Background
The nail complex, also known as the perionychium, is the structural and functional unit of the fingernail. The nail complex consists of the firm nail plate, nail bed (ie, sterile and germinal matrices), proximal fold (ie, eponychium), distal groove (ie, hyponychium), and lateral grooves (ie, paronychium) (see the image below). [1, 2, 3] Aside from being aesthetically appealing, the nail unit has the important function of protecting the distal phalanges, fingertips, and surrounding soft tissues from external injury, as well as enhancing precise delicate movements of the distal digits through the mechanistic action of counterpressure exerted over the volar skin and pulp. [4, 5]
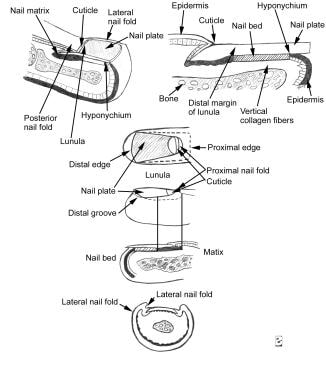 Longitudinal section of a digit showing the dorsal nail apparatus (top). Component part of the nail apparatus (bottom).
Longitudinal section of a digit showing the dorsal nail apparatus (top). Component part of the nail apparatus (bottom).
See 15 Fingernail Abnormalities: Nail the Diagnosis, a Critical Images slideshow, to help identify conditions associated with various nail abnormalities.
Performing successful nail surgery requires a comprehensive understanding of nail anatomy and physiology. [6, 7] Knowledge of the associated vascular and neural pathways supplying the nail complex and the functions and relationship of each component of the nail unit is also essential. Thus, the nail surgeon should be equipped with knowledge of nail pathology, surgical techniques and instrumentation, anesthesia, preoperative evaluation, management of complications, and wound care and healing after surgery. This knowledge ensures minimal patient discomfort, maximal patient satisfaction, and optimal surgical success. With these goals in mind, this article reviews the nail anatomy and focuses on common nail pathologies with the corresponding surgical techniques used for their diagnosis and treatment.
Indications
Multiple indications for surgical exploration of the nail unit exist, ranging from infectious and inflammatory to neoplastic and traumatic causes. Some commonly encountered disease processes affecting the nail complex include onychomycosis (ie, fungal infection), onychocryptosis (ie, recalcitrant ingrown nails), onychogryphosis (ie, hornlike hypertrophy of the nail plate), and onychauxis (ie, thickened nails), as well as psoriasis, lichen planus, congenital nail dystrophies, and tumors. In addition, nail surgery is frequently performed to aid in a suspected diagnosis, to relieve pain, and to correct or prevent anatomical deformities of the nail.
Paronychia
Acute paronychia is an acute inflammation of the nail fold and frequently results from minor trauma, such as an accidental break in the skin, a splinter in the distal edge of the nail, a thorn in the lateral groove, a hang nail, or excessive nail biting leading to infection of the surrounding soft tissues. [1, 8, 9] The infectious process begins in the lateral perionychium and is characterized by the development of erythema, intense inflammation, swelling, pain, and local tenderness. While the timing of the presentation may vary, it is often 2-5 days after the initial trauma. [10] Vesicles and blisters may also form, but may also indicate herpetic whitlow.
