Overview
Members of the human herpesvirus (HHV) and human papillomavirus (HPV) families cause the most common primary viral infections of the oral cavity. HPV infections have received particular attention in recent years, as high-risk strains have been linked to some cases of oral squamous cell carcinoma. Nonetheless, many other viral infections can affect the oral cavity in humans, either as localized or systemic infections. This article discusses viral conditions of the oral cavity, including HHV infection, HPV infection, coxsackievirus infection, mumps, measles (rubeola), and rubella. See Cutaneous Manifestations of HIV Disease and Cutaneous Manifestations of Hepatitis C for information on these viral infections.
For patient education resources, visit the Oral Health Center and Infections Center. Also, see the patient education articles Oral Herpes, Canker Sores, Measles, Mumps, Chemical Burns, and Allergic Reaction.
Human Herpesvirus
Background
HHV infections are common in the oral cavity. They may be primary or recurrent infections. Eight types of HHV have been linked with oral disease. These types have different disease patterns in their hosts.
-
HHV-1, also known as herpes simplex virus (HSV)–1, causes primary herpetic gingivostomatitis, or oral herpes. In some hosts, it becomes latent and may periodically recur as a common cold sore.
-
HHV-2, also known as HSV-2, causes genital herpes and occasionally causes oral disease that is clinically similar to that of HHV-1 infection.
-
HHV-3, also known as varicella-zoster virus (VZV), causes the primary infection chickenpox and the secondary reactivation disease herpes zoster.
-
HHV-4, also known as Epstein-Barr virus (EBV), causes the primary infection infectiousmononucleosis, and it is implicated in various diseases, such as AfricanBurkittlymphoma, other immunoproliferative disorders, and nasopharyngeal carcinoma. HHV-4 causes oral hairy leukoplakia in patients who are immunosuppressed. [1]
-
HHV-5, also known as cytomegalovirus (CMV), causes a primary infection of the salivary glands and other tissues, and it is believed to have a chronic form.
-
HHV-6, which can produce acute infection in CD4+ T lymphocytes, causes roseola infantum, a febrile illness that affects young children. It is believed to chronically persist in salivary gland tissue in some hosts, and oral shedding is the probable route of disease transmission. Although it has been linked to apical periodontitis in some studies, the evidence so far is mixed, so such an association remains currently unproved. [2, 3, 4]
-
HHV-7 has been isolated from the saliva of healthy adults and has been implicated as one cause of roseola infantum and febrile seizures in children.
-
HHV-8 is associated with Kaposi sarcoma (KS), and evidence links it with body-cavity lymphomas and Castleman disease.
Pathophysiology
Herpesvirus family members are icosahedral DNA viruses. A herpesvirus measures approximately 100 nm without an envelope or 150 nm with an envelope. HHVs replicate in the host cell nucleus. Infected saliva or droplets spread the viruses in the oral cavity. The viruses also may be transmitted via oral-genital contact. Viral shedding has been detected before, during, and after the appearance of clinical lesions in patients with recurrent HHV-1 and HHV-2 infections; therefore, lack of visible lesions does not correlate with lack of potential infectivity. [5, 6] In a localized primary infection, the virus penetrates the mucosal epithelium and invades the cells of the basal layer, where the viral DNA inserts into the host DNA.
In HHV-1 and HHV-2 oral infections, viral replication within the oral epithelium may cause lysis of epithelial cells, with vesicle formation. Shallow ulcers with scabs that then heal without scarring follow the formation of vesicles. Herpesviruses establish latent permanent infections in their hosts, although clinical signs of disease may not be detected.
Frequency
Frequency statistics are as follows:
-
HHV-1: The seroprevalence is approximately 80% in North American adults.
-
HHV-2: The seroprevalence is approximately 20% in North American adults.
-
HHV-3: The seroprevalence is approximately 95% in North American adults.
-
HHV-4: The seroprevalence is approximately 90% in North American adults.
-
HHV-5: The seroprevalence is approximately 70% in North American adults.
-
HHV-6: The seroprevalence approaches 100% in North American adults. [7]
-
HHV-7: The seroprevalence is approximately 85% in adults.
-
HHV-8: The global seroprevalence is estimated at 2-10%, although it has been demonstrated to be greater than 28% in Albanian adults, 25% in Albanian children, 18% in Kosovar adults, and greater than 16% in Kosovar children. [8]
Mortality/morbidity
In children and adults who are immunocompetent, primary herpetic infections may be annoying and uncomfortable, but they rarely cause significant morbidity or mortality.
In individuals who are immunosuppressed, primary herpetic infections can be severe, and, occasionally, they can cause esophagitis, encephalitis, keratoconjunctivitis, and other diseases. The other forms of HHV can result in death. Herpes infections occasionally trigger erythema multiforme.
Age
Primary herpes infections typically occur during childhood or youth, although occasional cases are observed in older individuals. Recurrent HHV-1 infections typically occur throughout life and are particularly triggered by stress, illness, immune compromise, or other factors. Herpes zoster usually affects patients older than 40 years, and has similar triggers, although triggering conditions usually need to be more profound.
Clinical history for HHV-1
HHV-1 is also known as Herpes Simplex Virus Type 1, or Oral Herpes Virus. Primary herpetic gingivostomatitis has different and distinct oral and perioral presentations from subsequent recurrences of HHV-1 disease.
Primary herpes infection (primary herpetic gingivostomatitis) usually occurs in children or adolescents who have not been previously exposed to the virus. Many primary infections are asymptomatic. Symptomatic primary infection, with multiple, small, clustered vesicles in numerous locations, can occur anywhere in the oral cavity, on the perioral skin, on the pharynx, or on the genitalia. Headache, fever, painful lymphadenopathy, and malaise are common. Antibody production follows, and the virus may become latent in sensory ganglia, often the trigeminal ganglion. Primary herpetic gingivostomatitis usually resolves within approximately 14 days.
Recurrent herpes lesions are commonly referred to as cold sores. Recurrent herpes occurs in approximately one third of patients who have experienced primary herpetic gingivostomatitis. When the disease manifests extraorally, prodromal burning or itching often precedes vesicle formation. Recurrent herpes is a more limited disease than primary herpes. Unlike primary herpes, it occurs on keratinized mucosa (usually the lips, attached gingiva, and/or the hard palate). Vesicles are present in one discrete area, typically the same site every time in any given patient. Such sites include the vermilion border of the lips, the perioral skin, the hard palate, or, occasionally, the gingiva or the dorsal aspect of the tongue. One case report describes HHV-1 infection manifesting as a mass in the piriform sinus. [9] Because vesicles can easily rupture intraorally, only an ulcer may be observed in some cases. Lymphadenopathy and systemic manifestations are much milder than in the primary disease.
Triggers for recurrence may include sunlight exposure, physical or emotional stress, or systemic illness for extraoral lesions. Trauma (eg, a dental procedure) is sometimes a trigger for intraoral lesions.
In immunosuppressed individuals, recurrent herpes lesions may occur on any oral mucosal surface, including nonkeratinized sites. They also may manifest solely as lesions on the dorsal aspect of the tongue. Such a presentation has been variously reported as red or white nodules, painful nonvesicular ulcerations, fissured, and, rarely, as a tongue mass. [10] Herpes lesions in immunocompromised individuals are often severe. Such atypical presentations in an individual who is immunocompetent may lead the clinician to further investigate the patient's immune status.
See the images below.
 Human herpesvirus (HHV) type 1. Primary herpetic gingivostomatitis often affects children or young adults. The initial clinical presentation can be severe, with vesicles throughout the oropharynx and perioral skin, in contrast to the much more limited presentation typical of recurrent herpes. Courtesy of A.K. ElGeneidy, DDS.
Human herpesvirus (HHV) type 1. Primary herpetic gingivostomatitis often affects children or young adults. The initial clinical presentation can be severe, with vesicles throughout the oropharynx and perioral skin, in contrast to the much more limited presentation typical of recurrent herpes. Courtesy of A.K. ElGeneidy, DDS.
 Human herpesvirus (HHV) type 1. Additional intraoral view of the same patient in Image 1. Note the redness around the marginal gingiva, representing healing ulcers, which days earlier would have appeared as vesicles. This extensive ulceration often makes eating painful. Courtesy of A.K. ElGeneidy, DDS.
