Overview
A postoperative complication may be defined as any negative outcome perceived either by the surgeon or by the patient. It may occur intraoperatively, in the immediate postoperative period, or later on, as the effects of tissue remodeling and scarring become apparent in an unacceptable aesthetic or functional result. These processes are largely interrelated, and they represent a complex interplay of factors along a continuous spectrum.
Complications must be anticipated, and preventive actions must be taken in every surgical case. Early recognition with prompt appropriate intervention is the best way to avert progression to a potentially disastrous situation. Patient education and close follow-up care are also requisite. The complications addressed in this article are those related to the use of a scalpel, otherwise known as cold-steel surgical procedures.
For patient education resources, visit the Skin Conditions and Beauty Center. Also, see the patient education articles Bruises and Suture Care.
Prevention of Complications
Preoperative evaluation
Surgical complications must be anticipated and addressed as soon as surgical treatment is determined to be necessary, usually during the preoperative consultation. Appropriate patient selection involves the detection of both physical and psychiatric conditions, which may interfere with a desirable outcome.
The physician (or nurse) can evaluate the patient's insight, his or her expectations (ie, are they realistic?), and his or her ability to provide informed consent through verbal and nonverbal cues during the initial encounter. One must consider the impact of concomitant neurologic or psychiatric illness, such as dementia, untreated depression, mania, psychosis, or an anxiety disorder. The patient's desire for education (ie, whether they do or do not wish to know details of the procedure) will also become apparent during the evaluation.
Psychosocial issues also have a role in planning treatment and follow-up care. For example, an elderly patient living alone may prefer a primary repair over healing by second intention for an anticipated wound in a difficult-to-reach area. A patient from an outlying area may choose the treatment that requires the least amount of follow-up care.
Including patients in the decision-making process by providing options and by inviting them to become an active participant in their health care is important. Listening to patients and addressing their concerns are critical. The author has found that having the patient look at the area to be treated as the surgeon demonstrates the proposed procedure and indicates possible defects, scar sizes and locations, as well as anticipated areas of edema and ecchymosis is valuable. Prior to surgery, discussing the procedure and possible defects is also prudent to verify that both the patient and the doctor agree on the area to be treated. Communicating and cross-referencing beforehand cannot be overemphasized. If a difference in opinion exists, it may be discussed at this time.
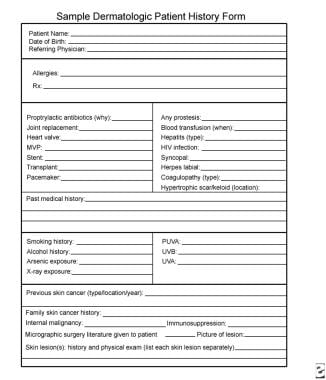
Medical risk factors are identified during the initial patient encounter. An effective strategy is to combine the use of a questionnaire form, which may be reviewed by the physician, and direct questioning to clarify and confirm identified risks. See the image below.
Risk factors for intraoperative and postoperative bleeding include both medication use (eg, aspirin, warfarin, novel oral anticoagulants, herbal remedies, vitamins) and active medical problems (eg, blood dyscrasias, liver or kidney disease). Allergies to medications, anesthetics, topical antibiotics, latex, and bandage adhesives need to be ascertained. Immunosuppression, whether related to underlying disease or secondary to medication, should be recognized. Tobacco and heavy alcohol use may affect wound healing and hemostasis. [1]
Viral illness, such as recurrent herpes labialis, may require prophylactic treatment for a procedure in the perioral region. Other conditions, such as irradiated skin, Ehlers-Danlos syndrome, and use of colchicine, portend poor wound healing. Cardiac valve disease, recent cardiac stenting, or internal prosthetic placement may require preoperative antibiotics. The presence of a pacemaker/defibrillator may require that bipolar electrocautery be used. Other medical conditions that may pose additional risks include a seizure disorder, cardiac disease, supplemental oxygen use, active viral or bacterial infection, and syncope. On the day of surgery, a brief review of the patient's medical status and a review of systems serve to identify other potential problems which may not have been evident at the time of preoperative counseling.
Proper surgical technique
Perhaps the single most important contribution the dermatologic surgeon can make to ensure a desirable outcome is to adhere to proper surgical technique. At the time of surgery, the patient's evaluation should be reviewed, and the patient's vital signs should be taken. A strategy should be planned to accommodate for risk factors that were previously identified. Anesthesia should be used diligently; the quantity should be adequate, not toxic (for lidocaine in adults: < 4.5 mg/kg without epinephrine, < 7 mg/kg with epinephrine). The patient should be asked to report any discomfort.
Strict aseptic technique and universal precautions are mandatory; hair should be secure, and a face mask, eye protection, scrubs, gloves, and gown should be worn, if necessary. Proper patient positioning is required for accessibility and immobility. Skin should be widely prepared with chlorhexidine or povidone-iodine solution. Chlorhexidine should be avoided near the eyes and ears to prevent ocular and ototoxicity, and caution should be used as well with povidone-iodine in the periorbital area to prevent corneal irritation. [2] The patient is then properly draped. The patient's eyes should be protected when operating on the head or the neck. In other cases, patients should be instructed to turn their head away from the area being treated to prevent airborne contamination. A controlled environment is created by limiting personnel traffic in the operating suite. Proper and accessible instrumentation as well as good lighting are requisite to ensure smooth operation. Knowledge of anatomical danger zones prevents inadvertent transection of vital structures.