Chronic paronychia is characterized by acute exacerbations of self-limiting inflammation and infection followed by remissions. Chronic paronychia commonly occurs in hands that are repeatedly exposed to water. [11] The proximal nail fold (PNF), the lateral nail fold (LNF), and the cuticle are progressively damaged over time. The potential barrier formed by the PNF is impaired, and the cuticle eventually detaches from the nail plate. The loss of seal allows for moisture accumulation, inoculation of bacterial or fungal pathogens, and irritants to penetrate within the nail bed grooves, leading to further exacerbation. [12]
The warm moistened environment is ideal for bacterial proliferation. Secondary Candida and bacterial infections (eg, Pseudomonas aeruginosa, Staphylococcus aureus) are implicated in acute exacerbations. [13] Exacerbations may be initiated through contact with irritants and allergens. Chemical and irritant contact dermatitis is common. Exacerbations usually resolve several days after abscesses spontaneously drain, but they lead to prolonged edema and fibrosis of the nail folds. [13] Factors to consider when assessing management options include etiology, duration, extent of paronychial involvement, and associated risk factors present such as contact with oral secretions or exposure to animals. [10]
Onychocryptosis
In onychocryptosis (ingrown nail), the toenails are most commonly affected; the fingernails are rarely afflicted. Predisposing factors involved in the pathogenesis of an ingrown nail include congenital malalignment of the digit; hyperhidrosis (commonly occurs in athletic adolescents); increased pressure from external sources (eg, trauma); poorly fitted shoes; poor posture and gait; excess internal pressure, which results in overcurvature of the nail plate; incorrectly trimmed nails or naturally short nails; underlying systemic disease (eg, obesity, diabetes mellitus); arthritis; skeletal disease; onychomycosis and other diseases that result in abnormal changes in the nail plate; and senile nail diseases (eg, onychauxis, subungual hyperkeratosis). [2, 8, 14]
In onychocryptosis, the primary direction of nail growth is lateral instead of the normal, proximodistal orientation. A more pronounced transverse curvature of their toenails increases the likelihood of developing ingrown toenails. [15] The laterally curved edge of the nail plate, or the nail spicule, penetrates the adjacent LNF, perforating the fold skin and the surrounding dermal components. Perforation of the lateral fold skin results in painful inflammation that manifests clinically as mild edema, erythema, and pain. [13] In advanced stages, drainage, infection, ulceration, and hyperhidrosis may be present. Hypertrophy of the lateral nail wall occurs, and granulation tissue forms over the nail plate and the nail fold during healing of the ulcerated skin. The resulting edema further exacerbates the problem by compressing the lateral dermal tissue between the sharp nail plate and the bony phalanx.
Failure to destroy or remove the lateral horn of the matrix can result in identical regrowth of the former nail, which reintroduces an epidermal breakage and a larger regrown nail. [15]
Myxoid cysts
Myxoid cysts are dome-shaped, translucent, solitary nodules occurring on the dorsal aspect of the finger. [13, 16, 17] Occasionally, the toes may develop these cysts in a similar location. Typically, the cysts are lateral to the midline between the PNF and the distal interphalangeal (DIP) joint. [16] The cysts typically measure 4-10 nm in diameter and can result in a longitudinal depression in the nail plate, as a result of pressure on the matrix. [18]
Although the etiology of these masses is not entirely clear, DIP joint myxoid cysts have been associated with the formation of a tract or communication with the joint. Cysts may also occur in the presence of degenerative disease of the DIP joint and in association with marginal osteophytes, thus explaining their presence in patients with osteoarthritis. [13, 19] As a result, myxoid cysts are frequently mistaken for synovial cysts. Myxoid cysts of the PNF may result from increased synthesis of hyaluronic acid by local fibroblasts. [13, 20] Whether or not these mechanisms of cyst formation occur is controversial.
Warts
Periungual and subungual warts are benign, fibroepithelial tumors that commonly affect the paronychial region of the nail unit. Also referred to as common warts, these hypertrophic growths have a rough, keratotic surface and tend to occupy the nail grooves, the retroungual nail folds, and the subungual area under the nail plate. Periungual and subungual warts are the single most common benign tumors of the perionychium and are caused by the human papillomavirus (HPV). In children, warts caused by HPV are most commonly found on the dorsal aspect of the distal interphalangeal (DIP) joint. [21]
Certain subtypes of HPV associated with periungual and subungual warts may cause squamous atypia. Usually, these warts are mildly infective tumors and present as multiple lesions. However, they appear to be more aggressive and destructive than other types of common warts in this location. [13]
In the absence of fissuring, periungual warts are usually asymptomatic. Subungual warts initially infect the hyponychium, gradually move toward the nail bed, and lastly involve the nail plate. They commonly cause pain. Typically, the nail plate is spared, except for ridging that occurs on the surface of the nail plate.
The differential diagnosis in clinical presentations of periungual and subungual warts should include epidermoid carcinoma and keratoacanthoma. [1, 8] The warts may be mistaken for a glomus tumor. The spread of periungual warts is assisted by biting and picking the nail and surrounding soft tissue. Picking infected lesions can lead to autoinoculation of noninfected fingers. [8, 11, 22]
Common warts under the proximal nail fold cause a swelling, similar to chronic paronychia. [18] Common warts in the posterior nail fold may exert pressure on the matrix, resulting in a deformed nail plate. If left alone, periungual and subungual warts tend to linger and persist as they continue to grow and invade the skin of the other neighboring digits.
