Practice Essentials
Emergency medicine physicians may diagnose sarcoidosis de novo or provide emergent management of its exacerbations, recurrences, and/or acute complications. Sarcoidosis is a chronic noncaseating granulomatous disease of unknown etiology that affects many organs and tissues; the lungs are most commonly involved, but significant morbidity and mortality may also occur due to granulomatous infiltration of the heart, eyes, and nervous system. [1] Although sarcoidosis may be suspected because of a patient's history, it usually is diagnosed by using chest radiography and histology. (See the images below.)
 Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
 Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
 Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
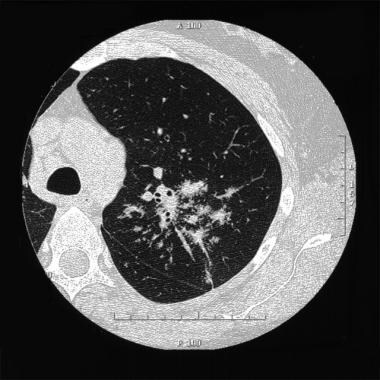 Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
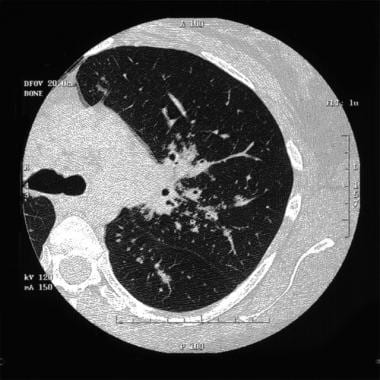 Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
The treatment of symptomatic sarcoidosis usually includes glucocorticoids, and cytotoxic drugs such as methotrexate, azathioprine, cyclosphosphamide, mycophenolate mofetil. Biologic therapy with a tumor necrosis factor alpha (TNFα) antagonist (eg, adalimumab) may be considered in severe or refractory sarcoidosis. The use of immunosupressive drugs, mainly cyclosphosphamide, is associated with an increased risk for infection [2]
Patients with sarcoidosis also have a higher risk of cardiovascular disease (CVD) and glucocorticoids, the most commonly used medication in management of sarcoidosis, may be a contributing factor as long-term use is associated with several traditional CVD risk factors such as diabetes mellitus, hypertension, and dyslipidemia. [3]
In a population-based retrospective study, a threefold increased risk of venous thromboembolism (VTE) was reported with significantly elevated risk for both deep vein thrombosis (DVT) and pulmonary embolism (PE). [4]
Patient History
In the emergency department (ED), a patient may present with nonspecific complaints or be diagnosed incidentally by radiograph and/or other findings. Approximately 50% of patients are asymptomatic at diagnosis. Patients may present to the ED with a known diagnosis of sarcoidosis and complain of symptoms consistent with a recurrence. Because sarcoidosis is a multiorgan disease, patients may complain of a variety of symptoms that may complicate diagnosis.
The organs most affected are as follows:
-
Lungs - 90% with abnormal chest radiographic findings at some point
-
Lymphatics - 75% of pulmonary and 60% of peripheral
-
Skin - 25% [5]
-
Eyes - 75% [6]
-
Bone marrow - 30%
-
Liver - 50-80% [7]
-
Spleen - 40%
-
Upper respiratory tract - Nose, tonsils in 20%
-
Salivary glands - Parotitis
-
Musculoskeletal - 25-39% [5] Acute or chronic arthritis; see Lofgren syndrome, below
-
Kidney -2-10% Mainly as a kidney stone secondary to hypercalcemia produced by calcitriol hyperactivity of macrophages [5]
-
Central nervous system - 5-15% [8]
-
Joint - 25%
-
Heart - 5-25%; can present as a conduction defect; also, in advanced cases, pulmonary hypertension causes cor pulmonale [5]
-
Endocrine system
-
Gastrointestinal system < 1% [7]
In a study of 588 consecutive Japanese patients newly diagnosed with sarcoidosis between 1974 and 2012, patients under age 45 presented more often with involvement of extrathoracic lymph nodes, the parotid/salivary gland, and liver, while patients aged 45 and older presented more often with involvement of non-lymphatic extrathoracic organs, including the eyes, heart, muscles, and kidney. Age at diagnosis increased over the study period. [9]
Patients may present with the following:
-
No symptoms; diagnosed incidentally because of chest radiographic findings
-
Abrupt onset of signs and symptoms evolving over 1-3 weeks; occurs in 40% of cases and consists of constitutional complaints and/or other findings
-
Gradual onset that evolves over a few months and is observed in 60% of patients; respiratory signs and symptoms predominate
-
Recurrences
Constitutional signs and symptoms
Constitutional signs and symptoms include the following:
-
Fever/night sweats
-
Malaise
-
Fatigue
-
Weight loss
-
Arthritis, uveitis, cranial nerve VII involvement, and parotid enlargement (ie, Heerfordt-Waldenström syndrome)