Because most dermatologic surgical procedures are performed under local anesthesia alone without sedation, taking measures to decrease the patient's anxiety is important. Speaking to the patient and engaging in conversation, if appropriate, are helpful. One should always maintain a calm speaking voice. Music in the operating suite also serves to distract and relax the patient. If operating alone, assistance must be within range; calling out loudly for help will surely unnerve the patient. The surgeon should prepare the patient by calmly explaining any situation that arises. Most importantly, one should be prepared. The dermatologic surgeon should anticipate the unexpected at each and every step of the procedure.
Also see Basic Excisional Surgery.
Postoperative care and follow-up care
Postoperatively, patients should be prepared to follow wound care instructions and to watch for warning signs of complications. Instructions should be provided in both verbal and written forms. Patients should be informed of the expected appearance of edema and ecchymosis in areas seemingly distant to the operative site. For example, periorbital edema and ecchymosis are frequent sequelae of surgical procedures performed on the forehead, but they may be unexpected and alarming to the patient if he or she is not appropriately warned. Similarly, surgery on the cheek may result in ecchymosis appearing on the neck, or even intra-orally, due to tracking of blood in naturally occurring tissue planes (see the images below).
Close follow-up care is needed to ensure the early identification of possible complications. Patients should be instructed to report bleeding, excessive pain, fever, discharge, and trauma to the operative site. When a complication arises, early intervention is of paramount importance, and both the patient and the staff should be educated in this regard.
Bleeding Complications
Bleeding is one of the most common complications in dermatologic surgery. Bleeding from the smaller caliber vessels encountered in cutaneous surgery is unlikely to pose a life-threatening immediate risk; however, it is alarming to the patient and threatens the integrity of the surgical repair. Postoperative bleeding may eventuate in the terrible tetrad of hematoma, infection, dehiscence, and necrosis. A normal hemostatic response to vascular injury involves the initial formation of a platelet plug followed by a fibrin-platelet clot, and this process depends on the adequate quantity and function of coagulation factors and platelets. A medication or diseased state that affects any step in this coagulation cascade has the potential to cause bleeding. Additionally, inadequate hemostasis during surgery and mechanical factors, such as hypertension and trauma, can cause bleeding complications.
The most commonly used medications known to affect hemostasis include warfarin, aspirin, other nonsteroidal anti-inflammatory drugs (NSAIDs), and antiplatelet agents. Warfarin inhibits the production of the vitamin K–dependent coagulation proteins II, VII, IX, and X to interfere with fibrin clot formation. The peak effects of warfarin anticoagulation are seen at 72-96 hours after administration and may be monitored by measurement of the international normalized ratio (INR) and prothrombin time.
Aspirin irreversibly inhibits cyclo-oxygenase to interfere with platelet aggregation and platelet plug formation. These effects last the lifespan of the platelet (7-10 d) and clinically result in an increased bleeding time. Conventional NSAIDs exert similar, though reversible, inhibition of platelet function via nonspecific cyclo-oxygenase inhibition. The duration of NSAID platelet inhibition depends on the elimination half-life of the particular drug (usually 1-3 d). The newer cyclo-oxygenase-2-specific inhibitors (eg, celecoxib [Celebrex]) have minimal effects on platelet function. [3, 4] Other agents, such as clopidogrel (Plavix) and ticlopidine, inhibit adenosine diphosphate-induced fibrinogen binding, resulting in decreased platelet aggregation. Dabigatran etexilate (Pradaxa) reversibly inhibits thrombin; rivaroxaban (Xarelto) selectively blocks the active site of factor Xa. Alcohol is a potent vasodilator, and its use should be avoided in the perioperative period.
Many patients also use herbal preparations with known anticoagulant properties, which may contribute to bleeding complications. Garlic inhibits platelet aggregation in a dose-dependent manner. Spontaneous epidural hematoma and bleeding during prostatectomy have been reported in association with garlic supplementation. Garlic contains adenosine, allicin, and paraffinic polysulfides, which exhibit antiplatelet effects believed to be irreversible in nature, lasting the lifetime of the platelet (7-10 d). Gingko biloba has been implicated in cases of postoperative and intracranial bleeding. The elimination half-life of 3-10 hours determines the level of antiplatelet activity.
Ginseng inhibits platelet aggregation in a likely irreversible manner, and it has been associated with vaginal bleeding. Feverfew contains sesquiterpene lactone and parthenolide, which inhibit platelet aggregation. Vitamin E is sometimes used in the treatment of ischemic heart disease and stroke, and it has known anticoagulant effects through the inhibition of the vitamin K–dependent coagulation cascade. Many patients do not consider over-the-counter supplements when reporting medication use, and they should be specifically questioned about them.
An increased risk of severe bleeding complications has been demonstrated when warfarin, aspirin, NSAIDs, and antiplatelet agents are used in the context of various types of surgeries, from orthopedic surgery to ophthalmologic surgery. The effects of these medications in association with bleeding complications in dermatologic surgery are less well documented. Several studies focusing on cutaneous surgery fail to demonstrate a significant difference in postoperative bleeding complications in patients who continue anticoagulant medications compared with those who discontinue them in the preoperative period.
Although the use of aspirin, warfarin, and NSAIDs may be associated with increased intraoperative bleeding in dermatologic surgery, whether it results in poorer outcomes is not clear. [5, 6, 7] A blinded, controlled study showed that surgeons were not able to predict a patient's anticoagulant status based on intraoperative observations. [8] Patients on warfarin or clopidogrel have an increased risk of bleeding, with a significant increase in bleeding risk when these medications are combined. [7] However, the bleeding complications were not life-threatening. Dabigatran and rivaroxaban have not been associated with severe bleeding complications when continued in the setting of cutaneous surgery. [9] The decision to stop a medication in the preoperative period involves a thorough, individualized risk-to-benefit analysis.
