Practice Essentials
Malakoplakia is a rare granulomatous disease of infectious etiology that involves the skin and other organs. [1, 2] Malakoplakia is most frequently reported to occur in the genitourinary system. The first case of malakoplakia reported to occur outside the genitourinary system was in 1958. [4] Since then, various organs have been reported to be affected.
Malakoplakia is usually reported in the setting of immunocompromise, although rare reports in immunocompetent individuals have been documented.
Malakoplakia presents clinically with a wide spectrum of findings, and the criterion standard for diagnosis is pathological examination.
Signs and symptoms
Also see History.
Malakoplakia lesions may present as erythematous papules, subcutaneous nodules, draining abscesses, ulcers, nonhealing surgical wounds, indurated plaque, or draining fistulas. [35, 36, 37, 38]
Malakoplakia was also reported masquerading as pyoderma gangrenosum, presenting as a nonhealing malleolar ulcer for 2 years. [39] The most common site affected in the reported cases was perianal (19%). Other affected sites included the abdomen, face, neck, and vulva. [40] In one study, perianal and inguinal skin, vulva, and scrotum were affected in 41% of patients with cutaneous malakoplakia, followed by abdominal wall, thorax, and head and neck at 20% and by extremities and axilla at 10%. [41]
The most common presentation in reported cases of cutaneous malakoplakia is nodules (23%), with about one quarter of these lesions complicated by abscess or ulcer formation.
Rarely, malakoplakia involves more than one anatomical site in the same patient. [42]
Duration varies from weeks to months and, rarely, years.
Complications include local disfigurement and organ dysfunction with visceral involvement.
Diagnostics
Please see Workup.
Management
Also see Treatment.
Excision of skin lesions and drainage of abscesses are fundamental to diagnosis and treatment. Surgery combined with antibiotic therapy should be directed against E coli or other organisms recovered on culture.
Background
The name is derived from the Greek malakos (soft) and plakos (plaque), describing its usual clinical presentation as friable yellow soft plaques.
It was first described by von Hansemann in 1901 and in 1902 by Michaelis and Gutmann. [3]
Cutaneous malakoplakia is rare and was first reported in 1972 by Leclerc and Bernier. [5]
Pathophysiology
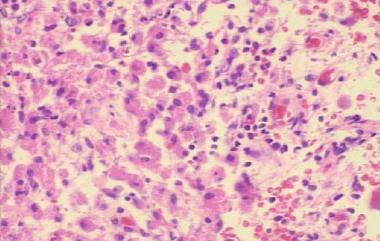
Malakoplakia is believed to result from the inadequate killing of bacteria by macrophages or monocytes that exhibit defective phagolysosomal activity. Partially digested bacteria accumulate in monocytes or macrophages and lead to the deposition of calcium and iron on residual bacterial glycolipid. The presence of the resulting basophilic inclusion structure, the Michaelis-Gutmann body, is considered pathognomonic for malakoplakia. See the image below.
Studies have suggested that a decreased intracellular cyclic guanosine monophosphate (cGMP) level may interfere with adequate microtubular function and lysosomal activity, leading to an incomplete elimination of bacteria from macrophages and monocytes.
The incidence of malakoplakia in immunocompromised states, including post organ transplantation, diabetes mellitus, AIDS, malignancy, and immunosuppressive therapy, suggests that a disturbed function of T lymphocytes may play a role in the pathogenesis of malakoplakia in patients in states of immunocompromise. [3]
Etiology
The most common organism isolated was Escherichia coli. Other organisms isolated include Klebsiella and Proteus species. Although E coli is the most common gram-negative bacterium isolated, other enteric bacteria may be found on culture. Staphylococcus aureus,Pseudomonas aeruginosa, and Rhodococcus equi may also be cultured. [6]
Defective macrophage killing of these bacteria leads to malakoplakia. Defective macrophage killing results in an accumulation of bacterial degradation products and a granulomatous reaction, which clinically manifests as the formation of a papule, a plaque, or an ulceration.
Risk factors for the development of malakoplakia include the following [7, 8, 9, 10] :
-
Immunosuppressive therapy after organ transplantation
-
Malignant lymphoma on chemotherapy
-
Myelodysplastic syndrome
-
Post radiotherapy
-
Diabetes mellitus
-
Alcoholism
-
Rheumatoid arthritis
-
Dermatomyositis
-
Lupus vulgaris
-
Carcinoma of the breast post mastectomy
-
Concomitant urinary tract infection
-
Prolonged therapy with systemic corticosteroids
Other rare associations that have been reported include papillary urothelial carcinoma [11] and abdominal malakoplakia following blunt trauma to the abdomen. [12]
Epidemiology
Frequency
The total number of patients with malakoplakia is fewer than 500. Most patients have genitourinary tract disease, although involvement of the gastrointestinal tract and other visceral organs has been described. Cutaneous malakoplakia is rare, with fewer than 60 cases reported in the literature. Because this disease is often diagnosed after biopsy of nondescript lesions, the true incidence is most likely higher.
Race
Cutaneous malakoplakia is more commonly reported in Whites (39%) than in Blacks (19%) or Asians (12%), although the patient's ethnic group is often not specified in case reports.
Sex
Cutaneous malakoplakia occurs with a male-to-female ratio of 2.3:1.
Age
Cutaneous malakoplakia presents in patients with a broad age range. The median age at the time of presentation is 53 years. Occurrence of the disease is associated more with the presence of an immunocompromised state affecting monocyte and macrophage function than with age.
Prognosis
Malakoplakia most often occurs in patients who are immunocompromised. Often, malakoplakia is resistant to treatment, with a mean duration of the skin lesions of 3-6 months. Malakoplakia shows a variable course and, in rare cases, can be fatal. [4] Mortality in patients with malakoplakia is most often due to an underlying condition.
Cutaneous lesions usually follow a benign clinical course. The cure rate following surgery with or without antibiotics is about 80%. [13, 14]
Significant morbidity relates to the chronicity of the condition, which can resist local and systemic therapy. Draining sinuses, persistence of disfiguring skin lesions, and involvement of visceral organs constitute significant morbidity in patients with malakoplakia.
Patient Education
Instruct patients who are immunosuppressed, who have undergone organ transplantation, or who are receiving systemic corticosteroids to notify the physician if they notice a fleshy mass that is growing slowly and ulcerating.
-
Cutaneous malakoplakia.
-
Michaelis-Gutmann body in a patient with malakoplakia.