Background
Mucous membrane pemphigoid (MMP), also known as cicatricial pemphigoid, refers to a group of rare chronic autoimmune blistering diseases that predominately affect the mucous membranes, including the conjunctiva, and occasionally the skin. Patients with cutaneous involvement present with tense blisters and erosions, often on the head and the neck or at sites of trauma. Scarring of the mucous membranes is common, hence the designation cicatricial, which can lead to decreased vision, blindness, and supraglottic stenosis with hoarseness or airway obstruction. The first international consensus on mucous membrane pemphigoid was published in 2002. [1]
See the illustration below depicting ocular mucous membrane pemphigoid.
 Ocular manifestations of cicatricial pemphigoid (mucous membrane pemphigoid) include symblepharon, demonstrated in this photograph by the tethering of the lower lid to the cornea.
Ocular manifestations of cicatricial pemphigoid (mucous membrane pemphigoid) include symblepharon, demonstrated in this photograph by the tethering of the lower lid to the cornea.
Classification of mucous membrane pemphigoid patients has been difficult because some patients with other autoimmune blistering diseases, including bullous pemphigoid (BP),epidermolysis bullosa acquisita (EBA),and anti-p200 pemphigoid, may have mucosal involvement. Also, clinical heterogeneity exists in the clinical manifestations of this disease, with some patients presenting with ocular involvement and others with oropharyngeal involvement. The heterogeneity in clinical manifestations does not appear to be linked to the heterogeneity of the target antigens alone.
Pathophysiology
As in other autoimmune diseases, environmental factors combined with genetic susceptibility lead to development of autoantibodies. By direct immunofluorescence (DIF) study, antibodies bound in a linear band at the epidermal-dermal junction have been found in patients with mucous membrane pemphigoid (MMP), as depicted below. By immunoelectron microscopy, these antibodies are found in the lamina lucida. In some patients, autoantibodies extend to the lamina densa. When detectable, circulating autoantibodies are present in a low titer. See the image below.
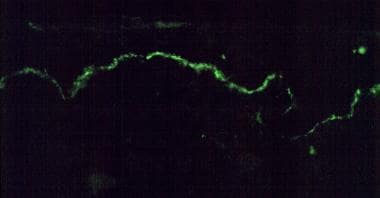 By direct immunofluorescence, a linear band of immunoreactants at the epidermal-dermal junction is demonstrated by using a fluorescein-tagged antibody specific for human immunoglobulin G.
By direct immunofluorescence, a linear band of immunoreactants at the epidermal-dermal junction is demonstrated by using a fluorescein-tagged antibody specific for human immunoglobulin G.
Different epithelial membrane zone components have been recognized by antibodies in patients with mucous membrane pemphigoid, including BP antigens 1 and 2 (BP230 and BP180), laminin-332, laminin-311, type VII collagen, b4 integrin subunit, and antigens with unknown identities (a 45-kd protein, uncein, a 168-kd epithelial protein, and a 120-kd epithelial protein). While circulating autoantibodies in a given patient tend to target a single antigen, sera of patients with same clinical features may target different autoantigens.
Etiology
Mucous membrane pemphigoid (MMP) is an autoimmune blistering disease associated with autoantibodies directed against basement membrane zone target antigens. Autoantibodies of the IgG subclass, particularly IgG4, are associated with mucous membrane pemphigoid; however, IgA antibodies have also been detected. The two major antigens associated with mucous membrane pemphigoid are BP180 and laminin-332. Patients with clinical features of mucous membrane pemphigoid may have antibodies directed against BP230 or type VII collagen. BP180 is a 180-kd hemidesmosomal protein with multiple extracellular collagenous domains. [2] BP180 is also a major target antigen for patients with BP and linear IgA bullous dermatosis. Patients with mucous membrane pemphigoid react with epitopes on BP180 distinct from those associated with BP and linear IgA bullous dermatosis, particularly the C-terminal of the protein. Given this reaction with the C-terminal epitope, routine serology for BP180 may fail to detect patients with circulating autoantibodies. [3]
A subset of patients with mucous membrane pemphigoid reacts with laminin-332. These patients have circulating autoantibodies that bind to the dermal side of salt-split skin as depicted by IIF study. By immunoelectron microscopy, these autoantibodies deposit at the lower lamina lucida, extending to the lamina densa. Laminin-332 contains disulfide-linked alpha, beta, and gamma chains, of which the alpha subunit is the major site of mucous membrane pemphigoid reactivity. Laminin-332 plays a major role in the adhesion of human keratinocytes to the dermis by binding alpha-6-beta-4 integrin. Because defects in laminin-332 are associated with junctional epidermolysis bullosa, one group has suggested calling mucous membrane pemphigoid associated with anti–laminin-332 autoantibodies acquired junctional epidermolysis bullosa; however, most clinicians refer to this disease as antiepiligrin or anti–laminin-332 mucous membrane pemphigoid.