Pulmonary signs and symptoms
Approximately 90% of patients have an abnormal radiographic finding at some stage of the disease; 10% have pulmonary fibrosis. Pulmonary symptoms include the following:
-
Dry cough
-
Dyspnea that worsens upon or with exertion
-
Occasional hemoptysis
-
Pleural effusion and pneumothorax (rare)
Cardiac signs and symptoms
Cardiac sarcoidoisis is the second leading cause of sarcoidosis mortality. Patients with cardiac involvement may be asymptomatic and once sarcoidosis is diagnosed, they should receive annual screening for cardiac abnormalities. The most common abnormality is atrioventricular block. Other signs and symptoms include the following [5] :
-
Chest pain
-
Palpitations
-
Dyspnea
-
Congestive heart failure
-
Pericardial effusion or syncope/presyncope due to dysrhythmias
Lymphadenopathy
Enlarged lymph nodes are found in hilar and peripheral locations, such as cervical, axillary, and inguinal.
Dermatologic signs and symptoms
Dermatologic manifestations include the following:
-
Maculopapular eruptions involving the nares, lips, eyelids, and previous trauma areas
-
Lupus pernio (specific for sarcoidosis), a plaquelike lesion of violaceous discoloration of the nose, cheeks, chin, and ears
-
Erythema nodosum (EN), the most common skin manifestation, referred to as Lofgren syndrome when it occurs with radiographic findings of bilateral hilar or paratracheal adenopathy and joint involvement (EN is associated with a good prognosis)
-
Subcutaneous nodules
Ocular lesions
Ocular involvement is the presenting symptom in 20%–30% of cases and may be characterized by granulomatous inflammation which can affect any part of the eye and its adnexa. The most common ocular manifestations are uveitis, dry eye and conjunctival nodules. Glaucoma and cataract can be complications from inflammation itself or adverse effects from therapy. [6]
Neurologic signs and symptoms
Neurosarcoidosis is sometimes called “the great imitator” since it can cause nonspecific and variable symptoms simulating many other conditions. Given the wide a range of neurologic involvement, patients may present with virtually any neurologic complaint. Neurologic manifestations include the following:
-
Facial numbness and dysphagia
-
Hoarseness
-
Decreased gag reflex
-
Headache
-
Visual deficit
-
Polydipsia
-
Deafness
-
Involvement of cranial nerves VII, VIII, IX, and X
-
Basal granulomatous meningitis with involvement of optic chiasm and optic nerve
-
Signs of meningitis - Aseptic meningitis that, on cerebrospinal fluid (CSF) examination, shows decreased glucose, increased protein, increased lymphocytes
-
Involvement of the hypothalamic-pituitary axis - Manifests with pituitary insufficiency, optic chiasm compression, diabetes insipidus
-
Seizures
-
Vasculitis [10]
-
Stroke or transient ischemic attack
-
Peripheral neuropathy - Possibly manifesting with paresthesias and decreased deep tendon reflexes (DTRs)
Physical Examination
Dermatologic findings
Clinical examination of the skin may reveal the following:
-
Maculopapular eruptions
-
Lupus pernio - Violaceous lesions on the face and/or extremities
-
Erythema nodosum – Red, painful lesion on the extensor surface of the lower extremities; considered to be the most common skin lesion in sarcoidosis
-
Granuloma formation in old scar or tattoo and subcutaneous nodules
Neurologic findings
Neurologic manifestations include cranial nerve VII involvement (unilaterally or bilaterally), Bell palsy, basal granulomatous meningitis (ie, aseptic meningitis), or peripheral neuropathies; each presenting with the proper constellation of symptoms
Ocular findings
Before the systemic manifestations of sarcoidosis develop, patients may present with ophthalmologic or neuro-ophthalmologic manifestations such as the following:
-
Uveitis - Blurry vision, tearing, and photophobia
-
Conjunctiva - Infiltration that has the appearance of a yellowish nodule
-
Keratitis sicca - Complaints of dry eyes
Decreased vision or visual field defects are secondary to involvement of the optic nerve and its visual pathway; papilledema is secondary to increased intracranial pressure. Additional findings include abnormal eye movement, pupillary abnormalities, and visual hallucinations. [6]
