Practice Essentials
Oral melanoacanthoma is a rare, reactive, mucosal lesion, which, similar to cutaneous melanoacanthoma, is associated with hyperplasia of spinous keratinocytes and melanocytes. [1] Its most common intraoral sites are the buccal mucosa, lip, palate, and gingiva. [2, 3, 4, 5] Melanocytes occur throughout the oral mucosa, but they have a relatively low level of pigment production and may go unrecognized. [6] The average age at presentation is 28 years, and it occurs mainly in Blacks, with a strong female predilection. [7] Oral melanoacanthoma is unrelated to seborrheic keratosis. Oral melanoacanthoma is most often seen as an enlarging flat or slightly raised area of hyperpigmentation on the buccal mucosa of adult black women. Strong homatropine methylbromide reactivity has been described, limiting its utility in distinguishing oral melanoacanthoma from malignant melanoma. Laugier-Hunziker syndrome, also known as idiopathic lenticular mucocutaneous hyperpigmentation, displays progressive mucosal pigmentation. It has been described with multiple metachronous oral melanoacanthomas. [8]
Although melanoacanthoma can be found both on the skin and oral mucosa, the focus of this review is cutaneous melanoacanthoma. Although most authors consider cutaneous melanoacanthoma a benign tumor of melanocytes and keratinocytes, some have suggested it may be a reactive phenomenon induced by localized trauma. [9]
Signs and symptoms
History
Cutaneous melanoacanthomas are painless and slow growing. The slow but persistent growth and related cosmetic problems with melanoacanthomas may prompt an affected individual to consult a physician.
Patients are generally asymptomatic; however, trauma or manipulation of the melanoacanthoma may lead to bleeding or inflammation. Patients may live with cutaneous melanoacanthoma for decades before they seek treatment.
Oral melanoacanthoma is rare, first noted with the sudden appearance and rapid growth of a brown-black macule. [10] Gingival melanoacanthomas may be evident as solitary or multiple. [11] Oral melanoacanthoma may be bilateral. [12] It may rarely appear on the gingiva. [13] Its appearance on the nipple of a middle-aged woman caused consternation. [14]
Physical examination
Melanoacanthomas are most often solitary. Multiple melanoacanthomas have been described. In one case, a 40-year-old man had multiple, minute, discrete or confluent shiny papules limited to his left upper eyelid. [15] They may rarely appear as multiple, asymptomatic, slowly growing, raised pigmented nodules and tumors scattered all over the body. [16] An ulcerating tumor has been described in one of the lesions.
Cutaneous melanoacanthomas are found mainly on the trunk or head, often on the lip or eyelid. The rare conjunctival melanoacanthoma may appear as a painless, solitary, pigmented conjunctival nodule. [17]
They have also been observed on the penile shaft [18] and in the genital regions as a large, solitary, slowly enlarging, hyperpigmented verrucous tumor with a cerebriform surface. [19]
Cutaneous melanoacanthomas may be hyperpigmented or verrucous and round or oval. The lesion may be a papule, plaque, cutaneous horn, or nodule. Lesional diameters range from a few millimeters to 10 cm. Note the image below.
The authors have observed a darkly pigmented cutaneous horn that extended from the left upper eyelid to below the lower eyelid in a 45-year-old man; the lesion had histologic findings consistent with melanoacanthoma (see image above).
Melanoacanthomas can occur on the oral mucosa, [20] but oral lesions are distinct from cutaneous melanoacanthomas. [7, 21]
Diagnostics
Neither laboratory nor imaging studies are required for melanoacanthomas.
Simple shave biopsy or excision, depending on the site of the melanoacanthoma, may be performed for diagnostic purposes. Because the lesions are epidermal and superficial, excision of the dermis and subcutis underlying a melanoacanthoma is not required or recommended.
Dermatoscopic features have been described, [22] including comedolike openings, fat fingers, and irregularly distributed dots. Comparison of these features between melanoacanthomas and melanoacanthomalike melanomas showed they may overlap clinically in appearance and on dermoscopy. [23] It is among the most frequent benign tumors that may have dermatoscopic characteristics suggestive of malignancy. [24] Reflectance confocal microscopy evaluation of melanoacanthoma may show features suggestive of a nodular melanoma, [25] with dendritic pagetoid cells. [26]
Microscopic examination of cutaneous melanoacanthoma reveals a benign acanthoma composed of keratinocytes and dendritic melanocytes. Acanthosis, hyperkeratosis, parakeratosis, papillomatosis, and small horn pearls may be seen. Large dendritic melanocytes with abundant melanin granules are spread throughout the lesion. Note the image below.