Most patients can avoid aspirin, NSAIDs, and vitamin supplements preoperatively without ill effects. However, patients taking anticoagulant medication to prevent thromboembolic events should be addressed with caution. In general, the INR decreases to 1.5 or less within 3 days of warfarin discontinuation. Cases of thromboembolic stroke after temporary discontinuation of warfarin and aspirin prior to cutaneous surgery have been reported. [10, 11] The continuation of medically necessary anticoagulant/antiplatelet medication has been found to be safe in the setting of dermatologic surgery. [7] At the present, most dermatologic surgeons routinely continue all medically indicated anticoagulation or antiplatelet agents during cutaneous surgery.
Postoperative bleeding usually arises within the first 24 hours after surgery. Minor postoperative bleeding from wound edges is not uncommon, and it usually results from excessive activity on the patient's part; from trauma to the area of the wound; or from the increase in blood flow, which occurs when the vasoconstrictive effect of epinephrine diminishes. Patients should be forewarned of this occurrence and educated to apply firm, constant pressure (preferably with a cool pack) to the bleeding area for at least 15 minutes. Most postoperative bleeding responds to this simple intervention. A pressure dressing is useful in providing some hemostatic compression, but it mainly provides immobilization and protection from trauma, which could dislodge small clots and result in bleeding.
Significant bleeding that compromises wound integrity requires exploration of the wound to visualize the bleeding vessel. Once identified, the vessels can be ligated or cauterized to achieve hemostasis. Occasionally, drainage may persist from wounds involving large areas of undermining or dead space. Placement of a fenestrated Penrose drain for the first 24 hours after surgery may be helpful prophylactically or in managing wounds that continue to ooze despite other interventions.
Bleeding under the suture line results in hematoma formation, which presents with sudden pain and a tender, often bluish area of swelling at the wound site. A hematoma can have deleterious consequences as it exerts pressure on the wound edges; it may lead to ischemia, tissue necrosis, and dehiscence. The collection of blood is also an excellent medium for bacterial growth and places the wound at increased risk of infection. If discovered in the acute postoperative period (within the first few days), the hematoma is still gel-like and may be expressed from the wound through the suture line or by partial takedown of the repair (see the images below).
A large, expanding hematoma requires immediate removal of the sutures to release the tension on the wound. The hematoma should be removed, followed by lavage with sterile sodium chloride solution. Then, the bleeding vessels can be identified and ligated or cauterized, followed by resuturing of the wound if within 24 hours of surgery, or the wound can be allowed to heal by second intention.
After several days, the hematoma evolves into a more solidified mass, and its removal is more difficult. If discovered at this point, one must assess for the presence of wound compromise to determine if the wound needs to be opened. If the wound does not appear to be compromised, the patient may be treated with a pressure dressing and close follow-up care. Antibiotics should be considered. The natural history of hematomas includes liquefaction, which occurs between 7-14 days. At this point, one may be able to aspirate the hematoma with a large-gauge needle.
Seroma, a collection of serous fluid under the suture line, may occur in areas of extensive undermining or dead space. Seromas may be drained to alleviate pain and tension on the wound by using a large-bore needle and syringe to withdraw the fluid (see the image below).
Infection
The postoperative wound infection rate in dermatologic surgery is low. Reported rates are 0.7-2.29%. Most dermatologic surgical procedures fall into either the clean category or the clean-contaminated category in the classification scheme, which predicts the infection rate as a function of wound contamination.
Clean wounds (class I) imply total adherence to aseptic technique; an uninfected operative wound; and no entry into the respiratory, GI, or genitourinary (GU) tracts. Wounds classified as clean have an expected infection rate of 1-4%.
Clean-contaminated wounds (class II) include wounds in which a minor break in technique has occurred or when a noninfected respiratory, GI, or GU tract has been entered. This category has an expected infection risk of 5-15%.
Class III and IV wounds include grossly contaminated and acutely infected wounds that are generally not encountered in dermatologic surgery.
This classification scheme was devised as a guide to prophylactic antibiotic administration. In general, clean wounds do not require prophylactic antibiotics, clean-contaminated wounds may require them, and contaminated and infected wounds definitely require antibiotic treatment. [12, 13]
When infection does occur, it is usually due to a combination of a lapse in aseptic surgical technique and a lowering of local host immune defenses by interference of blood flow or by causing local inflammation. Shaving the operative site prior to surgery has been shown to increase infection rates. If necessary, hairs should be clipped with scissors to avoid irritation and inflammation at the operative site.
Good surgical technique is indispensable in preserving the integrity of the local immune defense. A well-approximated wound with good hemostasis and little devitalized tissue can resist infection in the presence of higher numbers of bacteria. Excessive manipulation of the wound edges and suture placement that impairs dermal capillary blood flow lead to ischemia, increasing infection risk. Electrocautery results in necrotic tissue, which incites a local immune reaction; excessive use of electrocautery should be avoided. [14] Dead space in the wound and ineffective hemostasis predispose to the development of hematoma and seroma, which provide an ideal growth medium for bacteria and cause tension on wound edges.
Sutures are foreign bodies, and they incite a local immune response, which compromises the local ability to fight infection. The surgeon should choose the smallest adequate caliber suture and needle. Less reactive synthetic suture materials are preferable over natural ones. Studies in mice have demonstrated increased adherence of bacteria to multifilament (braided) subcutaneous sutures when compared with monofilament sutures. [15] This increased bacterial adherence is correlated with higher infection rates when multifilament sutures are used.