Nail trauma
Traumatic injuries of the nail unit include simple or complex lacerations, crush injuries, avulsions, terminal phalanx fractures, and subungual hematomas. Preservation of nail structure and function is the most important consideration when managing injuries to the nail complex. To ensure optimal management in cases of nail unit trauma, early treatment should be initiated. The goal is to explore and repair the wound within hours or days of the injury. In some instances, repair can still be performed up to a week following the injury.
Subungual hematoma
Acute subungual hematoma frequently may result from blunt or sharp trauma to the underlying vascular nail bed. Subungual hematoma may also result from chronic repeated injury to the nail caused by minor trauma, such as trauma of the toenail from poorly fitted shoes. They may also occur in older patients with atrophy of the skin and nails. [11] As bleeding continues, accumulated blood is limited to the subungual compartment of the nail unit. Accumulation of a subungual hematoma is accompanied by inflammation and severe pain secondary to increased pressure of the entrapped blood on the subungual tissue and underlying periosteum.
When acute subungual hematomas are directly under the transparent nail, they have an immediate onset and are conspicuous. In acute subungual hematoma, the nail color is initially red and changes to black after coagulation and degradation. [11] The hematoma is uniform in color with sharply demarcated margins, and it usually grows distally with the nail plate until reaching the free distal edge of the plate where it is no longer seen. Occasionally, the hematoma may persist under the nail and does not move distally with nail growth.
Hemorrhages resulting from trauma to the dorsal nail fold may not appear with forward nail growth for several days. The differential diagnosis of subungual hematoma should include melanoma, glomus tumor, Kaposi sarcoma, basal cell carcinoma, squamous cell carcinoma (SCC), exostosis, melanonychia striata, fungal melanonychia, and keratoacanthomas, all of which must be excluded. [23] To exclude a diagnosis of melanoma, biopsy must be performed in all pigmented lesions of unknown etiology.
Lacerations
Simple superficial lacerations of the nail are usually confined to the nail plate and LNFs. Complex lacerations may involve the nail matrix and PNF and result in partial or total nail avulsion or fragmentation of the nail plate. In some instances, the finger pulp, nail bed, and distal phalanx also may be involved. [23] Complex lacerations may lead to serious complications after injury and should be promptly treated to prevent abnormal nail morphology and function.
Fractures
A major function of the distal phalanx is to support the distal soft tissues of the finger. [24] Fracture of the distal phalanx occurs in approximately one half of nail bed injuries. The type of fracture (open vs closed), [23] the position of the fracture, and the extent of comminution determine treatment. Healing of the fracture may occur by bony or fibrous union and is mostly related to the degree of initial displacement and soft-tissue injury. A Seymour fracture represents an open fracture of the distal phalangeal growth plate in children. [25] Reduction of these fractures is typically prevented by interposition of the sterile matrix. These injuries warrant operative exploration and reduction.
Splinter hemorrhage
Most commonly, trauma or certain disease processes easily injure the small, fine capillaries that line the epidermal-dermal ridges on the nail bed. [1, 8] Splinter hemorrhages result from the extravasation of blood into the potential space between the nail plate and the nail bed after capillaries are disrupted. They develop in the long axis of the nail bed, which conforms to the orientation of the dermal ridges and the subungual vessels.
Other etiologic factors are associated with the formation of splinter hemorrhages in the nail bed; the hemorrhages may clinically occur in such conditions as psoriasis, vasculitis, bacterial endocarditis, arterial embolism, lupus, Darier disease, cirrhosis, hemochromatosis, thyrotoxicosis, and trichinosis. [1, 8, 26] Certain drugs (eg, tetracycline) and drug reactions may also induce their formation. The hemorrhages may be single or multiple, and they appear as brown, red, or black linear streaks, usually in the distal one third of the nail. [8] As the nail grows, the hemorrhages move distally and superficially. They do not tend to blanch on palpation of the nail plate.
Splinter hemorrhages that occur proximally near the lunula are frequently associated with systemic disease. [26] Involvement of multiple nails by these hemorrhages may indicate the presence of an underlying systemic disease. Overall, splinter hemorrhages occur most often in males and in blacks. They commonly involve the thumb and index finger of the dominant hand. However, in studies with single and multiple hemorrhages, the left thumb was found to be the most frequently involved digit.
Nail unit tumors
High-resolution MRI gained prominence in the noninvasive diagnosis of nonmelanoma nail tumors and is capable of detecting lesions that are smaller than or equal to 1 mm in diameter. [27] This modality is helpful in identifying lesions in the following presentations of benign and malignant tumors of the nail: glomus tumors, periungual fibromas or fibrokeratomas, mucous cysts, and exostoses.
