disease, and low ejection fraction.
Occasionally patients may present with recurrent episodes of postprandial abdominal pain, sometimes termed intestinal angina.
Bowel obstruction
Bowel obstruction accounts for approximately 12% of cases of abdominal pain in elderly patients. Obstruction is classified as blockage of either the small bowel or the large bowel, although the distinction can be difficult to make clinically (see Small-Bowel Obstruction and Large-Bowel Obstruction).
Cecal volvulus is relatively rare and typically presents clinically as small bowel obstruction. Sigmoid volvulus is much more common and often can be identified by plain abdominal radiography. See the image below.
 Radiograph of a 90-year-old man with abdominal pain of 4 days' duration. Plain films reveal large bowel dilatation. Sigmoid volvulus with ischemic colon was diagnosed at surgery.
Radiograph of a 90-year-old man with abdominal pain of 4 days' duration. Plain films reveal large bowel dilatation. Sigmoid volvulus with ischemic colon was diagnosed at surgery.
Distension of the colon of more than 9 cm can signal impending perforation.
Risk factors for sigmoid volvulus include inactivity and laxative use, both of which are common in elderly patients.
Abdominal aortic aneurysm
AAA is observed almost exclusively in elderly patients. Approximately 5% of men older than 65 years have AAA. The male-to-female ratio is 7:1.
If the diagnosis of ruptured AAA is made in the hemodynamically stable patient, the mortality is approximately 25%. In patients presenting in shock, the mortality is 80%.
Maintain a high index of suspicion, since many patients present with a clinical picture suggestive of renal colic or musculoskeletal back pain. Approximately 30% of patients with ruptured AAA are misdiagnosed initially.
Peptic ulcer disease
Peptic ulcer disease (PUD) deserves special mention, since the incidence among elderly patients is increasing. This may be due in part to the increasing availability and use of nonsteroidal anti-inflammatory drugs (NSAIDs). Users of NSAIDs are 5-10 times more likely to develop PUD than nonusers.
Mortality of elderly patients with PUD is approximately 100 times higher than that of younger patients with PUD.
Diagnosis of PUD in elderly patients can be difficult. Approximately 35% of elderly patients with PUD have no pain. The most common presenting symptom is melena.
Complications include hemorrhage and perforation. In elderly patients perforation is often painless, and free air may be absent on plain radiographs in more than 60% of patients.
Malignancy
Among elderly patients discharged from the ED with a diagnosis of nonspecific abdominal pain, approximately 10% eventually are diagnosed with an underlying malignancy.
Gastroenteritis
Consider gastroenteritis a diagnosis of exclusion in elderly patients with vomiting and diarrhea. Vomiting and diarrhea can be caused by many illnesses. Reviews of cases of missed appendicitis reveal that approximately one half of patients initially were diagnosed with gastroenteritis.
Even when more dangerous conditions have been excluded, realize that gastroenteritis can cause serious morbidity in elderly patients. Of all deaths due to gastroenteritis, approximately two thirds occur in patients older than 70 years.
Urinary tract infection
Elderly patients with urinary tract infection are much less likely to have symptoms of dysuria, frequency, or urgency than younger patients (see Urinary Tract Infection (UTI) and Cystitis (Bladder Infection) in Females and Urinary Tract Infection (UTI) in Males).
Other
Myocardial infarction and pneumonia also commonly present as vague abdominal complaints in elderly patients. [7, 8]
Etiology
Causes of abdominal pain in elderly patients are as follows (see Pathophysiology for more information):
-
Biliary tract disease
-
Appendicitis
-
Diverticulitis
-
Mesenteric ischemia (risk factors include atrial fibrillation, atherosclerotic disease, and low ejection fraction)
-
Peptic ulcer disease
-
Malignancy
-
Gastroenteritis
Bowel obstruction
Small bowel obstruction most often is caused by adhesions from previous surgery. In elderly patients, an incarcerated hernia, as shown below, causes approximately 30% of cases, and approximately 20% are caused by gallstone ileus.
 CT scan of a 64-year-old woman with vague abdominal pain of 2 days' duration. Physical examination revealed a tender palpable mass in the left lower quadrant. CT scan reveals an incarcerated ventral hernia.
CT scan of a 64-year-old woman with vague abdominal pain of 2 days' duration. Physical examination revealed a tender palpable mass in the left lower quadrant. CT scan reveals an incarcerated ventral hernia.
Large bowel obstruction is most often caused by malignancy or volvulus.
Epidemiology
Race-related demographics
Some causes of abdominal pain in elderly patients may vary by race due to the incidence of predisposing factors such as biliary tract disease, diabetes, and hypertension.
Age-related demographics
With advancing age, diagnostic accuracy steadily decreases, and mortality steadily increases.
A prospective study (1988-2004) that used self-report questionnaires to assess the effects of aging on the natural history of abodominal pain in 1,913 US adults on initial and follow-up surveys reported the following findings [9] :
-
Abdominal pain disappearance was associated with older age at initial survey and the period between surveys
-
Factors associated with the onset of abdominal pain included female sex, higher somatization scores, and larger changes in somatization scores
-
Onset of abdominal pain was associated with younger age at initial survey
-
There was an 18% rate of onset and 47% disappearance rate of abdominal pain over time
-
The rates of increasing abdominal pain score were 18% compared to rates of 21% for decreasing pain score
-
Inflammatory mass in the right lower quadrant of an 84-year-old woman with mild abdominal pain of 2 days' duration. A ruptured appendix was found at surgery.
-
CT scan of a 76-year-old woman with severe abdominal pain of 3 hours' duration. Note the ringlike enhancement of bowel wall in the posterior abdomen. Ischemic small bowel was resected at surgery.
-
Radiograph of a 90-year-old man with abdominal pain of 4 days' duration. Plain films reveal large bowel dilatation. Sigmoid volvulus with ischemic colon was diagnosed at surgery.
-
Radiograph of a 79-year-old woman with several hours of diffuse abdominal pain. Initial examination of the plain films suggests bowel obstruction.
-
Radiograph of a 79-year-old woman with several hours of diffuse abdominal pain. Initial examination of the plain films suggests bowel obstruction. Close-up view reveals pneumatosis intestinalis, indicating mesenteric ischemia.
-
CT scan of a 64-year-old woman with vague abdominal pain of 2 days' duration. Physical examination revealed a tender palpable mass in the left lower quadrant. CT scan reveals an incarcerated ventral hernia.
-
CT scan of a 62-year-old man who reported 2 weeks of left lower quadrant abdominal pain. CT scan reveals fat stranding and multiple diverticula around the descending colon. A phlegmon containing bowel and inflammatory tissue has eroded into the left psoas muscle.
-
A lower CT scan slice from a 62-year-old man who reported 2 weeks of left lower quadrant abdominal pain. Multiple diverticula are observed with an inflammatory mass overlying the left ilium.