Other factors associated with an increased risk of infection include lengthy procedures (2 h or more), inflamed operative sites (eg, ulcerated tumor, irritated lesion, inflamed cyst, reexcision of recent biopsy site), and the presence of drains. Patient characteristics, such as advanced age, immunocompromised state, malnourishment, and obesity, also predispose to infection. Other complications, such as hematoma, seroma, necrosis, and dehiscence, often coexist with an infectious complication. Infections distant to the operative site are associated with an increased risk. Moist body areas, such as the nose, the axillae, the mouth, the ears, and the genitalia, that have high bacterial counts pose a higher risk. Additionally, locations below the knee, wedge excisions of the lip, and ear and skin grafts may have an increased risk of postoperative wound infection. In all of these situations, perioperative antibiotics should be considered for prophylaxis. [16]
Patients at high risk for wound infection or endocarditis should receive prophylactic antibiotics chosen to cover the organism most likely to cause infection. Staphylococcus aureus is the most common etiology of skin wound infections. Streptococcus viridans is a common resident of oral flora, and Escherichia coli is present near the GI and GU tracts. Pseudomonas species are a common pathogen of the external ear. Prophylactic antibiotics should be administered prior to surgery to allow systemic absorption and incorporation into the coagulum, which seals the wound. The coagulum is formed within the first 3 hours of wounding. Recent recommendations in dermatologic literature advise a single dose given 1 hour before surgery. In cases of lengthy procedures or in those involving high-risk areas, a second dose should be given 6 hours after surgery.
Endocarditis prophylaxis is a confusing issue. Dermatologic surgery is not considered in the American Heart Association's published guidelines for endocarditis prophylaxis. [17] Several studies have indicated that the incidence of transient bacteremia during cutaneous surgery is low when procedures are performed on intact skin or on eroded but noninfected skin. Staphylococci and streptococci frequently colonize eroded, noninfected skin (ie, tumors also cause prosthetic valve endocarditis).
The authors do not recommend routine prophylaxis for high-risk patients (as per American Heart Association guidelines for patients with prosthetic cardiac valves, history of bacterial endocarditis, complex cyanotic congenital heart disease, surgically constructed systemic pulmonary shunts, or conduits) undergoing procedures on intact skin of less than 20 minutes duration. In other cases, patients at high risk for endocarditis should receive prophylactic antibiotics (ie, presence of infected skin, breach of oral mucosa or noninfected site at high risk for surgical site infection). [18]
Prophylaxis is not recommended in patients with indwelling cardiac pacemakers, hemodialysis shunts, arterial grafts present less than 1 month, GU prostheses, and breast implants. Prophylaxis should be considered for patients with orthopedic prostheses and ventriculoatrial and peritoneal shunts, and the appropriate specialist should be consulted in these cases. A 2008 advisory statement on antibiotic prophylaxis in dermatologic surgery expands on these guidelines. [19]
Signs and symptoms of wound infection usually present in an escalating manner from postoperative days 4-6 and include tenderness, erythema, warmth, and swelling at the wound site (see the image below).
Purulent exudate, frank cellulitis, lymphangitis, and fever may be present. If the infection is caught at an early stage (eg, superficial local reaction, lack of cellulitis or systemic symptoms), the patient may be treated with prompt institution of oral antibiotic therapy and close follow-up care. If fluctuance, inflammatory edema, purulent exudate, or systemic symptoms are present, the wound should be opened, lavaged with sterile sodium chloride solution, and packed with iodoform gauze. Wound cultures should be taken, and Gram staining should be performed. Wound culture is especially important because the incidence of community-acquired methicillin-resistant S aureus has increased in recent years. [20] Antibiotics should be started to cover likely organisms after culturing and changed, if necessary, pending results of culture and sensitivity tests.
Patients should be closely monitored to evaluate the clinical response. If the patient continues to worsen despite appropriate treatment, possible concomitant infection with less common pathogens, such as candidal, fungal, and mycobacterial organisms, should be considered.
Suture Reactions and Contact Dermatitis and Hypersensitivity
Suture reactions
Sutures are foreign bodies; as such, they cause a local, immunologically mediated tissue response, clinically evident as erythema. This reaction must be differentiated from true wound infection and contact dermatitis (eg, to topical antibiotic or tape adhesive). Many factors may contribute to suture reactivity. The longer the sutures are in, the more reactivity occurs. The larger the caliber of the suture, the more reactivity; an increase of one suture size results in a 2- to 3-fold increase in tissue reactivity. Synthetic or wire sutures are much less reactive than natural sutures (eg, silk, cotton, catgut); a monofilament suture is less reactive than a braided suture.
Other risk factors for tissue reactivity include anatomical site (eg, the chest, the back, the extremities, the sebaceous areas of the face), male sex, advancing age, and the surgeon's inexperience. A recent study of 1000 patients indicated that these secondary factors may play a larger role in the process than the sutures themselves.
No hard and fast rules exist about the appropriate time for suture removal; the time of removal largely depends on the surgeon's judgment. The need for tensile strength must be balanced with the potential for complications of sutures left in too long. This need is less of a problem when deep absorbable sutures are present to provide tensile strength for a longer period. An erythematous healing ridge is an indicator of reepithelialization, and it should be present before the sutures are removed to avoid the danger of dehiscence. Applying Steri-Strips after suture removal may provide added strength. In general, accepted time intervals for suture removal vary by body site, 5-7 days for the face and the neck, 7-10 days for the scalp, 7-14 days for the trunk, and 14 days for the extremities and the buttocks.