Pyogenic granuloma
Pyogenic granuloma is a benign granulomatous lesion commonly seen after a minor trauma penetrates the skin. It usually starts as a small, red papule on the PNF and rapidly grows to the size of a pea. [8, 11] Pyogenic granuloma may also localize to the nail bed after a trauma penetrates the overlying nail plate. Erosion of its surface by pressure necrosis of the overlying epidermis may occur.
Fibroadenoma
Various types of fibroadenoma may occur in the periungual or subungual region. They are usually distinctive in their etiology and presentation.
Glomus tumor
A glomus tumor is a small, well-differentiated, hamartomatous growth of the glomus apparatus. A glomus tumor appears as a small, blue or purple discoloration that may be visible through the nail plate. [8, 11, 17] Most commonly, the tumors are localized to the hand with involvement of the fingertips and the subungual region. Ultrasonography can be used to identify and locate the tumors; however, MRI is more sensitive. The onset of intense pulsating pain with slight pressure or with exposure to cold temperatures is pathognomonic for subungual glomus tumors. Microscopically, all the components in a glomus body are present in this tumor; the components are an afferent arteriole, an efferent venule, glomus cells, smooth-muscle cells, and myelinated and nonmyelinated nerves. [8, 28, 29]
Subungual exostosis
Subungual exostoses are painful outgrowths of healthy bone or remnants of calcified cartilage that frequently occur on the great toe in young persons. [8, 11] Subungual exostosis is not a true tumor. [8] Trauma has been implicated as the inciting cause. The exostosis begins as a small elevation on the dorsal surface of the terminal phalanx. Over time, it may appear as an outgrowth under the distal nail edge, or it may completely destroy the nail plate, creating an environment for tissue erosion and infection. Clinically, patients present with pain that may be accompanied by an abnormal gait because of difficulty walking and a deformed nail. The differential diagnosis includes osteochondroma, which has a similar presentation.
Malignant neoplasm of the nail apparatus
It is likely that the most common malignant neoplasm of the nail subunit is melanoma. Hence, it is not surprising that the majority of these malignant lesions present as pigmented brown-to-black streaks, qualifying as longitudinal melanonychia. The location of the pigmented streak in the nail subunit largely determines the surgical approach that should be used. Interestingly, melanomas confined to the nail bed often present without pigment and are amelanotic. [18]
An elliptical or punch biopsy is typically performed for pigmented streaks in a median position, or a complete horizontal excision may be used. A lateral longitudinal nail biopsy is used for brown streaks in a lateral position. [18]
A confirmed diagnosis of nail melanoma is managed surgically by total excision of the entire nail unit with confirmed negative tissue margins on histopathology. The resulting defect can be repaired with a cross-finger flap or a full-thickness skin graft. Melanomas of the nail apparatus measuring greater than 1 mm in depth require distal amputation. [18]
Relevant Anatomy
The nail plate, the largest segment of the nail unit, is a dense, keratinous horny structure derived from the germinal matrix, or nail root. [1, 2, 3, 4, 5] Externally, the germinal matrix is visualized as the lunula, a light crescent-shaped structure at the proximal base of the nail. Destruction of the nail root, despite an intact nail bed, results in permanent loss of the nail plate. Nail growth occurs in a forward distal direction, and growth of the nail plate is directly proportional to the turnover rate of cells in the matrix. Complete growth of the fingernail plate, measured from the matrix to the distal free edge of the plate, is estimated to occur every 3-6 months, corresponding to a rate of 0.1 mm daily. [1, 2, 3, 30] The turnover time for the toenail plate is longer, averaging around 12-18 months. [1, 2]
See the image below.
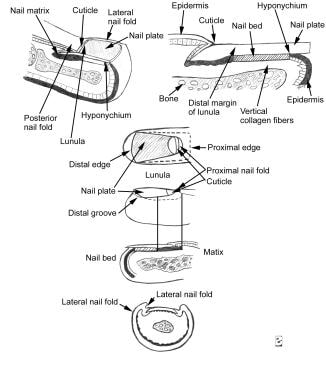 Longitudinal section of a digit showing the dorsal nail apparatus (top). Component part of the nail apparatus (bottom).
Longitudinal section of a digit showing the dorsal nail apparatus (top). Component part of the nail apparatus (bottom).