Musculoskeletal findings
Musculoskeletal manifestations include myositis, bony lesions, and polyarthritis. Regarding the third symptom, spondyloarthropathy has been found to have a higher incidence and prevalence in patients with sarcoidosis (6.6%) than in the general population (1.9%). An association with HLA-B27 has been determined, suggesting an association between sarcoidosis and spondyloarthropathy. Thus, a patient with sarcoidosis may present with back pain or sacroiliac pain. Note that Lofgren syndrome includes arthritis. [11]
In a study of 11 patients with sarcoidosis manifesting with progressive, generalized myopathy (confirmed with muscle biopsy), nine patients showed evidence of muscle atrophy, primarily in the lower limbs. Skeletal muscle computed tomography showed muscle atrophy distributed predominantly in the hip adductors, knee flexors and ankle plantar flexors. Radiologic evaluations suggested skeletal muscle inflammation in just half of the patients, but muscle biopsy showed an active inflammatory process in all of the patients. Treatment response was better in patients with a shorter duration of disease. [12]
Head, neck, and upper respiratory tract findings
Symptoms involving the head, neck, and upper respiratory tract include the following:
-
Dry cough
-
Rales
-
Tonsillitis, parotitis (Heerfordt syndrome), and epiglottitis that presents as hoarseness, stridor, or cough
-
Nasal involvement - May present as damage to the septum and turbinates
Cardiac findings
Cardiac manfiestations include the following:
-
Cor pulmonale (most common cardiac complication) - Caused by pulmonary fibrosis
-
Complete heart block, ventricular tachycardia (most common arrhythmia), bundle-branch block (BBB), ventricular aneurysm, myocarditis, pericarditis, and congestive heart failure (CHF)
Additional findings
Patients with sarcoidosis may also demonstrate the following:
-
Painless, nonadherent lymph nodes
-
Splenomegaly - Occurs in 10% of cases; presents with hematologic and general complications (eg, rupture)
-
Hepatomegaly - Occurs in 25% of cases, with elevation in liver function tests [LFTs]; usually not clinically significant
-
Nephrolithiasis - May be caused by hypercalcemia and hypercalciuria secondary to increase in 1,25-dihydroxyvitamin D and calcitriol production by activated macrophages
-
Clinically significant renal failure (uncommon)
Differential Diagnosis
Consider the possibility of other life-threatening conditions (eg, pulmonary embolism) if no evidence of sarcoidosis is documented in the ED and a patient complains of dyspnea.
Conditions to consider in the differential diagnosis of sarcoidosis include the following (tuberculosis and lymphoma are particularly important in the United States):
-
Lymphoma
-
Lung cancer
-
Parasitic infections (eg, leshmaniosis, schistosomiasis)
-
Pneumoconiosis (eg, silicosis, berylliosis)
-
Viral infections (eg, cytomegalovirus, Epstein-Barr virus)
Laboratory Studies
A complete blood count (CBC) with differential should be performed, and may show leukocytosis with or without eosinophilia. Other laboratory findings may include the following:
-
Elevated erythrocyte sedimentation rate (ESR)
-
Elevated serum angiotensin-converting enzyme (ACE) level - Elevated in 75% of cases; the value of monitoring ACE levels remains unclear
-
Increased serum PO 4 and alkaline phosphatase levels
-
Increased calcium levels - May be revealed with a 24-hour urinalysis assessment
-
Immunologic studies can show falsely elevated antinuclear antibodies (ANA) and rheumatoid factor (RF) levels and hypergammaglobulinemia
Hypercalcemia is observed in 10-15% of cases. It may be helpful to use the mnemonic for common causes of hypercalcemia, "Pam P. Schmidt," the letters of which represent the following:
-
P - Parathyroid hormone (PTH)
-
A - Addison disease
-
M - Multiple myeloma
-
P - Paget disease
-
S - Sarcoidosis (or other granulomatous disease)
-
C - Cancer (lungs, multiple myeloma, breast)
-
M - Milk-alkali syndrome
-
I - Immobilization
-
D - Vitamin D
-
T - Thiazides
Although hypercalcemia is present by definition in sarcoidosis, it is rarely clinically significant. If other organs are involved, such as the liver, kidney, or endocrine organs, laboratory results pertinent to these organs are abnormal.