Percutaneous sutures create puncture tracks through the skin and the subcutaneous tissue; these tracks begin to reepithelialize as wound healing progresses. In general, if sutures are removed within 7-10 days, these epithelial cells tend to regress; if left in for a longer time, a foreign body reaction ensues, which may result in erythematous papules or stitch abscesses surrounding the sutures. Stitch abscesses are sterile pustules that result from tissue reaction to the keratinizing epithelial cells, which have migrated along the wound created by suture placement; this process may lead to permanent fibrosis and scarring.
Suture spitting results from deep sutures being placed too high in the dermis. Suture splitting can occur from several weeks to several months after surgery. It usually presents as a noninflammatory papule and progresses with extrusion of the suture through the skin. The suture material may be trimmed or removed if loose, and it is not needed for maintaining wound strength.
Suture tracking results from the sutures being tied too tightly or being left in place too long. Puncture scars on either side of the wound connected by a linear scar in the area where sutures were placed give a railroad track appearance (see the image below).
This complication is best prevented by tying the suture just tightly enough to approximate the tissue. Additionally, the use of a suture with stretch, such as Prolene, and the use of loop sutures (eg, loose first knot, secured second and third square knots) may be helpful, allowing some suture "give" as the wound evolves. Once suture tracking has occurred, the normal contour of the skin may be restored by using laserbrasion or dermabrasion.
Tissue reactivity also has a negative effect on the local immunologic response against infection.
An allergic reaction to suture material is a rare complication. Hypersensitivity to chromic catgut suture is the most commonly reported reaction [21] ; however, allergies to silk and nylon sutures have also been reported. [22] Patients suspected of suture allergy should be patch tested to guide future treatment.
Also see Materials for Wound Closure and Suturing Techniques.
Contact dermatitis and hypersensitivity
Contact dermatitis must be differentiated from wound infection and suture reaction, both of which cause erythema around the wound. Typically, contact dermatitis is readily recognized by the characteristic shape of the erythematous area. An erythematous plaque in the shape of a square or following the shape of a bandage strongly suggests contact dermatitis (see the image below). The presence of vesicles and pruritus further supports the diagnosis.
Dermatitis may result from irritation or delayed-type hypersensitivity to any of the topical agents used in wound care. Neomycin represents the most common allergen in this group. In one prospective study, the frequency of allergic contact dermatitis due to neomycin was 5.3%. The incidence of bacitracin allergy has been increasing in recent years. [5] Polymyxin B and mupirocin are less common sensitizers. Because of the high incidence of neomycin allergy, the use of neomycin is best avoided.
Prolonged contact with an open wound can readily lead to sensitization. One study demonstrated no significant difference in the postoperative infection rate when comparing white petrolatum and bacitracin, [23] although a 2016 meta-analysis did show a slight advantage with the use of topical antibiotics when compared with white petrolatum in the prevention of infection. [24] However, despite this, most dermatologic surgeons recommend white petrolatum alone as part of their standard wound care protocol, given the dramatically increased risk of contact dermatitis with topical antibiotics.
Irritant contact dermatitis that results from adhesive bandage use is common; however, true allergic contact dermatitis is rare. [25] Paper tape may be used as an alternative in patients who experience dermatitis caused by bandage adhesive. Allergic contact dermatitis to povidone-iodine solution and chlorhexidine has been reported but is also rare. [26, 27, 28] Delayed-type hypersensitivity has been reported with the use of topical lidocaine.
Treatment of contact dermatitis necessitates avoiding exposure to the allergen. Topical steroids decrease inflammation and relieve pruritus. Oral corticosteroids may be required in severe cases. Exuberant vesiculation and weeping may be ameliorated by the use of Burow solution (aluminum acetate) or approximately 25% vinegar in water soaks. Patients with suspected delayed-type hypersensitivity reactions may be patch tested to confirm the diagnosis and to guide future treatment.
Immediate-type hypersensitivity manifests as urticaria, angioedema, or anaphylaxis and represents a potentially fatal complication. This type of allergy to amide local anesthetics (eg, lidocaine, mepivacaine, articaine) is rare, but cases have been reported. [29] Allergy to ester-type local anesthetics (eg, procaine, benzocaine, tetracaine) is more common because of their metabolism to p- aminobenzoic acid (PABA), a potential allergen. Anaphylaxis to bacitracin and chlorhexidine has been reported in rare cases. [30, 31] Evaluation of patients with suspected immediate-type hypersensitivity is best performed by a specialist in this area, in a setting equipped for emergent resuscitation.
Dehiscence, Necrosis, and Surface Contour Irregularity
Dehiscence
Dehiscence results when a wound fails to heal in apposition. The healing wound has minimal tensile strength, and, although reepithelialization occurs rapidly within 2 days, fibroplasia and subsequent collagen production are initiated after a delay of approximately 5 days. The deposition and remodeling of collagen gradually increase the tensile strength of the wound. The wound regains 3-5% of its original strength at 2 weeks; 15%, at 3 weeks; 35%, at 1 month; and increases to a final strength of 80%, after several months.
Both systemic and local factors can cause wound dehiscence; however, the most common cause involves surgical error. Excessive tension on the wound resulting from inadequate undermining or poor planning of the repair causes the wound to split apart because of sheer mechanical force. Unduly tight sutures also strangulate the wound edges, causing necrosis and decreased strength. The use of electrocautery coagulation decreases the tensile strength of wounds by increasing inflammation in response to necrotic tissue.