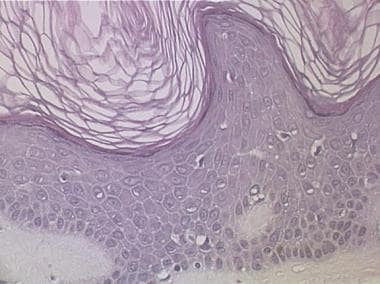 Photomicrograph of cutaneous melanoacanthoma. Large polydendritic melanocytes are seen at all levels of the epidermis. Acanthosis, hyperkeratosis, and slight papillomatosis are also present (hematoxylin and eosin stain, original magnification X139).
Photomicrograph of cutaneous melanoacanthoma. Large polydendritic melanocytes are seen at all levels of the epidermis. Acanthosis, hyperkeratosis, and slight papillomatosis are also present (hematoxylin and eosin stain, original magnification X139).
Cytologic atypia is not a feature of the melanocytes or keratinocytes in a melanoacanthoma. Two types of melanoacanthomas are described: a diffuse type in which melanocytes are unevenly scattered throughout the lesion and a clonal type in which melanocytes and keratinocytes are clustered in small nests. [27]
Electron microscopic studies reveal that the transfer of melanin from these highly dendritic melanocytes to neighboring keratinocytes is either partially or, in some cases, completely disrupted. [28] Immunoprecipitation assays and immunofluorescent studies show that melanoacanthoma is unrelated to malignant melanoma. [29, 30]
Management
Pharmacologic therapies are not available for melanoacanthomas.
Simple excision is curative for melanoacanthomas. Cutaneous melanoacanthoma is benign and may be removed with curettage. However, one theory suggests that cutaneous melanoacanthoma may be self-limited and it resolves without intervention.
Cryotherapy may be used if the diagnosis is certain and if histologic examination is not required. Additionally, argon plasma coagulation is a new treatment option for oral melanoacanthoma. [31]
Scarring can be expected after the surgical or cryotherapeutic removal of a melanoacanthoma.
Standard follow-up care may be needed to assess healing and address cosmetic issues.
A dermatologist should be consulted to confirm the diagnosis of melanoacanthomas.
Background
Melanoacanthoma is a term that Mishima and Pinkus [32] introduced in 1960 to describe a pigmented, benign proliferation of both keratinocytes and dendritic melanocytes. Prior to this designation, Bloch [33] described a similar lesion in 1927 that he called melanoepithelioma type I. Melanoepithelioma type II is an ordinary pigmented seborrheic keratosis.
Etiology
The cause of melanoacanthoma is unknown, but most instances appear to represent a benign neoplasm. Irritation or trauma to the skin may cause some cutaneous melanoacanthomas, especially on the lips. Trauma and irritation of the oral mucosa are believed to cause oral melanoacanthoma. A gingival melanoacanthoma was believed to be caused by teeth-whitening strips. [34]
Epidemiology
Frequency
United States
Cutaneous melanoacanthoma is generally regarded as rare. Melanoacanthoma was the primary diagnosis in 5 of 500,000 consecutive skin biopsy samples in one series from the United States. [27]
International
In their series of 189 consecutive seborrheic keratoses diagnosed among Spanish patients, Simon et al [35] found that cutaneous melanoacanthoma represented 28% of all seborrheic keratoses. A Korean survey of seborrheic keratoses classified 9.2% of 271 as melanoacanthomas. [36]
Race-, sex-, and age-related information
Cutaneous melanoacanthoma is described more frequently in White patients than in others. However, the lesion is rare in all ethnic groups.
Cutaneous melanoacanthoma develops in males and females with the same frequency.
Cutaneous melanoacanthoma develops in middle-aged and elderly people. Melanoacanthoma has been described in patients aged 46-81 years, with an average age of 55-65 years. [27, 18]
Prognosis
Melanoacanthoma is benign. Removal of cutaneous melanoacanthoma is curative.
Morbidity with melanoacanthoma is uncommon. However, a melanoacanthoma that extends from the upper eyelid to beyond the lower eyelid can obstruct the patient's vision. The authors have observed this complication. Melanoacanthomas may be as large as 10 cm in diameter and can therefore be unappealing to the patient. [37]
Patient Education
Patients should be informed that cutaneous melanoacanthoma is benign and has no potential for malignant transformation. Cutaneous melanoacanthoma is not associated with any skin or visceral cancer; it is not an indicator of cancer, and its presence is not a risk factor for cancer.
-
Large cutaneous melanoacanthoma in a 45-year-old man that obstructs his vision.
-
Photomicrograph of cutaneous melanoacanthoma. Large polydendritic melanocytes are seen at all levels of the epidermis. Acanthosis, hyperkeratosis, and slight papillomatosis are also present (hematoxylin and eosin stain, original magnification X139).