Patients with sarcoidosis may have myocardial involvement and elevated creatine kinase (CK) and CK-MB levels.
Studies also include slit lamp examination; this is generally is obtained periodically, even if the patient is asymptomatic.
Imaging Studies
Radiography
Chest radiography is an integral part of the diagnosis and staging. [13] In addition, the radiograph may demonstrate pleural involvement, such as a pneumothorax or pleural effusion. Stages of sarcoidosis, as identified through imaging, are as follows (see also the images below):
-
Stage O - No findings
-
Stage I - Bilateral hilar adenopathy
-
Stage II - Bilateral hilar adenopathy and parenchymal involvement (reticular opacities)
-
Stage III - Parenchymal involvement (reticular opacities) with shrinking adenopathy
-
Stage IV - Parenchymal involvement turns into volume loss (pulmonary fibrosis); cavitations and calcifications may also be seen
 Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
 Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
Radiotracer scanning
Gallium-67 scanning is used for staging of disease and for detecting extrapulmonary sarcoidosis. Gallium bound by inflammatory tissue and not by fibrotic tissue can distinguish areas of fibrosis from inflammation.
Other types of radiotracer scanning may be available. Technetium-labeled depreotide that binds somatostatin receptors has been used with good results in some cases. [14]
Bronchoalveolar Lavage
Bronchoalveolar lavage (BAL) shows increases in the CD4/CD8 ratio, lymphocytes, and cytokines. Studies performed to correlate the presence of these markers with prognosis were not conclusive.
However, a study by Bacha et al showed that a high CD4/CD8 ratio seems to be predictive of a poor prognosis in patients with multiple extrathoracic organ involvement. Their study of 40 patients with clinically and histologically evident sarcoidosis showed that, before corticosteroid treatment, total cell count was increased with a T lymphocytosis and an increase in the CD4/CD8 ratio, as shown in BAL fluid. After corticosteroid treatment, a significant decrease in CD4/CD8 ratio and lymphocyte proportion was noted in BAL fluid. Patients with multiple extrathoracic lesions had significantly higher CD4/CD8 ratios than did those with only intrathoracic involvement. [15]
Additional Tests
Skin anergy with purified protein derivative (PPD) is common in patients with sarcoidosis but obviously not specific. With regard to cardiac assessment, a Holter monitor study may be indicated to detect arrhythmias.
Biopsy
Biopsy is an integral part of the diagnosis and has very high yield. The site of biopsy is dictated by clinical presentation of the organ involved. The sensitivity is highest from lung parenchyma, and 5-10 biopsy specimens generally are needed.
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has high diagnostic accuracy for tuberculosis and the sonographic images can also aid in differentiating lymphadenopathy from sarcoidosis. [8]
Pulmonary function tests
Pulmonary function tests (PFTs) are not required for diagnosis, but results may range from reference range to findings consistent with restrictive lung disease.
Electrocardiography
Electrocardiography may reveal the following:
-
Signs of hypercalcemia (eg, decreased QT interval)
-
Ventricular tachycardia
-
Bundle-branch block or complete heart blocks
-
ST elevation, PR depression caused by pericarditis, or ST elevation caused by ventricular aneurysm
Kveim-Stilzbach test
In this study, a suspension from the spleen or a lymph node of a patient with a confirmed diagnosis of sarcoidosis is injected intradermally into a patient suspected to be affected by the disease. Test results are considered positive if a nodule appears within 2-7 weeks. A biopsy sample is then taken from the nodule to find similarities to sarcoid granuloma. The time required for this test, the incidence of false-negative and false-positive results, and the availability of more timely diagnostic tests make this procedure unpopular in the United States.
Prehospital Care
Focus prehospital care on immediate or potential life threats. Initial assessment of the patient always begins with attention to airway, breathing, and circulation (the ABCs). Focus on respiratory support and ensuring adequacy of oxygenation, because patients generally present with respiratory complaints.