Human herpesvirus (HHV) type 1. Additional intraoral view of the same patient in Image 1. Note the redness around the marginal gingiva, representing healing ulcers, which days earlier would have appeared as vesicles. This extensive ulceration often makes eating painful. Courtesy of A.K. ElGeneidy, DDS.
 Human herpesvirus (HHV) type 1. Primary herpes can affect the lips, and the ruptured vesicles may appear as bleeding of the lips (same patient as in Images 1-2). Courtesy of A.K. ElGeneidy, DDS.
Human herpesvirus (HHV) type 1. Primary herpes can affect the lips, and the ruptured vesicles may appear as bleeding of the lips (same patient as in Images 1-2). Courtesy of A.K. ElGeneidy, DDS.
 Human herpesvirus (HHV) type 1. Recurrent herpes is most often noted clinically as herpes labialis, with clustered vesicles (often coalescing) on the lip vermilion and often on the perioral skin. Recurrences generally occur in the same area each time, although their severity may vary.
Human herpesvirus (HHV) type 1. Recurrent herpes is most often noted clinically as herpes labialis, with clustered vesicles (often coalescing) on the lip vermilion and often on the perioral skin. Recurrences generally occur in the same area each time, although their severity may vary.
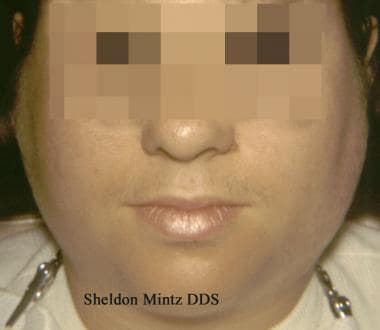
 Human herpesvirus (HHV) type 1. Recurrent herpes is occasionally observed intraorally. Inside the oral cavity, recurrent herpes typically affects only keratinized tissues, such as the gingiva or the hard palate. Vesicles often break quickly, so the clinician may observe small clustered ulcers. Courtesy of Sheldon Mintz, DDS.
Human herpesvirus (HHV) type 1. Recurrent herpes is occasionally observed intraorally. Inside the oral cavity, recurrent herpes typically affects only keratinized tissues, such as the gingiva or the hard palate. Vesicles often break quickly, so the clinician may observe small clustered ulcers. Courtesy of Sheldon Mintz, DDS.
Clinical history for HHV-2
HHV-2 is also known as herpes simplex virus type 2, or genital herpes virus. HHV-2 infection is less common in the oral cavity than HHV-1 infection; however, its oral manifestations are clinically indistinguishable from HHV-1 infection. [11] Assessment of HSV-2 shedding by polymerase chain reaction has detected oral HSV-2 shedding in the absence of an oral lesion, but concurrent with genital HSV-2 reactivation. This was more common in HIV-positive males.
Clinical history for HHV-3
HHV-3 is also known as varicella-zoster virus. HHV-3 is responsible for chickenpox and shingles.
Primary varicella, or chickenpox, usually occurs in children aged 3-6 years who are not immunized at the time of their first exposure to the virus. Itchy vesicles begin on the skin of the trunk and spread to the skin of the head. Intraoral and pharyngeal vesicles may occur. Antibody production follows, and the virus usually becomes latent in the dorsal root ganglia. Healthy children usually recover uneventfully, with a mortality rate of fewer than 2 deaths per 100,000 cases. However, older patients may experience more severe symptoms, and, in patients who are immunocompromised, the mortality rate may approach 18%.
Recurrent varicella, also known as herpes zoster or shingles, usually occurs in adults, and its incidence increases with age. It can occur in any patient who has had chickenpox and only rarely occurs in patients who have received chickenpox immunization. Recurrent varicella may occur when cellular immunity decreases. It results in a vesicular rash that usually affects a single dermatome. Inside the oral cavity, this may be observed as vesicles or ulcerations that stop sharply at the midline. A prodrome of pain, burning, or itching that mimics a toothache may occur.
After resolution of the rash, postherpetic neuralgia may linger for a month or longer, especially in patients who are immunosuppressed or in those older than 50 years.
Unusual complications can include devitalization of teeth, root resorption, osteonecrosis, and root resorption. [12]
Ramsay-Hunt syndrome arises when the virus emerges from latency in the geniculate ganglion. It involves cranial nerve VII (facial nerve), which has both motor and sensory functions. Manifestations may include paralysis that involves the levator palati muscle and the face; hoarseness; loss of secretory function (eg, dry mouth, loss of taste); vertigo; tinnitus; pain; and vesicles involving the pharynx, the eardrum, the external ear, or the tympanic membrane. Persistent facial nerve weakness or deafness may follow.
 Human herpesvirus (HHV) type 3. The initial manifestation of Varicella-Zoster Virus infection is chickenpox (varicella), and vesicular lesions may be noted on the oral mucosa in addition to the characteristic and better-known skin lesions.
Human herpesvirus (HHV) type 3. The initial manifestation of Varicella-Zoster Virus infection is chickenpox (varicella), and vesicular lesions may be noted on the oral mucosa in addition to the characteristic and better-known skin lesions.
 Human herpesvirus (HHV) type 3. Intraoral herpes zoster closely resembles recurrent HHV-1 infection, but the lesions generally follow a dermatome and stop sharply at the midline, as shown here. However, the rules for common sites of occurrence of HHV-1 and HHV-3 often do not apply to patients who are immunocompromised. Courtesy of Sheldon Mintz, DDS.
Human herpesvirus (HHV) type 3. Intraoral herpes zoster closely resembles recurrent HHV-1 infection, but the lesions generally follow a dermatome and stop sharply at the midline, as shown here. However, the rules for common sites of occurrence of HHV-1 and HHV-3 often do not apply to patients who are immunocompromised. Courtesy of Sheldon Mintz, DDS.
Clinical history for HHV-4
HHV-4 is also known as Epstein-Barr virus. HHV-4 is most commonly known as the agent that causes infectious mononucleosis, although it has been linked to African Burkitt lymphoma, other lymphoproliferative diseases, and some nasopharyngeal carcinomas.
Primary infection, infectious mononucleosis (colloquially referred to as “mono” or “kissing disease”), occurs on first exposure to the virus, usually during young adulthood. It is often a subclinical infection. The virus (usually acquired from infected saliva) replicates in the cells of the mucosa and salivary glands and spreads to B lymphocytes and the bloodstream. If the patient is immunocompetent, cytotoxic T cells become activated and a characteristic lymphadenopathy (notably involving the posterior cervical nodes) accompanies tonsillitis and hepatosplenomegaly. Tonsillitis may be severe and may encroach on the airway. Thrombocytopenia may complicate the infection, and petechiae may be noted at the junction of the hard and soft palates. The patient may report headache, fever, malaise, myalgia, and fatigue. Severe abdominal pain may indicate splenic rupture.
See the image below.
Latent infection of B lymphocytes follows acute disease. EBV has been detected in saliva as long as 18 months after recovery from clinically evident disease.
Hairy leukoplakia, caused by HHV-4, primarily occurs in adults who are immunosuppressed. Hairy leukoplakia manifests as asymptomatic white lesions on the lateral border of the tongue, often bilaterally. The lesions may be observed on the adjacent dorsal or ventral surface of the tongue. Occasionally, lesions are present in other sites, such as the buccal mucosa near the commissures. The lesions have a corrugated, linear appearance and may appear granular or nodular or may have hairlike projections. Hairy leukoplakia may be the first manifestation of immunosuppression and may prompt the clinician to test the patient's HIV status. The presence of hairy leukoplakia is significantly associated with an HIV viral load of at least 3000 copies/μL, although a diagnosis of hairy leukoplakia is not synonymous with a diagnosis of HIV as it can be associated with immunosuppression due to other causes. [13, 14, 15]
HHV-4 has been detected in aggressive periodontal lesions more often than in less diseased periodontal tissues, and it has also been detected in periapical lesions. The significance of these findings is unclear. [16, 17, 18] There is evidence that some malignancies of the base of the tongue and tonsillar regions may be associated with HHV-4 and human papillomavirus (HPV) co-infection. [19]
Clinical history for HHV-5
HHV-5 is also known as cytomegalovirus. Primary HHV-5 infection is usually asymptomatic in patients who are immunocompetent. The virus is shed by glandular secretions, including saliva. It occasionally is shed in urine. Primary HHV-5 infection can be asymptomatic, but it can also mimic mononucleosis. Clinical disease is more common in neonates and in patients who are immunosuppressed than in other individuals.
