Practice Essentials
Congenital nevi are present at birth and result from a proliferation of benign melanocytes in the dermis, epidermis, or both (see the image below). [1] Occasionally, nevi that are not present at birth but are histologically identical to congenital nevi may develop during the first 2 years of life. This is referred to as congenital nevus tardive. [2]
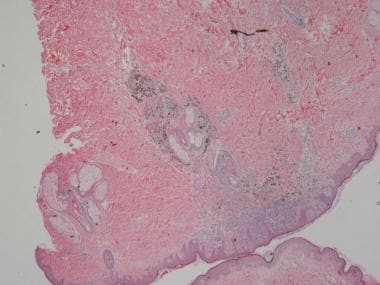 The photomicrograph shows a symmetrical broad proliferation of melanocytes in the papillary and reticular dermis with maturation with progressive descent; splaying between collagen bundles; and permeation of muscles of hair erection, blood vessels, and adnexa (hematoxylin and eosin stain, 20X magnification).
The photomicrograph shows a symmetrical broad proliferation of melanocytes in the papillary and reticular dermis with maturation with progressive descent; splaying between collagen bundles; and permeation of muscles of hair erection, blood vessels, and adnexa (hematoxylin and eosin stain, 20X magnification).
Symptoms
The presence of congenital nevi may be reported by adults, adolescents, or the parents of infants and children.
Nevi may be located anywhere on the body. Classification as a congenital nevus depends in large part on an accurate history or photographs or medical reports from birth.
Scalp nevi in children younger than 18 years old tend to have perifollicular hypopigmentation that creates the appearance of scalloped, irregular borders if occurring on the periphery, or variegation in pigmentation, if occurring within the nevi. [3]
Congenital melanocytic nevi affecting acral volar skin in children are larger, more asymmetrical, and commalike compared with their acquired counterpart. [4]
Also see Complications.
Diagnostics
Biopsy confirms a benign or malignant nature in suggestive lesions.
In cases associated with a high index of suspicion for the presence of neurocutaneous melanosis, magnetic resonance imaging of the central nervous system is a useful diagnostic tool. The presence of a large congenital melanocytic nevus in an infant should prompt magnetic resonance imaging testing before age 4 months if it is in a posterior midline location or is associated with multiple satellite nevi. [5]
Congenital melanocytic nevi rarely involve underlying bones and the maxillary sinus. Such a tumor was documented by magnetic resonance imaging, scintigraphy, and histopathology. [6]
A review of dermoscopy patterns in congenital nevi found that most nevi demonstrate a reticular, globular, or reticuloglobular pattern. The findings varied with age and the anatomic location of the nevus, with the globular pattern found more often in younger children and the reticular pattern found in patients aged 12 years or older. [7] Congenital and congenital-type nail matrix nevi may have clinical and dermoscopic features resembling adulthood subungual melanoma. [8] However, a distal fibrillar ("brush-like") pattern may suggest congenital and congenital-type nail matrix nevi. Although valuable in melanoma, genetic testing of congenital melanocytic nevi is probably unnecessary. [9]
Also see Histologic Findings.
Management
See Treatment for a full discussion.
The management of congenital melanocytic nevi depends on a number of factors, including the size of the lesion, the location of the lesion, the age of patient, the effect on cosmesis, and the potential for malignant transformation.
Although the risk of malignant transformation in small and medium-sized congenital melanocytic nevi has not been established, many physicians agree that the risk is probably not significant enough to warrant the prophylactic removal of all of these lesions. However, some patients may desire removal of these lesions to improve cosmesis. [10] Until evidence is presented on which to base definitive treatment guidelines, many physicians are managing small and medium-sized congenital melanocytic nevi with baseline photography and regular follow-up, with frequency dependent upon the clinician's experience and practice. [11]
Background
Congenital melanocytic nevi are one of several known risk factors for the eventual development of melanoma. Fortunately, melanoma remains an uncommon malignancy in prepubertal children, with an annual incidence of 0.7 cases per million children aged 0-9 years. Patient concerns regarding changing or worrisome-looking nevi are, nonetheless, very common. Moreover, by the time a child reaches adolescence, the incidence of melanoma increases substantially, with a rate of 13.2 cases per million children aged 15-19 years. [12] These melanoma metastasize and are thus life-threatening. [13]
While many sources have noted the so-called melanoma epidemic in adults, only in recent years have data documented an alarming increase in melanoma in adolescents. This increase, combined with the recognition of clearly identifiable melanoma risk factors in childhood, allows physicians of the 21st century to play a crucial role in the identification of children at risk for melanoma and to aid in the prevention of melanoma through education regarding the risks of ultraviolet light exposure.
