Background
Melanoacanthoma is a rare condition of oral mucosa that has been reported only in the last century. The lesion is characterized by a proliferation of both melanocytes and keratinocytes that results in pigmented macular or plaquelike lesions (see image below).
Oral melanoacanthoma is regarded by many as a reactive condition unrelated to cutaneous melanoacanthoma, but the histologic features are similar. Cutaneous melanoacanthoma and mucosal melanoacanthoma differ in terms of patient age, patient race, and site.
Early publications
In 1927, Bloch provided the earliest known description of melanoacanthoma, which was reported in the German literature. [1] Bloch described several skin lesions, which he originally called benign nonovoid melanoepithelioma of the skin. He further subdivided his cases into two types. In the histologic samples studied, type 1 had both dendritic melanocytes and keratinocytes, whereas the histologic appearance of type 2 was similar to that of type 1, but it lacked the dendritic melanocytes.
In 1960, Mishima and Pinkus reexamined the condition and further refined the diagnostic terminology. [2] The condition that Bloch designated as type 1 is currently called melanoacanthoma, and type 2 is currently called pigmented seborrheic keratosis. [3]
Although cutaneous lesions of melanoacanthoma were reported as early as 1927, Tomich et al at the American Academy of Oral Pathology first reported oral mucosal lesions in 1978. [1] Although many authors subsequently published case reports, Goode et al published the first case report in 1983. [4] This was a retrospective review of 10 cases of oral melanoacanthoma reported in the literature.
Oral melanoacanthoma continues to be listed as a rare condition. While some studies report approximately fewer than 100 reported cases, it would be legitimate to point out that the low case published reports may be attributed to the benign nature of lesion appearance, rate and timing of manifestations, and potential differential diagnosis of amalgam tattoo, for example, which though common, are not routinely reported nor typically addressed with treatment owing to the location of the lesion and treatment options.
The cutaneous variant is also rare; however, it has been suggested it is more prevalent than the mucosal variant. This variance in observation of data may be due to differential diagnosis options and subsequent interest in case reporting, as well as by the patient motivation, with potential patient action biased by treatment selection for aesthetic considerations.
Pathophysiology
The mucosal variants of melanoacanthoma have histologic appearances similar to those of cutaneous melanoacanthoma. The lesion consists of proliferating melanocytes and keratinocytes, which result in large pigment-containing dendritic cells. The dendritic cells are present throughout the middle and upper layers of the epithelium. See the image below.
Inflammation occurs almost universally in patients with mucosal lesions. The presence of inflammation and the spontaneous resolution of oral lesions are suggestive of a reactive process rather than a neoplastic process. [5] The observation of trauma and inflammation associated with oral lesions has led to the conclusion that the mucosal variant is likely the result of a reactive process rather than a neoplastic process. [6]
Etiology
The role of trauma in the development of the lesion remains controversial, but any irritant must be removed. BRAF inhibitor therapy may play a role in some cases. [7] Some data suggest the close resemblance in the pattern of pathophysiological development shared with amalgam tattoos or other external or internal stimulants as reactive-induced lesions, including comorbidities, leaving the location and the rate of presentation as the first clinical differentiating factors.
Epidemiology
US frequency
Oral melanoacanthoma is rare, with only approximately fewer than 100 cases reported since 1978, [8, 9, 10] when the lesions were first reported. The cutaneous variant is more common, but it is still relatively rare among skin lesions. Among all the cases reported, specific patterns are described with respect to the race, sex, and age of patients with cutaneous melanoacanthoma and those with mucosal melanoacanthoma.
Race
Cutaneous lesions of melanoacanthoma are reported almost exclusively in White patients. The mucosal variant is reported almost exclusively in Black patients, [11, 12] with higher rates reported in women. Some sporadic mucosal cases are reported in Asian individuals.
Sex
The prevalence for both variants of melanoacanthoma is fairly equal in both sexes, with a slight female predominance. [13] The female-to-male ratio is approximately 3:2.
Age
The age distributions of the two types of melanoacanthoma differ. [14] Cutaneous lesions are found in patients with a mean age of approximately 60 years. Mucosal lesions appear in patients with a mean age of approximately 25 years.
Prognosis
Prognosis with treatment intervention can vary, for example by blade surgical excision, laser surgery, or other treatment options. More studies are needed to differentiate optimal outcomes with a minimally invasive approach.
Initially, cutaneous lesions were suspected to be malignant, and, subsequently, the lesions were linked to a transformation to low-grade malignancy. Malignant transformation has been reported in at least two cases. However, most lesions are considered benign and should be treated conservatively. Clinical data collection supported by histopathology reports can substantiate a better prognosis.
No cases of recurrence or metastasis have been reported in either the mucosal variant or cutaneous variant. A low risk of recurrence exists. To date, no malignant oral melanoacanthoma have been reported.
Patient Education
Patient observation and regular monitoring and screening of the cutaneous and oral mucosal lesion classifications are easily established in the dermatologic and dental routine evaluation protocols. Subsequent comprehensive patient education on findings and appropriate recall can be enhanced by etiologic diagnosis of lesion, and proved by histological report.
-
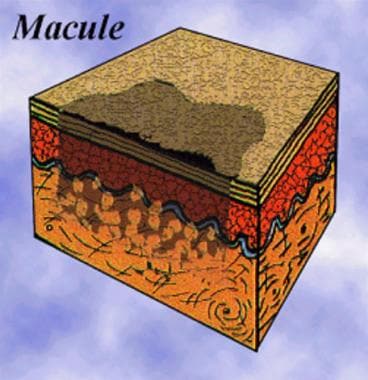
Diagram of a pigmented epithelial macule.
-
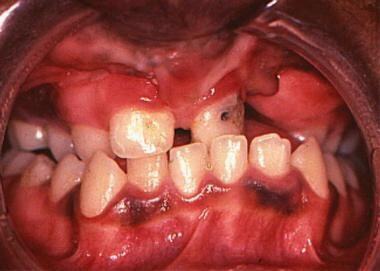
Intraoral melanoacanthoma lesion on the mandibular gingiva.
-
Increased melanin pigmentation in the basal layer of a melanoacanthoma (hematoxylin and eosin, original magnification X10).
-
Proliferating dendritic melanocytes in the prickle-cell layers of a melanoacanthoma (hematoxylin and eosin, original magnification X40).