HHV-5 can persist indefinitely in the host. Reactivation of latent infection can occur in patients who are immunosuppressed, including most patients who have undergone organ transplantation and as many as 90% of patients with AIDS. Latent HHV-5 infection may cause esophagitis, which is occasionally accompanied by oral ulcerations or erythema. The disease can also affect many other body systems, including the colon, eyes, liver, lungs, or brain. The oral ulcerations are clinically nonspecific, and a biopsy is required for definitive diagnosis. A patient with HIV infection who develops HHV-5 oral ulcerations is at high risk for progression to AIDS.
Congenital HHV-5 infection affects 0.5-2.2% of newborns. It is frequently asymptomatic, but oral manifestations may include enamel hypoplasia of the primary teeth.
Clinical history for HHV-7
HHV-7 infection has been associated with roseola infantum, acute hemiplegia of childhood, respiratory tract infections, and hepatitis. [20, 21] It has also been linked to seizures in children with febrile illnesses. HHV-7 has been identified in the saliva of adults, and this is most likely where the virus persists chronically.
Clinical history for HHV-8
HHV-8 is also known as KS-associated herpesvirus, because DNA sequences of HHV-8 have been identified in persons with Kaposi sarcoma (KS), and, therefore, it is believed to be important in causing and/or maintaining KS lesions. KS in the oral cavity follows the same disease pattern as KS in other body sites. Initially, the lesion may appear as a red, purple, or dusky patch that enlarges into a plaque and later progresses into a tumorous mass. It is observed most frequently in immunosuppressed patients and rarely occurs in children. In the oral cavity, early KS may mimic an amalgam tattoo. The palate is the initial site of intraoral KS in approximately half the cases; other favored sites include the gingiva, the tongue, and the tonsillar area. [22, 23]
Differentials for primary herpetic gingivostomatitis
See the list below:
-
Herpetiform aphthae
-
Acute necrotizing gingivostomatitis
-
Factitial injuries
-
Vesiculobullous disease
-
Primary chickenpox
Differentials for recurrent herpetic gingivostomatitis
See the list below:
-
Primary herpetic gingivostomatitis
-
Herpetiform aphthae
-
Aphthous minor
-
Acute necrotizing gingivostomatitis
-
Factitial injury
-
Herpangina
-
Vesiculobullous disease
-
CMV ulceration
-
Deep fungal infection
-
Foreign body reaction
Differentials for hairy leukoplakia [24, 25]
-
Traumatic keratosis (tongue chewing)
-
Epithelial dysplasia
Differentials for oral KS
See the list below:
-
Amalgam tattoo
-
Other tattoo
-
Hemangioma
-
Varix
-
Nevocellular nevus
-
Ecchymosis
Imaging studies
Radiography of suspected early KS may be useful to differentiate it from an amalgam tattoo. In many amalgam tattoos, the amalgam is visible as discrete radiopaque particles.
Procedures
Diagnosis is often made based on the clinical findings alone, especially for HHV-1, HHV-2, and HHV-3. A smear of an intact viral vesicle may be helpful to confirm the clinical diagnosis. Smear results may reveal virally altered epithelial cells. Direct immunofluorescence antibody tests and culturing help identify the causative virus. A person who is infected initially has an IgM response followed by an immunoglobulin G (IgG) response. Biopsy is usually required to confirm a diagnosis of KS, and it may be required to confirm the diagnosis of other conditions. Quantitative polymerase chain reaction may serve useful for detection of HHV-8 in whole blood or in tissues. [26]
Histologic findings
HHV-1 and HHV-2 infections are characterized by acantholytic intraepidermal vesicles with epithelial giant cells. The cells exhibit nuclear molding and peripheral accentuation of the nucleoplasm. Underlying leukocytoclastic vasculitis is typically present.
HHV-3 infection has similar findings, but the leukocytoclastic vasculitis is more pronounced.
HHV-4 infection manifests as enlarged endothelial cells. An infected cell typically has ample cytoplasm and an owl’s eye nucleus.
KS is a neoplastic spindle cell proliferation with erythrocytes in slitlike spaces and extravasation of the erythrocytes between the neoplastic cells.
General medical care
Establishing the diagnosis is important because the differential diagnoses include diseases that are conventionally treated with immunosuppressive agents. Immunosuppressive therapy may not be prudent for an active herpetic infection because it could promote dissemination.
Herpesvirus infections may trigger erythema multiforme. If recurrences are common and debilitating, long-term suppressive antiviral therapy may reduce the recurrence of herpes and thus erythema multiforme. [27]
Patients should be counseled about the routes of infectivity.
Medical care for primary HHV-1/HHV-2
The goals of treatment are to make the patient comfortable and to prevent secondary infections or worsening systemic illness. The patient should maintain fluid intake and a balanced diet with the use of liquid food replacement if necessary. Analgesics, such as acetaminophen, may make the patient more comfortable. Aspirin should be avoided in pediatric patients because of the possibility of Reye syndrome. Topical anesthetics and coating agents may make the patient more comfortable and may aid in the consumption of food; however, they do not speed healing.
Patients should be advised about the potential for autoinoculation if they touch the herpetic lesion and then touch a mucous membrane or an eye. Controlling autoinoculation can be a challenge if the patient is a young child.
Medical care for recurrent orofacial HHV-1/HHV-2
Some patients find that sunburn triggers the recurrence of labial lesions. Sun avoidance with the use of hats or shading or the application of a sunscreen or sunblock may reduce the frequency of recurrences. [28, 29]
If the decision is made to use systemic antiviral treatment, it should be initiated as early as possible in the prodromal stage to reduce the size, severity, and duration of the lesions. Topical antiviral medications are minimally useful in treating recurrent HHV-1 infection in healthy patients. Emollient preparations may make the patient more comfortable. Systemic prophylactic antiviral medication may be indicated for patients who experience 6 or more recurrences a year or for patients who experience repeated bouts of erythema multiforme induced by herpes. [30]
Medical care for HHV-3 (varicella-zoster virus)
Antiviral therapy is most effective in limiting the area of involvement and the duration of the symptoms if instituted within the first 48-72 hours. Acyclovir may control the size of the lesions, but it is less effective than valacyclovir or famciclovir in reducing pain and in lessening the risk of postherpetic neuralgia. Postherpetic neuralgia is especially common in older patients, and it may be appropriately managed with short-term, high-dose corticosteroid prophylaxis in conjunction with or following antiviral therapy. The pain of postherpetic neuralgia can also be managed with anticonvulsants, antidepressants, painkillers, or topical anesthetics. [31]
Prevention of chicken pox/varicella infection can be accomplished via vaccination. Two vaccines are available in the United States for the prevention of varicella infection. The first is a single-antigen varicella vaccine (Varivax; Merck & Co), which was licensed in 1995 in the United States. It is indicated for use in healthy children older than 12 months, adolescents, and adults. The second vaccine is a combination of the measles, mumps, rubella, and varicella components (ProQuad; Merck & Co), which was licensed in 2005 in the United States for use in children aged 12 months to 12 years. [32] A new vaccine to prevent herpes zoster, Shingrix, was licensed in the United States in 2017 and is preferred over its predecessor, Zostavax, which had been used since 2006. [33]
The following are the Advisory Committee on Immunization Practices recommendations for varicella vaccine [34, 35, 36, 37] :
-
Routine 2-dose varicella vaccination regimen for children, with the first dose given at age 12-15 months and the second dose given at age 4-6 years
-
Second catch-up dose of varicella vaccine for children, adolescents, and adults who previously received 1 dose
-
Routine vaccination of all healthy individuals aged 13 years or older who do not have evidence of immunity
-
Prenatal assessment and postpartum vaccination
-
Varicella vaccination of HIV-infected children with age-specific CD4+ T lymphocyte percentages of 15-24% and adolescents and adults with CD4+ T lymphocyte counts equal to or greater than 200 cells/μL
-
Establishing middle school, high school, and college entry vaccination requirements
The new zoster vaccine, Shingrix, can reduce the likelihood of herpes zoster and its complications, including postherpetic neuralgia. The US Centers for Disease Control and Prevention (CDC) recommend two doses of Shingrix separated by 2-6 months for immunocompetent adults aged 50 years and older, although it should not be given to someone who is experiencing an active attack of herpes zoster. It may be given to patients who have previously received the older Zostavax vaccine. [38] For a commentary, see "Shingles and Shingles Vaccine: An Update”.