Dehiscence may result when sutures are removed too early, especially in wounds that do not have adequate buried absorbable sutures to provide tensile strength (see the image below). Superficial sutures serve to approximate wound edges, but they do little to fortify the wound against tearing apart. Dehiscence may become apparent immediately upon suture removal. The surgical dictum of "without inflammation, there is no healing" provides a clue to the readiness of the wound for suture removal. One should note a pink, raised healing ridge (which usually appears at days 5-8) prior to suture removal. Complications, such as hematoma, infection, and trauma, can also result in wound dehiscence.
Systemic factors increase a patient's risk of wound dehiscence. Age older than 65 years, hypoalbuminemia, obesity, uremia, malignancy, systemic infection, hypertension, Cushing disease, thyroid disease, liver disease, and congestive heart failure can predispose to wound dehiscence. Additionally, tobacco use and certain medications (eg, anticoagulants, aspirin, colchicines, systemic corticosteroids, penicillamine, cyclosporine, metronidazole, cytotoxic chemotherapeutics) have adverse effects on wound healing and increase the risk of dehiscence.
Prevention of wound dehiscence by proper surgical technique is ideal. Avoiding crushing of tissue, excessive electrocautery, ineffective hemostasis, dead space in the wound, excessive wound tension, and overly tight sutures is important, because they not only increase the risk of dehiscence but also contribute to the development of other complications.
Buried absorbable sutures should be adequately used to provide tensile strength. Consideration should be given to the tensile strength retention properties of suture material when suturing high-tension areas, such as the back. For example, polydioxanone (PDS II) is a synthetic absorbable monofilament suture with low reactivity and prolonged retention of tensile strength. The suture retains 70% of its strength at 2 weeks; 50%, at 4 weeks; and 25%, at 6 weeks, providing extended wound support. This suture has been associated with significantly less scar spreading in high-tension areas when compared with a polyglycolic acid (Dexon) suture and is the authors’ suture of choice for high-tension, truncal closures. Patients should be instructed to avoid stretching or trauma to the wound area. Wound immobilization with Steri-Strips and a dressing provides some protection for the area and serves as a reminder to the patient.
Wounds may be resutured in cases of dehiscence due to premature suture removal or trauma without evidence of infection. Devitalized tissue may need to be removed; however, routine freshening of the wound edges should be avoided to prevent removal of active fibroblasts, which are present in the wound edges. Retention of these fibroblasts allows the already initiated healing process to continue. Dehiscence due to hematoma may be resutured in uncomplicated cases after complete removal of the hematoma. In cases of delayed hematoma or infection, the wound is best treated by allowing it to heal by second intention. Scar revision is best planned after adequate healing has occurred, usually no sooner than 8 weeks.
Necrosis
Necrosis of tissue occurs secondary to tissue ischemia. Any condition that results in a decrease of oxygenated blood flow to the wound has the potential to cause necrosis. Damage to tissue during surgery is the most common cause. Excessive tension on wound edges, excessive suturing and undermining, and superficial undermining all decrease blood flow to the distal wound margins. Grafts as well as random pattern flaps with a length-to-base ratio of greater than 4:1 are at high risk of necrosis because of the precarious nature of the circulation at the distal wound edges (see the image below).
Other complications can contribute to tissue necrosis. An expanding hematoma may cause excessive tension on the wound, leading to compromised blood supply and tissue death. A hematoma causes flap necrosis by a free radical–induced cytotoxic mechanism. Current investigations include the use of free radical scavengers, such as deferoxamine, as potential treatments to increase flap survival.
Cigarette smoking has a deleterious effect on the survival of reconstructive flaps and grafts. Smoking results in vasoconstriction; increased blood viscosity; hypoxia; and increased platelet aggregation, which promotes microvascular thrombosis. Patients who smoke more than 1 pack of cigarettes per day have 3 times the risk of necrosis of flaps and full-thickness skin grafts when compared with persons who have never smoked, low level smokers (< 1 pack/d), and ex-smokers. When necrosis does occur, the median area involved tends to be greater in smokers (approximately 3-fold) than in patients who never smoked. Many of the adverse effects of cigarette smoking on the microvasculature are reversible; benefits in flap and graft survival may be realized by stopping (or decreasing) smoking for at least 2 days before surgery and for 1 week after surgery. Treatment with parenteral pentoxifylline and topical nitroglycerin has been shown to improve skin flap survival in animal models. [32, 33, 34]
Treatment of necrosis is conservative. The necrotic area should be allowed to fully demarcate. Debridement prior to this time may injure viable tissue and should be avoided, except in cases of hematoma and infection. When the eschar begins to easily separate from the wound bed, careful sharp debridement may be performed, and the wound may be allowed to heal by second intention granulation. These wounds are at higher risk for infection, and the need for systemic antibiotics should be considered. If necessary, scar revision may be performed at a later date.
Surface contour irregularity
Surface contour irregularity is to be expected in the healing wound. Patients should be advised of this fact, and they should be told what to expect during the healing process. Postoperatively, the scar is purple-red and raised for the first week and may even appear more so with the resolution of edema within the first postoperative days. The erythema gradually diminishes, and the scar appears less red and raised after several weeks. The appearance continues to evolve over several months to 1 year, leaving the scar flatter, paler, and thinner. Scar maturation takes time and may continue to improve up to 18 months after surgery. Patients should be counseled that the appearance of the scar at 1 week after surgery does not count as much as its appearance in the long term. Because of this long maturation process, scar revision is best deferred for at least 1 year.