Congenital melanocytic nevus can be divided into two types, the first being the most common, usually a solitary plaque growing in proportion to that of the child, and a second type composed of many lesions, at least one being large and surrounded by many others and sometimes involving bone and central nervous system. [14]
Pathophysiology
The etiology of congenital melanocytic nevi remains unclear. The melanocytes of the skin originate in the neuroectoderm, although the specific cell type from which they derive remains unknown. [15, 16, 17] One hypothesis is that pluripotential nerve sheath precursor cells migrate from the neural crest to the skin along paraspinal ganglia and peripheral nerve sheaths and differentiate into melanocytes upon reaching the skin. [18] One possible explanation for the presence of congenital melanocytic nevi is that an external insult results in a mutation that affects the morphogenesis of the embryonic neuroectoderm and migration of precursor cells to the skin. Multiple congenital melanocytic nevi may reflect a mosaic RASopathy, reflecting postzygotic activating mutations in NRAS. [19]
One study found that the MC1R (melanocortin-1-receptor) genotype, which corresponds to a red-haired genotype and a tendency to increased birthweight, was overrepresented in a cohort of congenital melanocytic nevi affected Northern European patients. How MC1R variants promote growth of congenital melanocytic nevi and the fetus itself is unknown as is the application of this finding to non-European and more darkly pigmented races. [20]
Congenital nevi have been stratified into 3 groups according to size. Small nevi are less than 1.5 cm in greatest diameter, medium nevi are 1.5-19.9 cm in greatest diameter, and large or giant nevi are greater than 20 cm in greatest diameter. Giant nevi are often surrounded by several smaller satellite nevi. An alternate definition is that a small congenital nevus is one for which primary closure is possible after excision. A single-center, consecutive study of 152 patients with giant nevi delineated malignant transformation in 7 of them: 4 melanomas, 2 rhabdomyosarcomas, and 1 malignant peripheral nerve sheath tumor. [21]
Congenital nevi may also be seen as a component of neurocutaneous melanosis, a rare congenital syndrome characterized by the presence of congenital melanocytic nevi and melanotic neoplasms of the central nervous system. Rokitansky first described neurocutaneous melanosis in 1861. [22] The current diagnostic criteria for neurocutaneous melanosis are (1) large (>20 cm) or multiple (>3) congenital nevi in association with meningeal melanosis or melanoma, (2) no evidence of meningeal melanoma except in patients in whom cutaneous lesions are histologically benign, and (3) no evidence of cutaneous melanoma except in patients in whom meningeal lesions are histologically benign. [23]
Neurocutaneous melanosis may result from an error in the morphogenesis of the neuroectoderm, which gives rise to the melanotic cells of both the skin and meninges. Clinically, patients may present with increased intracranial pressure due to hydrocephalus or a mass lesion. The prognosis of patients with symptomatic neurocutaneous melanosis is very poor, even in the absence of malignancy. In one review of 39 reported cases of symptomatic neurocutaneous melanosis, death occurred in more than half the patients within 3 years of the onset of neurological symptoms, and most deaths were in patients younger than 10 years. [23]
Mutations in NRAS in congenital melanocytic nevi can cause mitogen-activated protein kinase activation and may represent early events in melanoma development. [24]
Oncogenic missense mutations in codon 61 of NRAS were found in affected neurological and cutaneous tissues in 12 of 15 patients with congenital melanocytic nevi with neurocutaneous melanosis, implying single postzygotic NRAS mutations were responsible. [25] However, the higher risk of a large or giant congenital melanocytic nevus becoming malignant compared with common acquired nevi is not explained by the presence of mutations in MAPK pathway genes. [26]
Etiology
The etiology of congenital melanocytic nevi has not been elucidated. One possible cause is a mutation due to an external insult. [27] An association between infantile hemangiomas and congenital melanocytic nevi has been suggested. [28] Future investigation may yield more definitive causative factors.
Epidemiology
Frequency
Congenital nevi are present in 1-2% of newborn infants. One small study in Spain found a higher prevalence of congenital melanocytic nevi in preterm infants, females, and nonwhite infants, whereas maternal age, number of previous pregnancies, and birth weight did not appear to influence the prevalence. [29]
Race-, sex-, and age-related information
No racial predilection is recognized for congenital nevi.
Congenital nevi occur in both sexes, with no known predilection.
To be considered congenital nevi, lesions must be present at birth.
Prognosis
The prognosis for patients with small or medium-sized congenital melanocytic nevi is good. Although the risk of developing melanoma in these lesions has not been quantified, it is generally regarded as only slightly higher than that of normal skin. Despite the increased risk for melanoma in patients with giant congenital melanocytic nevi, the vast majority of patients never develop melanoma. Therefore, prognosis remains good in these patients, especially if the lesions are examined regularly for signs of atypia.
Prognosis in cases of symptomatic neurocutaneous melanosis is quite poor.
Mortality/morbidity
Congenital nevi, depending on size and location, may have a significant impact on cosmesis. Giant congenital nevi place individuals at an increased risk for the development of melanoma at the site of the nevus. For giant congenital melanocytic nevi, the risk of developing melanoma has been reported to be as high as 5-7% by age 60 years. [30, 31] One study suggests that the risk of melanoma may be greater in those with giant congenital melanocytic nevi with more satellite lesions or a larger diameter, [32] although it is unlikely to be so high. [33] Another suggests multiple satellite nevi alone or with associated posterior midline location of large congenital melanocytic nevi is linked with increased risk. [5] Additionally, melanoma developing within giant congenital nevi may develop during childhood and occur deeper in the tissue where it is harder to detect clinically.
While the general consensus regarding smaller nevi is that they pose a greater risk for the development of melanoma than normal skin, this risk has not been quantified. Also suggested is that melanoma developing within smaller congenital nevi usually occurs at puberty or later and develops more superficially in the skin, where it is easier to detect clinically.
Patient Education
All people need to be educated on the importance of protection from ultraviolet light exposure. This is especially important in people who have congenital melanocytic nevi, particularly the giant type, because they are already at an increased risk for the development of melanoma.
-
The photomicrograph shows a symmetrical broad proliferation of melanocytes in the papillary and reticular dermis with maturation with progressive descent; splaying between collagen bundles; and permeation of muscles of hair erection, blood vessels, and adnexa (hematoxylin and eosin stain, 20X magnification).
-
Higher-power view of the previous image (hematoxylin and eosin stain, 40X magnification).