Persons with either varicella or zoster may benefit from oral antiviral drugs.
Medical care for HHV-4 (EBV)
Topical tretinoin gel may be used to manage oral hairy leukoplakia, but it often is not necessary. Topical podophyllin applications (a keratotic agent) may help to control HHV-4-associated hairy leukoplakia. Repeated treatment may be necessary to obtain satisfactory results. Management of the underlying immunosuppressed status may be a more useful strategy. Occasionally, the use of systemic antiviral medication may be warranted. Potential toxicity, adverse effects, and complications of systemic therapy combined with a high risk of lesion reappearance and the benign nature of hairy leukoplakia support a conservative approach in the management of hairy leukoplakia.
Medical care for HHV-5 (CMV)
Similar to HHV-1/HHV-2, HHV-5-related ulceration of the oral cavity requires immediate referral to an ophthalmologist if ocular involvement is of concern. Systemic antiviral treatment (ie, with ganciclovir or valganciclovir) is the treatment of choice for oral lesions.
Medical care for HHV-8
Patients diagnosed with HHV-8–associated KS should be referred to a health care provider experienced in the treatment of this disease. The best results in the treatment of KS are achieved by improving systemic immune functions. When limited to the oral cavity, low-dose radiation therapy, intralesional injections of vinblastine and/or sodium tetradecyl sulfate (Sotradecol), and/or interferon alfa (IFN-A) have been reported to result in the resolution of the lesions. [39]
Consultations
Patients with ocular lesions should be immediately referred to an ophthalmologist.
Patients with KS are commonly referred to an appropriate subspecialist for treatment.
Patients with confirmed hairy leukoplakia or KS should undergo a thorough investigation of their immune status.
Medication
See Medication.
Medical/legal Pitfalls
Note the following medicolegal pitfalls:
-
Failure to inform the patient of the potential for disease transmission
-
Failure to search for underlying immunosuppression, if appropriate
-
Failure to make necessary medical referrals
-
Failure to indicate treatment availability
Human Papillomavirus
Background
HPVs are members of the Papovaviridae family, which are small icosahedral viruses that contain circular DNA. The term papova is derived from the first 2 letters of their common clinical features, as follows: papillomatous lesions, polyomas (varied tumor induction), and vacuolization of infected cells. [40]
Well over 100 types of HPV have been discovered. The infectivity of HPV is incompletely understood. Some types of HPV may act in concert with cofactors such as diminished immunity, tobacco use, or sun exposure. [41]
HPV may have a role in oral premalignancy and malignancy in humans. [42, 43, 44, 45] HPV is capable of integration into the host’s HPV is capable of integration into the host’s HPV is capable of integration into the host’s genome, and this can result in the loss of normal controls over cellular proliferation. HPVs may interfere with the normal function of regulatory proteins, such as p53, p16, and pRb, and they may have a promoter effect. Most types of HPV are considered to be “low-risk” for the subsequent development of malignancy, but about 13 types are considered “high-risk”. [46, 47, 48, 49] For example, skin warts are caused by low-risk HPV types and are not associated with increased risk of malignancy; they affect 7-12% of humans. [50]
HPV-16 in particular (but also HPV-18, HPV-33, HPV-35, and others) have been associated with verruciform proliferations in the oral cavity, oral premalignant lesions, and oral squamous cell carcinoma. [51, 52, 53, 54, 55, 56] Although the magnitude of its risk is not completely clear, high-risk HPV is currently considered to be an independent risk factor for the development of oral squamous cell carcinoma, especially in younger cancer patients and persons with tonsillar carcinoma. Odds ratios range in various studies from 2.0 to 5.4, and variation is in part associated with the method of viral detection. Certain HPV types have been more strongly associated with malignancies of the tonsils, anus, genital tract, and other areas.
In accordance with other studies, lifestyle parameters, including recent or life-long number of sexual and oral-sexual partners, predicted a higher risk for the presence of HPV in oral rinses. [57, 58]
Pathophysiology
HPV is a 50-nm virus composed of double-stranded DNA with no envelope. The virus penetrates the mucosal epithelium and invades the cells of the basal layer, where the viral circular DNA inserts into the host DNA.
Frequency
HPV has been detected in the oral cavity of approximately 6-10% of children and adolescents. The rate of HPV in the oral cavity of healthy adults is estimated at 5-80%. Persistent oral HPV infection in one spouse appears to predict similar infection in the other spouse, regardless of oral sex habits. [59, 60, 61, 62] There is conflicting evidence whether oral HPV infection may denote an increased risk of vaginal HPV infection and vice-versa. [63, 64]
In a landmark cross-sectional study, Gillison et al reported the prevalence of HPV in oral rinses collected from 5579 men and women aged 14-69 years. The overall prevalence of HPV approached 7%. The prevalence of HPV-16 subtype, the overwhelmingly relevant subtype for oral cancer, was around 1%. [65] A study of Northern Italian men who have sex with men found much higher levels of oral HPV detected by PCR: about 21% of the men had HPV and about 24% of these men had high-risk HPV. [66]
HPV-16 has been linked to the development of dysplasia and carcinoma of the uterine cervix. Oral HPV-16 detection is more common in women with HPV-associated cervical dysplasia. [67] Oral HPV-16 detection is much less common in children than in adolescents and adults. However, persistence of HPV-16 and other high-risk HPV types is more common in infants of parents with persistent oral HPV infections and high-risk behaviors.
The presence of HPV in oropharyngeal cancers is believed to be on the rise. This may be more pronounced in HIV-positive patients. [68] The presence of HPV in these types of cancer is a predictor of a better prognosis when compared with tumors in which HPV cannot be detected. [69, 70]
HPV lesions are more common in immunocompromised patients, especially in HIV-infected patients and in solid organ transplant recipients. [71, 72] Oral HPV may also be more common in renal dialysis patients. The recent development of effective preventive HPV vaccines may, in the future, have a significant impact on these rates. [73, 74, 75]
Mortality/morbidity
Most oral lesions caused by HPV are benign. Lesions are usually painless and not ulcerated, although they may be secondarily ulcerated by trauma. Lesions may be more common and severe in immunocompromised patients than in other patients.
Clinical History
Verruca vulgaris, or common warts (HPV-2; HPV-4; occasionally HPV-1, HPV-3, HPV-27, HPV-29, and HPV-57), are more common on the skin than in the oral cavity. [76, 77] On the oral mucosa, the warts are usually sessile, verrucous, and white; solitary or multiple; and elevated with discrete borders. The lesions most commonly occur on the lips, hard palate, or gingiva. Verruca plana is similar but less elevated. Warts are commonly observed on the digits of patients with oral infection.
Condyloma acuminata, or genitalwarts (usually HPV-6, HPV-11; occasionally HPV-30, 40, 42, 43, 44, 45, 51, 52, 54, 61, 70, 72, and 81), may affect the oral mucosa as well as the genitals, perianal region, larynx, or trachea. [78, 79] These lesions are usually cerebriform, pink, and sessile and solitary or multiple; they occur more commonly on nonkeratinized mucosa than on keratinized mucosa. Patients infected with HPV-6 or HPV-11 and their sexual partners may have genital lesions, and the lesions have presumably been spread to the oral cavity via oral-genital contact.