Spread scars occur on high-tension and high-use areas (eg, shoulders, back, chest), and they occur as a result of complications, such as infection or dehiscence. Spread scars may result from premature or excessive intralesional steroid injections. The best therapy for spread scars is prevention by good surgical technique. The use of buried absorbable sutures with long tensile strength retention time (eg, polydioxanone) decreases spread scars in high-tension areas. Excisional scar revision and dermabrasion or laserbrasion may be performed when the scar has matured.
Depressed scars and trapdoor deformities most commonly occur in sebaceous areas, typically on the nose. These scars may be treated by scalpel scar revision, dermabrasion, or laserbrasion to restore a smoother contour. Less commonly, dermal or subcutaneous fillers, both temporary and permanent, may be used to achieve a satisfactory result.
Dog ears may result when the angle at the apex of the ellipse exceeds 30-35°, especially in areas where skin is less pliable and over convexities. This complication can usually be avoided by ensuring that the length of primary closure is at least 3-3.5 times the width of the defect. Small dog ears, especially on the trunk and hands, usually flatten out over time and become inconspicuous. [35] Larger standing cones may be treated by excisional scar revision.
Hypertrophic scars (see images below) and keloids represent a pathologic response to tissue injury and can be pruritic. Excessive scar tissue that is raised above the level of the wound but remains within the confines of the original area of injury is termed hypertrophic scarring. Keloids extend beyond the original wound area. Both problems can cause cosmetic disfigurement and functional disability. Hypertrophic scars and keloids are more common on the chest and the back and in darker skin types. Hypertrophic scars arise more frequently in wounds allowed to heal by second intention. Management of these 2 entities differs because of their different patterns of evolution; hypertrophic scars arise early (4 wk postoperatively), they often spontaneously regress, and they do not recur. Keloids may arise months after surgery, they do not regress spontaneously, and they frequently recur.
Management of hypertrophic scars and keloids traditionally includes intralesional steroid injections. Silicone gel sheeting and nonsilicone occlusive dressings have demonstrated efficacy in some cases. [36, 37] The 585-nm pulsed dye laser may be used to improve the appearance and to reduce the symptoms; however, results are variable. [37] Other treatments for keloids include topical retinoids, topical imiquimod, [38, 39] cryosurgery, pressure therapy, recombinant interferon gamma and interferon alpha-2b, and low-dose ionizing radiation. Surgical scar revision with intraoperative and postoperative intralesional steroid injections may also be effective.
Nerve Injury and Other Complications
Nerve injury
Inadvertent nerve damage is one of the most dreaded complications of dermatologic surgery. Patients should always be warned of the possibility of nerve injury during discussion of informed consent. Nerve injury may be transient and reversible or permanent. Thorough knowledge of the anatomy, with special attention to known danger zones, is required to anticipate vital structures as they are approached. Effects of local anesthesia may result in temporary sensory or motor nerve paralysis; these conditions resolve within 1 day. Neurapraxia refers to a deficit caused by inadvertent pressure or tension during surgery. This type of injury may result in sensory or motor deficits, and it may persist for months.
Transection of small cutaneous sensory nerves is common, resulting in a patch of anesthesia at the surgical site. This type of injury is reversible; sensation typically returns within several months. Damage to the branches of the trigeminal nerve (cranial nerve V) is associated with larger areas of deficit. Transection of the supratrochlear or supraorbital nerves results in anesthesia superior to the area of injury on the forehead and scalp and extends along the entire course of the injured nerve. Damage to the infraorbital nerve results in loss of sensation to the nose and the cheek. Mental nerve injury is more functionally problematic, resulting in numbness of the lip. Sensation is often at least partially restored within 6 months.
Transection of branches of the facial motor nerve (cranial nerve VII) causes functional disability, which is usually permanent. The temporal branch of the facial nerve is very superficial as it crosses the zygomatic arch in the temple region. It is vulnerable to injury in this area, especially in elderly patients with thin skin. Transection of the temporal branch to the frontalis muscle results in unilateral eyebrow ptosis and loss of the normal forehead furrows (see images below).
 Injury to the temporal branch of the facial nerve causing eyebrow droop and loss of normal forehead furrows.
Injury to the temporal branch of the facial nerve causing eyebrow droop and loss of normal forehead furrows.
Injury to the branches supplying the orbicularis oculi muscle may result in difficulty closing the eye or ptosis (the orbicularis oculi muscle has a coexisting supply from the zygomatic branch). The zygomatic branch of the facial nerve is less vulnerable as it crosses the zygoma because of its deep plane; it exits the parotid gland prior to its entry into the orbicularis oculi muscle. Injury to this nerve results in ectropion and in the unilateral inability to close the eyelid.
Transection of the buccal branch of the facial nerve along its course from the parotid gland to the orbicularis oris muscle results in facial asymmetry and in the inability to pucker the lips. Buccal nerve paresis has been reported in a patient with a history of an ipsilateral parotidectomy prior to a Mohs procedure and reconstruction. [40] Injury to the marginal mandibular branch may result in facial asymmetry and in weakness of the lips. The nerve is vulnerable at the angle of the jaw as it courses from under the parotid gland. The sequelae of motor nerve injury may be treated with reconstructive procedures to restore functionality, such as a brow lift or a blepharoplasty. In other cases, nerve anastomosis or transplantation may be indicated.