Provide supplemental oxygen to all patients. Patients with signs of impending respiratory failure should have ventilatory assistance with bag-valve-mask (BVM) and high-flow oxygen. Consider intubation if a patient's condition continues to deteriorate. Perform continuous pulse oximetry if available.
Obtain intravenous access for all patients except those who have minimal complaints. Provide judicious fluid boluses to patients with evidence of dehydration. Monitor cardiac function of all patients with a history of sarcoidosis because of the potential for cardiac involvement.
Because many patients with sarcoidosis are treated with steroids, consider the possibility of altered glucose metabolism and perform blood glucose determinations.
Emergency Department Care
Perform a primary evaluation of the ABCs. Because pulmonary complaints predominate, pay attention to respiratory effort, monitor oxygenation, and evaluate for evidence of respiratory failure.
Provide supplemental oxygen for all patients. Patients with impending or obvious respiratory failure should have ventilatory assistance with BVM and high-flow oxygen. Patients with respiratory failure should be intubated and placed on ventilator control.
Perform pulse oximetry. Hypoxemic patients and those with evidence of respiratory failure should have arterial blood gas determination. With the possibility of cardiac involvement, cardiac monitoring is generally indicated. Consider intravenous access and administration of fluid boluses to patients with evidence of volume depletion.
Because patients with sarcoidosis may have taken long courses of steroids, consider alteration in glucose metabolism and the possibility of secondary adrenal insufficiency. Blood glucose determination, urinalysis, and serum chemistries may be indicated.
Sarcoidosis generally is treated with steroids, but this is not endorsed by all physicians. The dosage and duration of treatment varies among institutions and studies; the prognosis of sarcoidosis is difficult to determine, because the course of the disease varies from one individual to another. However, a consensus exists among most physicians to treat symptomatic patients and patients who show signs of deterioration from baseline. These guidelines are discussed below and are arbitrarily classified into pulmonary and extrapulmonary.
Pulmonary Care
Pulmonary symptoms may vary from dyspnea on exertion to severe respiratory failure. Patients require supplemental oxygen, pulse oximetry, arterial blood gas (ABG) assessment, chest radiography, and intubation when indicated. Note that endotracheal disease is present in 40% of cases in stage I and in 70% of patients in stage II and III. Nevertheless, significant stenosis is uncommon and intubation should not be a problem.
For patients in stage I-III, if the individual is asymptomatic and pulmonary function test (PFT) results are normal, he or she is monitored for a few weeks with radiography and PFTs. If symptoms worsen, steroids are begun.
Patients in stage IV are symptomatic and are treated with steroids. Even though stage IV stands for pulmonary fibrosis, patients taking steroids show improvement, probably because the steroids act on ongoing inflammation.
Other agents, mainly cytotoxic medications, also have been used in the treatment of sarcoidosis; however, success has been variable. Consider a lung transplant if the disease does not respond to standard therapy or the disease is in the end stage.
Review of the patient's medication is mandatory. If the patient is not taking any medications or if the patient's medication dosage was recently changed, starting or restarting the patient on medications is reasonable.
In most cases, when symptoms are severe, 60 mg of prednisone daily is prescribed. In moderate cases, 40-60 mg of prednisone every other day is sufficient, and the drug is tapered by 5 mg per month after 6 months. Many patients are treated with a maintenance dose of 20 mg.
Ruling out other pulmonary pathologies, such as pneumonia (eg, bacterial, fungal, Pneumocystis jiroveci pneumonia [PCP]), heart failure, or pulmonary hypertension, is mandatory. [16]
Extrapulmonary Care
Cardiac care
Cardiac involvement in sarcoidosis can manifest as conduction disease, arrhythmia, and/or heart failure. [17] Standard treatment is indicated. Holter monitoring is indicated in the outpatient setting. Central nervous system (CNS) or peripheral neuropathy is treated with systemic steroids.
Patients may present with chronic heart failure (diuretics and/or inotropics are the mainstays of therapy) or arrhythmias (eg, bundle-branch blocks, atrioventricular [AV] blocks). Electrocardiography, chest radiography, and telemetry are indicated. Cardiac manifestations are treated in the usual fashion with diuretics and inotropics, as indicated.