Focal epithelial hyperplasia, or Heck disease (HPV-13, HPV-32), may appear as an epidemic in young adults in small communities. This condition was first described in native North American people. Heck disease typically manifests as multiple, smooth, sessile nodules, often on the mucosal surface of the lower lip or on the buccal mucosa. Lesions may regress spontaneously after a number of months. [80, 81, 82]
HPV may have a role in oral premalignancy and malignancy in humans. [30, 31] HPV-16 in particular (but also HPV-18, HPV-33, HPV-35, and others) have been associated with verruciform proliferations in the oral cavity, oral premalignant lesions, and oral squamous cell carcinoma. [32, 34, 35, 36] HPVs may interfere with the normal function of regulatory proteins, such as p53, p16, and pRb, and they may have a promoter effect.
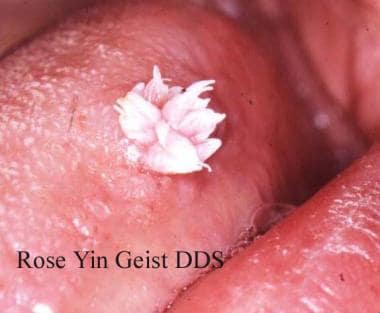 Human papillomavirus (HPV). Verruca vulgaris on the lateral border of the tongue exhibits the multiple, sharp-tipped, white, verrucous appearance, which is classic for this lesion in the oral cavity. Not all verrucae are so clinically diagnostic. Courtesy of Rose Yin Geist, DDS.
Human papillomavirus (HPV). Verruca vulgaris on the lateral border of the tongue exhibits the multiple, sharp-tipped, white, verrucous appearance, which is classic for this lesion in the oral cavity. Not all verrucae are so clinically diagnostic. Courtesy of Rose Yin Geist, DDS.
 Human papillomavirus (HPV). This verruca on the retromolar pad shows much less keratinization and a broader base. Verrucae and papillomas may be difficult to differentiate, but both are usually surgically excised.
Human papillomavirus (HPV). This verruca on the retromolar pad shows much less keratinization and a broader base. Verrucae and papillomas may be difficult to differentiate, but both are usually surgically excised.
 This is a verruca vulgaris of the anterior maxillary gingiva in a healthy young male. He had recently resolved a wart on his finger.
This is a verruca vulgaris of the anterior maxillary gingiva in a healthy young male. He had recently resolved a wart on his finger.
 Papillomas, which are of questionable viral origin, are frequent findings in the oral cavity, especially on the lateral/ventral tongue and soft palate.
Papillomas, which are of questionable viral origin, are frequent findings in the oral cavity, especially on the lateral/ventral tongue and soft palate.
 These small papillomas on the lateral tongue of a young woman showed histologic evidence of HPV in the form of extensive koilocytosis.
These small papillomas on the lateral tongue of a young woman showed histologic evidence of HPV in the form of extensive koilocytosis.
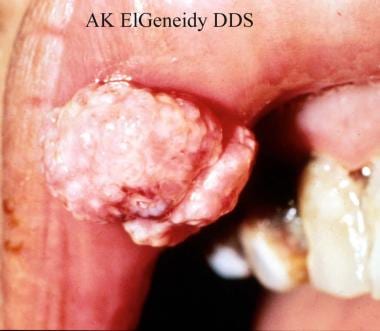 Human papillomavirus (HPV). Condyloma acuminatum of the oral cavity usually appears as a pinker, more cerebriform lesion (as shown here) compared with the whiter, more verrucous appearance of verruca vulgaris. Courtesy of A.K. ElGeneidy, DDS.
Human papillomavirus (HPV). Condyloma acuminatum of the oral cavity usually appears as a pinker, more cerebriform lesion (as shown here) compared with the whiter, more verrucous appearance of verruca vulgaris. Courtesy of A.K. ElGeneidy, DDS.
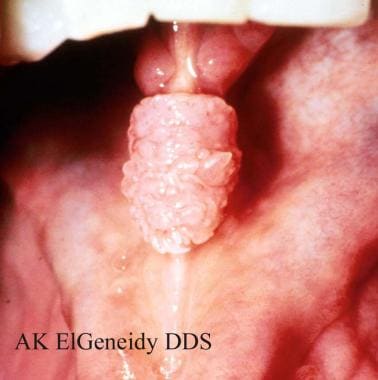 Human papillomavirus (HPV). Some patients with condyloma acuminatum present with multiple oral lesions. Lesion on the lingual frenum occurred in the same man shown in Image 14. Courtesy of A.K. ElGeneidy, DDS.
Human papillomavirus (HPV). Some patients with condyloma acuminatum present with multiple oral lesions. Lesion on the lingual frenum occurred in the same man shown in Image 14. Courtesy of A.K. ElGeneidy, DDS.
 Human papillomavirus (HPV). Condylomata on the lower lip, as well as other sites at the initial presentation (same patient as in Images 14-15). This presentation is unusually extensive. Multiple condylomata may be synchronous or metachronous. This patient did not present with genital condylomata; however, the appropriate health care practitioner should examine patients with condyloma to determine the extent of the disease. The source of infection (eg, a partner who is infected) should also be determined and treated. Courtesy of A.K. ElGeneidy, DDS.
Human papillomavirus (HPV). Condylomata on the lower lip, as well as other sites at the initial presentation (same patient as in Images 14-15). This presentation is unusually extensive. Multiple condylomata may be synchronous or metachronous. This patient did not present with genital condylomata; however, the appropriate health care practitioner should examine patients with condyloma to determine the extent of the disease. The source of infection (eg, a partner who is infected) should also be determined and treated. Courtesy of A.K. ElGeneidy, DDS.
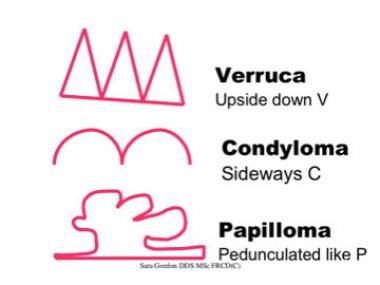 A mnemonic for remembering the microscopic and clinical shapes of verruciform oral lesions: Verruca vulgaris is shaped like a series of inverted V's. Condyloma acuminata are shaped like a series of C's placed on their sides. Papillomas are pedunculated like the letter P.
A mnemonic for remembering the microscopic and clinical shapes of verruciform oral lesions: Verruca vulgaris is shaped like a series of inverted V's. Condyloma acuminata are shaped like a series of C's placed on their sides. Papillomas are pedunculated like the letter P.
 Human papillomavirus (HPV). Heck disease in the buccal mucosa of a 7-year-old boy. Courtesy of Sheldon Mintz, DDS.
Human papillomavirus (HPV). Heck disease in the buccal mucosa of a 7-year-old boy. Courtesy of Sheldon Mintz, DDS.
Differential diagnoses
See the list below:
-
Verruca vulgaris and condyloma acuminata
-
Papilloma
-
Focal epithelial hyperplasia
-
Proliferative verrucous leukoplakia
-
Focal epithelial hyperplasia
-
Focal fibrous hyperplasia (fibroma)
-
Condyloma acuminata
-
Papillomatosis
-
Condyloma plana
-
Verruca plana
-
Connective-tissue tumor
-
Salivary gland tumor
Laboratory studies
The typing of HPV, if deemed necessary, may be performed by immunohistochemical detection of HPV structural proteins. This analysis has a low sensitivity. Enzyme-linked immunosorbent assay and polymerase chain reaction DNA amplification are more sensitive techniques for HPV detection.
Procedures
Diagnosis is usually based on clinical findings, which may be combined with biopsy results. Excisional biopsy is commonly performed, and it has a high success rate as a treatment of these lesions. [83]
Carbon dioxide laser treatment is problematic because viral DNA has been detected in the laser plume. [84] Such laser treatment is considered potentially infectious to surgical personnel. However, HPV DNA was absent in the laser plume of the Er:YAG laser in one study. [85]
Histologic findings
When the production of viral DNA and structural proteins begins, koilocytosis also develops, with dark shrunken nuclei and cytoplasmic vacuolization of infected cells.
Verruca vulgaris typically exhibits a verrucous epithelial proliferation with hyperkeratosis. Koilocytes are frequently noted in the upper stratum spinosum and stratum corneum.