Grossly, the nail plate is composed of 3 distinct layers: a dorsal thin layer, a thick intermediate layer, and a ventral layer. [4, 5] The nail plate originates beneath the PNF and can be seen passing over the lunula. [31] and the richly vascularized nail bed where it firmly attaches. The nail plate is bordered by the PNF and LNFs, and it is distally adjoined by the hyponychium, although its free distal border generally extends beyond the distal phalanx. The healthy nail plate appears as a smooth, convex, nearly rectangular, translucent structure that has a pink color when light is reflected from its surface; the color is due to the underlying vascular-enriched nail bed. [1, 4, 5]
The shape of the nail plate largely conforms to the convexity of the distal margin of the lunula, the visible crescent-shaped distal segment of the matrix. The nail plate exhibits a thickness gradient with the nail thickness, increasing proximally to distally and with age. Thus, the nail plate tends to be thinner at the lunula. [1, 4, 5, 32] Nail thickness is directly related to the length of the matrix. [1, 30] In darkly pigmented persons, a hyperplasia of melanocytes is commonly seen throughout the matrix epithelium, resulting in longitudinal linear bands of light brown to black pigment visible through the nail plate. [1, 30, 33] Although the linear bands of pigment may represent pathological states, they may be a normal finding in people of color, secondary to hyperproduction and accumulation of melanin.
The onychodermal band is the narrow, transverse delineation at the distal end of the nail plate. This band appears yellowish white in whites or reddish brown in darkly pigmented persons. The onychodermal band marks the point of separation of the nail bed from the nail plate, [14] and it appears to be important in preventing onycholysis after trauma. This band may be prominent in cirrhosis, acrocyanosis, and other chronic diseases. [3, 8] The onychodermal band has been postulated to have a separate vascular supply from the rest of the nail bed. [4, 5, 11]
Hyponychium
The hyponychium is the anatomical area that begins at the onychodermal band, where the nail bed ends, and terminates at the distal groove. The distal groove is a transverse demarcation extending across the distal digit that divides the hyponychium from the volar epidermis of the digit. This groove is the first component of the nail unit to be recognized during the embryologic period, and it is the origin point of the volar epidermis. [1] In persons who bite their nails, the distal groove is easily identified. [1]
The solehorn is the ventral cuticle layered between the ventral nail plate and the distal nail bed; it functions as a potential waterproof barrier. [30] in the space created by its firm attachment to the nail plate and the distal bed epithelium. In this capacity, the solehorn prevents the entrance and invasion of offending organisms and, therefore, protects the nail plate from infection (eg, distal subungual onychomycosis). Frequent aggressive manicuring of the hyponychial area results in disruption of this barrier and allows microbes to enter it.
Proximal nail fold
The PNF is a continuation of the dorsal skin of the digit that folds back on itself at the nail root to create 2 epithelial surfaces: a superficial dorsal layer and a deep ventral layer. [3, 4, 5, 14] The ventral layer travels to the base of the nail plate and becomes continuous the nail matrix. Thus, the PNF obscures most of the nail root (germinal matrix) and the area where the proximal nail plate embeds itself into the proximal groove.
The PNF is also contiguous with the LNFs that border the nail plate. Where the two epithelial surfaces meet, the cuticle converges onto the distal nail plate. [3, 4, 5] The cuticle is the horny end product of the PNF, adhering to the dorsal wall of the nail plate. It is the true nail vest that appears as a fine white band. [30] The role of the cuticle is similar to that of the solehorn; it functions as an impermeable barrier, sealing off the potential area that exists between the PNF and the nail plate. Eventually, the cuticle is shed like the cornified horny layer of epidermal skin.
When the cuticle is disrupted, usually due to overzealous manicuring or nail-biting, [30] the individual becomes susceptible to paronychia and other infectious and inflammatory diseases. Damage to the cuticle can also result in increased chemical insults, such as irritant contact dermatitis. [8] Loops of blood capillaries are sometimes found in and around the PNF, and they may be pathognomonic for certain diseases, such as dermatomyositis and lupus erythematosus. However, the loops may be a normal finding in certain individuals. [1, 4, 5, 11]
Nail matrix
The nail matrix is the germinative portion of the nail complex, giving rise to the nail plate. [1, 4, 5, 11, 30] The matrix is at the most proximal point of the nail bed and is seated deep beneath the PNF; it is separated from the distal phalanx by only a few millimeters. According to Zaias, "the top half of the nail plate (the dorsal aspect) is derived from the proximal matrix, while the derivation of the lower half (the ventral aspect) is from the distal matrix." The proximal matrix continues proximally and laterally to form the lateral matrix horn. The nail surgeon should be cognizant that the lateral matrix horn may be extensive.