Other complications
Milia are essentially tiny epidermal inclusion cysts. Their occurrence is commonly reported after dermabrasion because they have been unroofed. However, they may also appear after excisional surgery at the suture line because of implantation of epidermal components into the dermis. Treatment of milia consists of incision and extraction. Tretinoin, glycolic acid, and gentle abrasion are also effective treatments. [41]
Telangiectases (see image below) may appear after surgery around the sutured area, and they are often associated with wound tension or a personal tendency. Treatment may be expectant; telangiectases may resolve spontaneously in 6-12 months. If treatment is desired, several options exist. Lasers shown to be effective in the treatment of telangiectasias include the 532-nm potassium titanyl phosphate (KTP), the 532-nm diode copper vapor, and the 585-nm pulsed dye lasers. The 532-nm KTP and the copper vapor lasers have both demonstrated comparable efficacy to the pulsed dye laser in the treatment of telangiectasias with greater patient acceptance (no purpura). [4] Treatment with a 595-nm pulsed-dye laser using an elliptical spot in conjunction with a long pulse width shows very good efficacy without purpuric adverse effects. [42] The vessels may also be ablated by platinum-tipped electrocautery.
Hypergranulation (also termed "proud flesh") may occur in wounds that are healing by second intention. This aberrant response represents overgrowth of fibroblasts and endothelial cells, and it is clinically recognized by its beefy, friable, red appearance. These highly vascular lesions resemble pyogenic granuloma on histologic analysis, and they bleed easily. The presence of this tissue results in the inhibition of fibroblast proliferation and prevents wound healing. Treatment consists of destruction of the hypergranulation tissue by cautery, shave excision, silver nitrate, aluminum chloride, or curettage.
Pruritus within scars is a relatively common occurrence. The association of increased numbers of mast cells and histamine production within scar tissue is debatable. The most consistently effective treatment is time. Massaging the scar with an emollient has been reported to reduce itching, pain, and anxiety and to improve the patient's mood. [43] Topical steroids may be effective in decreasing pruritus. Postsurgical treatment with topical onion extract has failed to show significant improvement in scar erythema and pruritus when compared with a control emollient. [44]
Other complications may be peculiar to the specific anatomical site. Ectropion (see image below) entails eversion of the lower eyelid margin with scleral show, and it causes an inability to fully close the eye. It is a problematic condition, resulting in a dry, irritated eye. This complication occurs when excessive tension is placed on the lower eyelid, and it may be due to several factors, such as scar formation, excessive lid laxity, injury to the orbicularis muscle, nerve injury, or poor surgical planning. Of these, poor surgical planning is responsible for most cases of ectropion.
When planning an eyelid repair, patients at risk for ectropion formation may be identified with the snap test. The lower eyelid is gently pulled away from the globe and allowed to retract. Healthy elasticity and tone cause the eyelid to quickly snap back. Delayed retraction is indicative of high risk for ectropion formation. Ectropion is best prevented by surgical design; all tension vectors should be directed perpendicular to the free margin of the eyelid. If ectropion does occur, initial management includes upward massage of the eyelid. Eventually, surgical intervention, such as a skin graft, V-Y advancement flap, wedge tarsectomy, or lateral tarsal strip procedure, may be required.
Eclabium is a similar condition resulting from excessive tension in the perioral area causing eversion of the lip, and it may result in functional disability (see image below). Scar revision may be performed to improve cosmesis and to restore functionality.
The ear represents a complex anatomical structure with the potential for unique postoperative complications. Chondritis (see image below), perichondritis, chondronecrosis, and stenosis of the external auditory canal may complicate auricular surgery. [45] Pseudomonas aeruginosa is commonly implicated in postoperative infections involving the ear. Progression of infection is rapid, and immediate systemic antibiotic treatment with pseudomonal coverage is necessary. Stenosis of the external canal commonly results from wounds in this area left to heal by secondary intention. Immediate reconstruction is advised to avoid stenosis. Additionally, autonecrosis of skin during secondary intention healing, tragal retraction, and extension of the tumor through fenestrated cartilage have been reported.
Conclusion
Serious postoperative complications arising from dermatologic surgery are uncommon. Many problems may be prevented by thorough preoperative evaluation, sound surgical technique, and careful follow-up care. Good communication and patient rapport are invaluable. Patients must be informed of all possible risks (likely or unlikely), advised on what to expect in the postoperative period, and educated in the early recognition and reporting of adverse events. Open and honest discussions of the surgical goals, careful listening to the patient's concerns, and prompt intervention when complications are suspected allow the development of trust, result in patient cooperation, and potentially avoid litigation.
-
Preoperative evaluation questionnaire.
-
Ecchymosis on the neck due to tracking of blood in naturally occurring tissue planes.
-
Periorbital ecchymosis.
-
Extensive ecchymosis in a patient on anticoagulant medication.
-
Early hematoma under full-thickness skin graft repair.
-
Expression of early hematoma.
-
Expression of the hematoma in this patient did not require takedown of the graft.
-
Aspiration of seroma.
-
Erythema and induration characteristic of postoperative wound infection.
-
Typical railroad track appearance of suture tracking caused by sutures that were tied too tightly.
-
Contact dermatitis.
-
Dehiscence of a wound.
-
Graft necrosis.
-
Hypertrophic scar.
-
Hypertrophic scar in an area allowed to heal by second intention granulation.
-
Injury to the temporal branch of the facial nerve causing eyebrow droop and loss of normal forehead furrows.
-
Injury to the temporal branch of the facial nerve causing an inability to raise the eyebrow.
-
Postoperative telangiectasia radiating from a scar.
-
Ectropion demonstrating the lower eyelid being pulled away from the globe with scleral show.
-
This patient had an eclabium from prior surgery.
-
Chondritis.
-
If a hematoma is noticed in the early postoperative period, it may be expressed through the suture line or by partial takedown of the repair. Sutures must be removed if wound compromise (excessive tension on the suture line) is present.