Autoantibodies specific for laminin-332 and BP180 are believed to be important in blister formation. Lazarova et al [4] have developed an animal model of anti–laminin-332 mucous membrane pemphigoid in which passive transfer of rabbit anti–laminin-332 into neonatal mice leads to a subepidermal blistering disease with features consistent with mucous membrane pemphigoid. Passive transfer of anti–laminin-332 antibodies to mast cell and complement-deficient neonatal mice can also induce blistering, suggesting a direct effect of the circulating autoantibodies in inducing dermal-epidermal cleavage.
The incidence of the HLA haplotype HLA-DQB1*0301 is increased in patients with ocular mucous membrane pemphigoid. This HLA haplotype may be important in the presentation of specific epitopes on target antigens in the generation of an autoimmune response; however, the precise events relevant in the initiation of autoantibody production in patients with this disease are unknown.
Epidemiology
Frequency
The incidence of mucous membrane pemphigoid (MMP) has been estimated to be 2 cases per million in studies performed in France and Germany. [5, 6, 7] Pure ocular mucous membrane pemphigoid occurs in less than 1 case per million in the United Kingdom. [8] . Among white patients in the United States, mucous membrane pemphigoid is associated with human leukocyte antigen DQB1*0301 (HLA-DQB1*0301). [9, 10]
Race
No racial predilection is known.
Sex
Most studies have demonstrated a female-to-male ratio of approximately 2:1
Age
Most patients with mucous membrane pemphigoid are elderly, with a mean age of 62-66 years.
Prognosis
Extensive studies on the long-term outcome of patients with mucous membrane pemphigoid (MMP) have not been performed.
In general, mucous membrane pemphigoid is a chronic, progressive disorder that responds poorly to therapy. Some patients may experience long-term remissions. The disease is characterized by intermittent exacerbations and waning of disease activity. Mucous membrane pemphigoid is a chronic blistering disease that frequently heals with scarring. Individual blisters may itch, and subsequent erosions are often painful. Depending on the sites affected, sequelae include decreased vision or blindness, hoarseness, esophageal stenosis, or upper airway compromise. This disease is often recalcitrant to therapy.
A cohort study of 35 patients with anti–laminin-332 mucous membrane pemphigoid indicated an increased risk of malignancy that approximates that for adults with dermatomyositis. The risk is particularly high in the first year of disease.
Patient Education
Be certain that patients understand the chronic nature of this disorder.
Help patients in identifying factors that precipitate disease activity, and instruct them to avoid conditions that exacerbate the condition.
Discuss the medications, including the dose, the adverse effects, and the symptoms of toxicity, with the patient.
Teach patients appropriate wound care.
-
Ocular manifestations of cicatricial pemphigoid (mucous membrane pemphigoid) include symblepharon, demonstrated in this photograph by the tethering of the lower lid to the cornea.
-
In a patient with more advanced ocular scarring, note the thickening of the lid margins, shortening of the conjunctival sulcus, and scarring. The eyelashes have been epilated after entropion developed.
-
By direct immunofluorescence, a linear band of immunoreactants at the epidermal-dermal junction is demonstrated by using a fluorescein-tagged antibody specific for human immunoglobulin G.
-
With advanced disease, ankyloblepharon (a fixed globe) develops.