The lunula is an opaque, grayish white, half-moon–shaped structure that extends beyond the distal limit of the PNF. The lunula is usually seen through the transparent nail plate, especially on the thumbs and great toes, as the visible proximal component of the nail matrix. [1, 4, 5, 11] The distal margin of the lunula must always be preserved during nail surgery if the normal shape of the nail is to be maintained [1, 13, 30] An active granular layer typically found in the PNF is missing from the nail matrix; therefore, keratohyaline granules cannot be found in the matrix. The basal cells of the matrix actively participate in the process of differentiation and keratinization to eventually produce the dead horny product, the nail plate.
Several reasons exist why the nail surgeon must attempt to leave the structural and functional boundaries of the nail matrix intact when performing nail surgery; some of the reasons include the following:
-
The matrix is the center of nail formation and the source of the nail plate.
-
Nail growth is a direct function of the rate of turnover of matrix cells. [1]
-
Nail thickness is directly related to the length or the size of the nail matrix. [14]
-
The shape of the distal border of the lunula determines the shape of the nail. If this border is convex, the distal free edge of the plate will also be convex.
Disruption of any of these components of the nail matrix can result in scarring and onychodystrophy of the evolving nail plate. The most common indication for partial or complete destruction of the matrix is a recurring problem of ingrown nails recalcitrant to conventional therapies. The healthy matrix synthesizes a complete fingernail plate on an average of every 6 months. [1, 2, 22]
Nail bed and dermis
The distal nail bed (eg, sterile matrix) is the sterile component of the nail unit and the primary site of nail keratinization. [4, 5] The nail bed extends from the distal lunula to the point of origin of the hyponychium. It shares similar boundaries with the nail plate, with the lunula marking the proximal border of the nail bed, with the lateral folds marking the lateral border, and with the hyponychium marking the distal border.
The epidermis of the nail bed is relatively thin, with a dimensional thickness of only 1-2 cells. [4, 5] The epidermal surface of the bed has parallel longitudinal ridges that interlock with similar folds on the ventral surface of the nail plate. [1, 3, 4, 5, 30] The ridges securely bind the nail plate to the nail bed, allowing a firm adhesion between the 2 structures. The area marking the point at which living cells become keratinized and continue to become dead horny cells of the nail plate is abrupt. [4, 5]
The nail bed is a highly vascular structure that lacks an underlying subcutaneous layer of adipose tissue. As a result, nothing separates the dermis from the periosteum of the distal phalanx. The lack of this layer becomes apparent when one is confronted with aggressive tumors of the nail because such tumors may easily extend to involve the underlying bone.
The connective tissue of the dermis, the dermal collagen, contains a balanced mixture of lymphatics, blood vessels, and elastic fibers. The dermis also has a wealth of glomus bodies and a rich capillary network longitudinally oriented with the parallel ridges. Splinter hemorrhages of the nail plate form when a small amount of blood leaks from the capillary bed into one of these folds and becomes trapped by the nail plate. [2] Melanocytes are not found in the nail bed, although they are present in significant numbers in the matrix.
Vascular and nervous supply
An abundantly rich arterial and capillary vascular network supplies the nail unit. The ulnar and posterior tibial arteries divide into the proper palmar and plantar digital arteries, respectively. The two digital arteries, which occupy the lateral and medial aspects of the digit, form a cruciate anastomosis at the level of the deep dermis in the ventral pulp space. Upon anastomosing on the volar aspect of the terminal phalanx, the two arteries contribute branches to a superficial arcade and the underlying phalangeal periosteum. [30] The superficial arterial arcade, which also receives a contribution from a vessel coursing dorsally over the DIP joint, supplies the PNF, including the capillary loops of the nail fold and the nail matrix.
The digital arteries continue around the waist of the terminal phalanx and onto the dorsal surface where they divide near the DIP joint to form the dorsal and ventral arches supplying the nail bed and the nail matrix. The dorsal arch courses dorsally over the DIP joint where it terminates in an anastomosis with the proximal arch to supply the matrix and the PNF. The capillary loop system in the PNF is derived from the anastomosis between the two arches. [1, 8, 30] Therefore, perfusion of the nail matrix comes from two arterial systems: the superficial arcade and the proximal arcade. Anatomically, the superficial arcade sits at the base of the PNF, while the proximal arcade lies deep to the matrix. [30] The ventral or distal branch supplies the remainder of the nail unit, specifically its most distal aspect, including the fingertips.