Condyloma acuminata may exhibit acanthosis, vacuolated keratinocytes, a more compact stratum corneum, and parakeratosis.
Focal epithelial hyperplasia (Heck disease) exhibits acanthosis of the spinous layer and thickened, fused rete pegs. The epithelial cells may exhibit intracellular edema. Mitosoid bodies are often noted in the middle to upper levels of the epithelium; these virally-affected cells have a hyperchromatic, shrunken nucleus and bear some resemblance to a cell in mitosis. Slight parakeratosis is usually present.
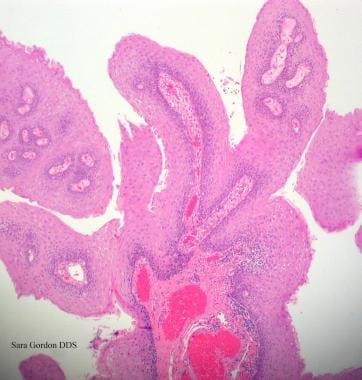 Human papillomavirus (HPV). Verrucae and papillomas appear as frondlike epithelial proliferations. Verrucae tend to be more keratinized with sharper projections than papillomas.
Human papillomavirus (HPV). Verrucae and papillomas appear as frondlike epithelial proliferations. Verrucae tend to be more keratinized with sharper projections than papillomas.
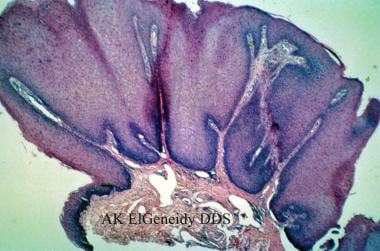 Human papillomavirus (HPV). Condyloma acuminatum generally has a papillary architecture and may microscopically resemble verruca vulgaris and papilloma (hematoxylin and eosin stain, original magnification X10). Courtesy of AK ElGeneidy, DDS.
Human papillomavirus (HPV). Condyloma acuminatum generally has a papillary architecture and may microscopically resemble verruca vulgaris and papilloma (hematoxylin and eosin stain, original magnification X10). Courtesy of AK ElGeneidy, DDS.
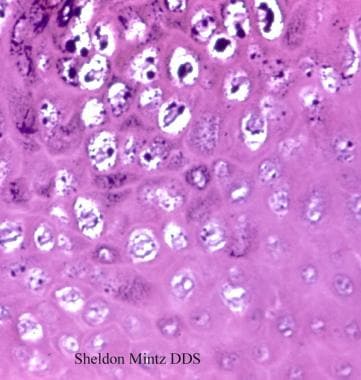 Human papillomavirus (HPV). Koilocytes in the upper epithelium are a helpful, although not completely reliable, indication that a lesion is associated with human papillomavirus. Koilocytes display a dark small nucleus with clear cytoplasm (hematoxylin and eosin stain, original magnification X100). Courtesy of Sheldon Mintz, DDS.
Human papillomavirus (HPV). Koilocytes in the upper epithelium are a helpful, although not completely reliable, indication that a lesion is associated with human papillomavirus. Koilocytes display a dark small nucleus with clear cytoplasm (hematoxylin and eosin stain, original magnification X100). Courtesy of Sheldon Mintz, DDS.
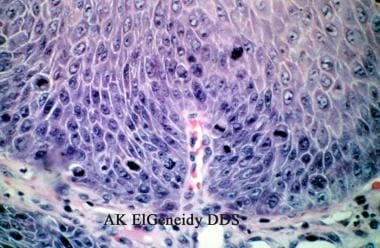 Human papillomavirus (HPV). Condyloma acuminatum may show brisk mitotic activity, although oral condyloma acuminatum is not considered a premalignant lesion (hematoxylin and eosin stain, original magnification X40). Courtesy of A.K. ElGeneidy, DDS.
Human papillomavirus (HPV). Condyloma acuminatum may show brisk mitotic activity, although oral condyloma acuminatum is not considered a premalignant lesion (hematoxylin and eosin stain, original magnification X40). Courtesy of A.K. ElGeneidy, DDS.
Medical Care
Oral lesions are usually treated with excisional biopsy. After the lesions have been removed and the diagnosis is confirmed by biopsy results, they usually do not recur unless reinfection occurs. To prevent reinfection, the source of infection (eg, digits, lesions on sexual partners) should be determined and treated if possible. In HIV-infected patients, recurrence of the lesions is widely reported. The treatment objective can sometimes be limited to control rather than eradication of the HPV lesions. Reports have indicated that solid organ transplant recipients can also be at risk for recurrent and florid oral lesions, which also can limit the treatment objective to control rather than cure.
Topical agents are sometimes used. [86] Cidofovir is an antiviral agent that is a nucleotide analog of deoxycytidine monophosphate. Cidofovir is approved for intravenous administration in patients with AIDS who have CMV retinitis. Topical administration of this medication (1% cream or gel) has been used for refractory condyloma acuminata and recurrent genital herpes. Cidofovir is occasionally used for oral lesions. When used systemically, it may cause nephrotoxicity, uveitis, and numerous other adverse effects. [87, 88]
Intralesional injections may be used in refractory cases, but they are not recommended for the primary treatment of oral lesions. Bleomycin is a cytotoxic polypeptide that inhibits DNA synthesis in cells and viruses. Adverse effects include pain with injection, local urticaria, Raynaud phenomenon, and possible tissue necrosis. Bleomycin should be considered a third-line treatment when standard therapies have failed. IFN-A is a naturally occurring cytokine with antiviral, antibacterial, anticancer, and immunomodulatory effects. Intralesional administration of IFN-A is associated with mild flulike symptoms. Treatments may be required for several weeks to months before beneficial results are observed. IFN-A should be considered a third-line treatment to be used after standard therapies have failed. Research on topical low-dose IFN-A is being conducted. The results of this therapy have yet to be communicated.
Systemic agents, such as retinoids or synthetic vitamin A analogs, may be used to treat extensive lesions in patients who are immunocompromised or immunosuppressed. They may be used in conjunction with other treatments. Adverse effects may include liver function abnormalities, increased serum lipid levels, and teratogenicity. Some clinicians have used podophyllin, but it is not approved by the FDA for this purpose.
Imiquimod 5%(Aldara), a toll-like receptor 7 activator, has been approved for external genital warts and has been tried with varied success in the oral cavity.
Vaccination
As of February 2015, the CDC recommends the use of the nanovalent vaccine to be administered to all adolescents aged 11-12 years and through age 18 years, with the possibility of starting the vaccine series at age 9 years. When the vaccine is administered before age 15 years, the CDC recommends two doses be administered 6-12 months apart. At age 15 years, the CDC continues to recommend three doses, with the second dose administered 1-2 months after the first and the third dose administered at 6 months. [89] Special situations such as pregnancy, immune compromised status, or history of sexual assault result in a modification of the above recommendations.
Early data on the efficacy of the HPV vaccine indicate that HPV vaccination provides a sustained immunogenicity, which 5 years after vaccination results in HPV-6– and HPV-18–specific antibodies that remain 35-fold above that seen following a natural infection. [90]
Early data demonstrate that HPV vaccination results in HPV-specific antibodies in the oral cavity. [91] The efficacy of HPV vaccination to reduce oral HPV infection rates, and ultimately HPV-associated oropharyngeal cancer, is expected to be documented over time.
Medication
See Medication.
Further outpatient care
Monitor the patient for the recurrence of the condition.
Consult a dermatologist for patients with skin lesions.
Consult an obstetrician/gynecologist (for females) or a urologist (for males) for patients with condyloma acuminata (and their sexual partners) to detect, diagnose, and treat any coexistent lesions of the anogenital lesion, which may be premalignant.
If the initial therapy is inadequate or lesions recur, evaluation of the patient for underlying immunosuppression may be warranted.
Complications
Local scarring from surgical excision may occur.
Transmission to family members or sexual partners is possible.
Recurrence may be observed.
Prognosis
The prognosis is excellent. In extreme conditions, the treatment objective is limited to control rather than eradication of the HPV lesions.
Education
Educate the patient concerning the etiology and the route of transmission to prevent reinfection. This should include education regarding safer genital, anal, and oral sex.