Ocular care
The eye is commonly involved in sarcoidosis. A slit lamp examination and/or ophthalmologic consultation are mandatory. The primary aims for treatment of ocular sarcoidosis are to restore vision and to prevent complications. The mainstay of treatment is topical, regional, and systemic corticosteroid therapy. Systemic immunosuppressive agents are indicated in patients who are dependent on or intolerant of corticosteroids. [6]
Neurologic care
Patients who have CNS involvement may present with any of the following:
-
Cranial nerve symptoms (eg, VII, IX, X)
-
Evidence of optic chiasm involvement (eg, papilledema, blurred vision)
-
Meningeal symptoms caused by aseptic meningitis (requires a lumbar puncture [LP] for confirmation)
-
Symptoms of stroke/transient ischemic attack
-
Decreased deep tendon reflexes
-
Paresthesias (caused by peripheral neuropathies)
Computed tomography (CT) scanning of the head, magnetic resonance imaging (MRI), and neurologic consultation are appropriate. Once it is established that neurologic symptoms are secondary to sarcoidosis, systemic steroids are started.
Hypercalcemia treatment
Hypercalcemia is generally responsive to intravenous hydration. If this is not sufficient or electrocardiographic manifestations are present, systemic steroids are indicated. In the outpatient setting, a decrease in sunlight exposure and, sometimes, treatment with ketoconazole (decreases 1,25-dihydroxyvitamin D) are helpful in minimizing hypercalcemia and hypercalciuria.
Additional therapies
Skin manifestations are treated with topical or systemic steroids. Methotrexate and retinoids are used occasionally. A dermatologic consultation is suggested. Arthritis generally is treated with nonsteroidal anti-inflammatory drugs (NSAIDs). Steroids and occasionally colchicine are reserved for severe cases. Asymptomatic elevation of liver function test results does not require treatment.
Oral proton pump inhibitors (PPIs) are administered to treat GI symptoms (ie, epigastric pain, abdominal fullness, early satiety); more aggressive interventions, such as blood transfusions and pyloric stenosis dilatation or hemostatic intervention, may be needed to treat GI bleeding. [7]
Inpatient Care
Prednisone is an oral steroid and the mainstay of medical treatment. Base dosage on the patient's symptoms.
Patients with severe pulmonary and/or extrapulmonary symptoms must be admitted to the hospital. When failure of steroid treatment and progression of disease is evident, other empiric treatments, such as cytotoxics (eg, methotrexate) are tried. Lung transplantation is an option when the patient's condition is refractory to medical therapy and end-stage pulmonary failure is present. However, cases of new-onset sarcoidosis in transplanted lungs have been documented.
Prednisone treatment is instituted, as discussed earlier. Admitting the patient to the intensive care unit (ICU) is prudent if symptoms are refractory to treatment, if multiorgan involvement occurs because of concomitant failure, or if infection is present.
In the hospital, patients may benefit from pulmonary physical therapy (PT). This decision must be made in conjunction with the PT department. PT can involve the following:
-
Energy conservation
-
Incentive spirometry
-
Segmental breathing exercises
-
Demonstration of positions to relieve breathlessness
-
Interval exercise training to improve aerobic capacity
Transfer, Consultations, and Follow-Up
Transfer
Consider transfer to a specialized center for patients who are not responding to standard therapy or if lung transplantation is entertained. Before transfer, ensure that the patient has stable vital signs and a good or acceptable oxygen saturation level, electrocardiogram (ECG) findings, and mental status.
Consultations
Consider consultations with other services, such as pulmonology, neurology, dermatology, ophthalmology, gastroenterology, and rheumatology, for all patients, except those with minimal findings. Patients considered for discharge should meet with a specialist in managing sarcoidosis for appropriate follow-up treatment.
Follow-up
Emphasize the need for follow-up treatment. Explain the complications and symptoms that require immediate medical attention. Discuss compliance with medications and medical follow-up.
-
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
-
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
-
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
-
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
-
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
-
Stage II sarcoidosis. Courtesy of Anthony Notino, MD, New York Hospital, Department of Radiology, Cornell Medical Center.
Tables
What would you like to print?
- Practice Essentials
- Patient History
- Physical Examination
- Differential Diagnosis
- Laboratory Studies
- Imaging Studies
- Bronchoalveolar Lavage
- Additional Tests
- Prehospital Care
- Emergency Department Care
- Pulmonary Care
- Extrapulmonary Care
- Inpatient Care
- Transfer, Consultations, and Follow-Up
- Show All
- Media Gallery
- References