An accessory blood supply that is separate from the main blood supply in the pulp space also exists. This accessory system is important in providing adequate perfusion of the nail unit for normal nail growth when the primary vasculature is compromised by disease, which sometimes occurs in scleroderma or infection. [3]
Specialized neurovascular structures called glomus bodies are widely distributed throughout the arterial and deep venous circulation. These oval bodies are encapsulated, consisting of tortuous blood vessels and a neural supply of mostly cholinergic nerves. [3, 8] The glomus bodies form an extensive arteriovenous (AV) anastomotic network, which functions in modulating the thermoregulatory response of the nail unit. Under circumstances where the nail is exposed to cold temperatures, the glomus bodies enhance blood flow to the nail complex by dilating and shunting blood through their complex AV anastomotic systems to prevent ischemia. [3, 4, 5, 11, 34]
The nail apparatus is also richly innervated by a complex neural system allowing tactile sensitivity and sensory discrimination. Anatomically, the laterally positioned digital nerves and their divisions nearly parallel the vascular supply to the nail unit. Specifically, there are two dorsal and two volar digital nerves, and the first through fifth digits are innervated by the dorsal nerves, whereas the second through fourth digits are innervated by the volar nerves.
Contraindications
Relative contraindications to performing surgery in the nail unit include the presence of established peripheral vascular disease, collagen vascular disease, diabetes mellitus, and disorders of hemostasis. Patients presenting with acute infection or inflammation of the nail unit, including the surrounding paronychial tissues, are considered to have relative contraindications to nail surgery. When possible, surgery in these patients should be postponed until the acute event has resolved.
When administering anesthetic for nail surgery, the use of epinephrine should be avoided or cautiously used in patients with a history of thrombotic or vasospastic disease such as thromboangiitis obliterans, Raynaud disease/phenomenon, or severe peripheral vascular disease. [35, 36] Epinephrine has vasoconstricting properties, and it has been associated with necrosis and poor wound healing of tissues. However, these complications appear to be mostly theoretical and have rarely been noted to occur in practice.
Wilhelmi et al performed an extensive review of the medical literature and found no reports of epinephrine as a primary cause of ischemic necrosis or finger gangrene when appropriately mixed with lidocaine for digital block. The authors confirmed this finding when they performed 23 digital blocks with 1% lidocaine with 1:100,000 and 1:200,000 epinephrine. They recommend the use of epinephrine as an adjunctive component to help augment the effect of the local anesthetic, decreasing the total amount of anesthetic required and lowering the risk of toxicity.
Several studies have proposed that epinephrine can be used safely in the digits. [37] Epinephrine is also beneficial in reducing blood loss at the surgical site because of its hemostatic properties. However, Wilhelmi et al caution that the maximum dose of epinephrine used in healthy individuals should not exceed 1 mg. Also, epinephrine should be cautiously administered in patients presenting with pheochromocytoma, severe hypertension, hyperthyroidism, and heart disease. [38]
Sylaidis and Logan determined that digital blocks of 2% lidocaine with 1:80,000 epinephrine were safe, although intense local vasoconstriction was noted at the injection site. In their prospective study involving 100 patients, they observed the effect of 2% lidocaine mixed with 1:80,000 epinephrine on several variables of digital arterial perfusion. No ischemic necrosis of the digit was reported after the application of a digital block. The fingers remained well perfused despite the apparent vasoconstriction at the injection site. [39] Therefore, epinephrine can be a safe and valuable adjunct when appropriately mixed with lidocaine to perform a digital block. In the event that ischemia does occur, it can be reversed with phentolamine injection or nitroglycerin ointment. [35]
During nail surgery, the application of a tourniquet at the base of the digit allows the surgeon to operate in a bloodless surgical field. [40] However, to avoid complications such as vascular compromise of the extremity, the use of a tourniquet for more than 15 minutes should be avoided. Optimal hemostasis is achieved when the tourniquet is applied for a maximum period of 15 minutes during the most critical part of the surgery.
-
Longitudinal section of a digit showing the dorsal nail apparatus (top). Component part of the nail apparatus (bottom).