Given the association between sexual behavior and the rate of HPV infection as measured by HPV detection in oral rinses (discussed above), oral HPV has to be considered as a sexual transmitted virus and requires counseling of patients by healthcare providers. This counseling must include informing the patients of the up-to-date knowledge on the mode of transmission of oropharyngeal HPV and the possible risks associated with it.
This issue is pertinent to deciding on HPV vaccination especially for male patients. Finally, for this reason, younger adolescents and their parents, should be included in this counseling. The oral and maxillofacial pathology section of the American Dental Education Association decided at a 2009 consensus meeting that when a dentist and patient discuss the patient’s history, this should include a discussion of possible exposure to high-risk HPV types, and safer sex practices, for all patients judged to be sexually active. This is a new direction for dentists, who have not traditionally discussed sexual matters with their patients.
Medical/legal Pitfalls
Note the following medicolegal pitfalls:
-
Failure to refer patients for evaluations of potentially malignant anogenital lesions
-
Failure to diagnose or misdiagnosis of a verrucous carcinoma
-
Failure to inform patients about the rare risk of oral malignancy if inadequately diagnosed and treated
-
Failure to indicate the need for follow-up, even after treatment
-
Failure to warn patients of the risk of recurrence or of treatment failure
-
Failure to indicate treatment availability
-
Failure to inform patients of the risk of transmission of HPV
-
Failure to inform patients with condyloma of the need to treat sexual partners
-
Failure to search for immunosuppression in patients with treatment failures and lesion recurrences
Coxsackievirus
Background
The coxsackieviruses belong to the Picornaviridae family, more specifically, the Enterovirus genus. Enteroviruses are further divided into 4 subgroups: polioviruses, group A coxsackieviruses, group B coxsackieviruses, and echoviruses. Group A coxsackieviruses comprise 23 serotypes, and group B coxsackieviruses comprise 6 serotypes.
Coxsackieviruses cause 3 conditions that can manifest in the oral cavity: hand-foot-and-mouth disease, herpangina, and acute lymphonodular pharyngitis. Hand-foot-and-mouth disease is usually caused by coxsackievirus A16 and, less commonly, by types A5, A7, A10, B2, and B5 and Enterovirus 71 (EV-71). EV-71 outbreaks are often associated with more serious manifestations, including meningitis. Herpangina outbreaks and individual cases are mainly associated with coxsackieviruses A1-6, A8, A10, and A22. Acute lymphonodular pharyngitis is associated with the A10 subgroup.
Pathophysiology
Enteroviruses infect humans mainly via the fecal-oral route. Spread of the disease can also occur via direct contact with nasal and throat secretions from individuals who are infected.
The virus attaches and replicates in susceptible areas of the pharynx or in the distal part of the GI tract. After multiplying in the submucosal lymphoid tissues, enteroviruses move to the regional lymph nodes (cervical and mesenteric) and produce a minor viremia that is transient and undetectable. Most infections are subclinical, and viral replication stops or is halted by host defense mechanisms. Oral and cutaneous lesions result from secondary infection of the small blood vessels during viremia. The incubation period is 2 days to 2 weeks but is generally 3-5 days. A patient who is infected sheds the virus several days before symptoms appear and can continue to excrete the virus several weeks after the illness.
Frequency for hand-foot-and-mouth disease
In the United States, most cases (individual and outbreaks) occur in the summer and early fall.
Internationally, major outbreaks of hand-foot-and-mouth disease related to Enterovirus 71 (EV-71) occurred in Malaysia in 1997, [92] with periodic epidemics since then, [93] and in Taiwan in 1998. Over 75,000 cases were reported in Quingdao, People's Republic of China between 2007 and 2014, with peak incidence in the warmer months. [94] In 2008, 387 severe cases of hand-foot-and-mouth disease and 14 deaths were reported in Taiwan. [95] In Vietnam between 2011 and 2012, there were over 200,000 hospitalizations and 207 deaths from hand-foot-and-mouth-disease. [96] Between 2008 and 2014, 10,717,283 cases of hand-foot-and-mouth-disease were reported in China. There were 3,046 deaths with a fatality rate of 0.03%. [97]
Hand-foot-and-mouth disease is not a reportable disease in the United States. The most recent reports of US hand-foot-and-mouth disease occurred during the period of November 7, 2011 to February 29, 2012. During this time, 63 cases were reported to CDC. Regionally, these cases were concentrated in Alabama, California, Connecticut, and Nevada. Of the 63 cases, a significant percentage of patients (63%) were younger than 2 years and 24% of cases were in adults older than 18 years. Coxsackievirus A6 was seen in 74% of the cases in which clinical specimens were obtained. International importation of these cases was not felt to be a contributing factor based on travel history. [98]
Frequency for herpangina and acute lymphonodular pharyngitis
In the United States, illness usually occurs as summer outbreaks, peaking between August and October. Infections occur with higher frequency in younger age groups, in people who live in crowded areas, and in people who are economically disadvantaged. Under these conditions, the rate of infection with 1 or more enteroviruses can be more than 50%.
There was a significant outbreak of herpangina in Hangzhou, China during the summer of 2015. Between May and August 2015, 210 cases of herpangina were diagnosed among children, with 91% occurring in children younger than age 5 years. [99]
Mortality/morbidity
Oral symptoms, such as mild pharyngitis and erythema of the oral mucosa, occur with hand-foot-and-mouth disease, herpangina, and acute lymphonodular pharyngitis. In hand-foot-and-mouth disease, an accompanying rash also occurs. Other than the oral discomfort and general malaise that accompany herpangina, acute lymphonodular disease, and most forms of hand-foot-and-mouth disease, mortality and morbidity rates are low.
Hand-foot-and-mouth disease caused by EV-71 is often accompanied by more life-threatening manifestations, such as respiratory distress and aseptic meningitis. A major outbreak of hand-foot-and-mouth disease was reported in Taiwan in 1998; this outbreak resulted in a number of deaths. The etiologic agent implicated was EV-71. Most patients who were hospitalized developed rapid cardiopulmonary failure and died soon afterward. This event is the third known EV-71 outbreak leading to rapid deterioration and death in children. Previous outbreaks in young children occurred in Bulgaria in 1975 and in Malaysia from April through June in 1997. [100]
Race
No racial predilection is reported.
Sex
No sexual predilection is apparent.
Age
Hand-foot-and-mouth disease most often occurs in children younger than 5 years. Herpangina most frequently occurs in children aged 3-10 years. Acute lymphonodular pharyngitis also most frequently occurs in children.
Clinical history for hand-foot-and-mouth disease
After an incubation period of 3-6 days, a mild fever usually occurs, accompanied by malaise, anorexia, and a sore mouth. Oral vesicular lesions usually follow after 1-2 days. Skin lesions follow oral lesions in approximately 75% of children who are infected, whereas only 10% of adults who are infected present with a cutaneous rash. The infection usually lasts 5-8 days. Oral lesions generally occur in groups of 5-10 vesicles that soon rupture and often coalesce, resulting in shallow ulcerations surrounded by erythematous halos. Involved sites include the anterior buccal mucosa, the tongue, and the soft palate.
Accompanying skin lesions occur on the dorsal or lateral aspects of the hands and feet and on the fingers and toes. Skin lesions are approximately 3-7 mm in diameter and consist of a mixture of papules and clear vesicles with a surrounding zone of erythema.
Clinical history for herpangina
In herpangina, the sudden onset of infection is characterized by fever, sore throat, and painful swallowing. These symptoms manifest several hours to a day prior to the appearance of vesicular lesions on the posterior aspect of the pharynx. Other symptoms include headache, anorexia, vomiting, and abdominal pain. The fever usually subsides in 2-4 days, but ulcers may be present for as long as 1 week. Most cases of herpangina are mild and resolve spontaneously.
The oral lesions begin as punctate macules that evolve over a 24-hour period into 2- to 4-mm erythematous papules. Vesicular change and central ulceration follow, with the development of peripheral zones of erythema. The lesions usually occur in groups of 2-6 and are moderately painful. They occur on the soft palate, usually between the tonsils and the uvula. The lesions are less frequently observed on the tonsils, on the posterior aspect of the pharyngeal wall, or on the buccal mucosa.
Clinical history for acute lymphonodular pharyngitis
Acute lymphonodular pharyngitis is considered a variant of herpangina. The pattern of distribution of oral lesions is similar to that observed in herpangina. The main difference is that in acute lymphonodular pharyngitis, the pharyngeal lesions remain papular without progression to vesicles and ulcers.
Differentials for hand-foot-and-mouth disease
See the list below:
-
Herpetiform ulcers
-
Primary and secondary herpetic stomatitis
-
Herpangina
Differentials for herpangina
See the list below:
-
Primary herpetic gingivostomatitis
-
Acute herpetic pharyngotonsillitis
-
Herpetiform stomatitis
-
Gonococcal pharyngitis
-
Bacterial tonsillitis
-
Viral pharyngitis
Differentials for acute lymphonodular pharyngitis
See the list below:
-
Viral pharyngitis
Laboratory studies
The diagnosis for each of the 3 entities can usually be established based on the clinical symptoms. However, if laboratory confirmation is necessary, viral isolation via cell culturing, polymerase chain reaction, or serologic testing can be used. [101] Cell culturing is the most widely used method for confirming the diagnosis.
Genomic sequencing of the virus is likely to be used for confirmation in the future.
Procedures
Swabs can be taken from the oral lesions or from the stool samples submitted for viral testing.
Histologic findings
Initially, intracellular and intercellular edema occurs with formation of an intraepithelial vesicle. This progresses to reticular degeneration, followed by ulceration. A mixed lymphocytic and neutrophilic inflammatory cell infiltrate is often present.
Medical care
Medical care is not usually necessary. The goals of treatment are to make the patient comfortable and to prevent secondary infections or worsening systemic illness. The patient should maintain fluid intake and a balanced diet with the use of liquid food replacement if necessary. Analgesics, such as acetaminophen, may make the patient more comfortable. Aspirin should be avoided in pediatric patients because of the possibility of Reye syndrome. Topical anesthetics and coating agents may make the patient more comfortable and may aid in the consumption of food; however, they do not speed healing.
As of 2017, two EV-71 vaccines that were approved in 2015 and 2016 are commercially available in China. These are formalin-inactivated EV-71 vaccines that protect against EV-71 but not against CVA-16, which causes the most common form of hand-foot-and-mouth- disease. There are calls to develop a bivalent formalin-inactivated EV-71/CVA-16 vaccine or other multivalent vaccines. [102]
Medication
See Medication.
Mumps
Background
Mumps, also known as epidemic parotitis because it often causes marked parotid disease, is an acute generalized infection observed in children aged 5-15 years. The viral agent belongs to the Paramyxoviridae family. The parotid glands are usually affected, whereas the submandibular and sublingual glands are generally spared. Meningitis and epididymo-orchitis are the 2 most important but less common features of this disease. [103]
Pathophysiology
The mumps virus is a member of the Paramyxoviridae family and of the Rubulavirus genus. This genus includes the mumps virus; Newcastle disease virus; and human parainfluenza virus types 2, 4a, and 4b. Transmission of the mumps virus occurs via direct contact, via droplets, or via fomites, and it enters through the nose or mouth. More intimate contact is necessary for the spread of mumps than for measles or varicella. During the incubation period (approximately 16-18 days), the virus proliferates in the upper respiratory tract and regional lymph nodes. Viremia follows with secondary spread to the glandular and neural tissues. Inflammation of infected tissues leads to the manifestations of parotitis and aseptic meningitis. Patients are most contagious 1-2 days before the onset of parotitis.
Frequency
In the United States, prior to the use of the live-attenuated mumps vaccine in 1967, epidemics occurred every 2-5 years. The outbreaks were more frequent between January and May. Since the introduction of the mumps vaccine, a decline of more than 99% has occurred in the annual incidence of mumps in the United States. In 1986 and 1987, a resurgence of mumps occurred, with 12,848 cases reported in 1987. Most cases affected children aged 10-19 years who were born prior to the institution of recommendations for routine mumps vaccination. [104]
In the United States, a mumps outbreak occurred in 2006. It involved 45 states and the District of Columbia. [105] From January 1 to October 7, 2006, 5783 cases of mumps were reported, of which 3113 (54%) were confirmed, 2612 (45%) were probable, and 58 (1%) were of unknown classification. [106, 107] This was the largest outbreak of mumps since 1991, when 4264 cases were reported. With regard to the 2006 outbreak, the median age was 22 years and 3644 cases (63%) occurred in females. Most of the cases were reported in individuals who had received two doses of measles, mumps, rubella (MMR) vaccine. It is known that two doses of MMR are not totally effective in preventing disease. One other contributing factor is the college campus environment, where close contact of students can spread mumps through respiratory and oral secretions. Another factor is that only 25 states have a college admission requirement of two doses of MMR vaccine.
Another US outbreak of mumps occurred in 2009. This was the most significant outbreak since 2006. The 2009 mumps outbreak occurred in the northeastern United States, specifically in the New Jersey/New York area and started in June 2009. One thousand seven hundred and seventy-six cases occurred by year end. Most cases occurred in the Orthodox Jewish community, a significant number of which (77%) were in males. Furthermore, 36% of cases of mumps were seen in adolescents aged 13-17 years. If the individuals who received vaccination for mumps, 88% received a single dose or more of mumps vaccine while 76% had received 2 doses. [108]
Most recently in 2016, 4,975 cases of mumps were reported in Arkansas. These made up 78% of all cases in the United States during that year. Of the individuals with mumps, 73% were immunized with two doses. [104]
Internationally, mumps is endemic throughout the world.
Mortality/morbidity
Deaths related to mumps are rare; more than half the deaths occur in individuals older than 19 years. Fetal deaths are increased when mumps infection occurs during the first trimester. Approximately one third of the people infected with the mumps virus are asymptomatic. Although as many as 50% of patients with mumps demonstrate inflammation of the CNS, less than 10% present with manifestations of CNS infection. Adults are at higher risk of aseptic meningitis. A common complication of mumps infection is orchitis, but sterility is rare. Other less common complications include pancreatitis and deafness.
Race
No racial predilection is reported.
Sex
Males and females are affected equally.
Age
Mumps is uncommon in infants younger than 1 year because of passive immunity acquired via placental transfer of maternal antibodies. Before the vaccine was instituted in 1967 and during the initial period of vaccination, most cases occurred in children aged 5-9 years, with 90% of cases in children younger than 15 years. In the late 1980s, a shift toward older individuals aged 5-19 years occurred. More recently, the number of cases in infants and elderly persons has increased.
Clinical history
Prodromal symptoms include a low-grade fever, malaise, lack of appetite, and headache. A day after the initial symptoms appear, reports of earache and tenderness of the parotid glands are common. One parotid gland often enlarges a few days after the other, and unilateral involvement is observed in one fourth of patients with salivary gland involvement. Once maximum parotid gland swelling has occurred, the pain, fever, and tenderness quickly diminish. The affected parotid gland returns to its normal size within 1 week. Complications of parotitis are uncommon. Recurrent acute and chronic sialadenitis are potential complications of parotitis. [109]
Physical findings
Parotitis results in enlargement and tenderness of involved parotid glands, and it is observed in 30-40% of individuals who are infected. At its most severe stage, the earlobe on the affected side lifts upward and outward. Enlarged parotid glands can also be observed when viewing the patient from behind. The enlarged parotid gland may obscure the angle of the mandible, in contrast to cervical lymphadenopathy, which does not hide this structure.
 This patient with mumps has marked bilateral swelling of the salivary glands. Courtesy of Sheldon Mintz, DDS.
This patient with mumps has marked bilateral swelling of the salivary glands. Courtesy of Sheldon Mintz, DDS.
Intraorally, enlargement and redness of the opening of the Stensen duct of the affected gland occur. Trismus can lead to difficulty in eating and in speaking. Involvement of the submandibular glands may accompany parotitis but rarely occurs as the sole manifestation of mumps. Submandibular gland involvement is similar in presentation to that of anterior cervical lymphadenopathy. Sublingual gland involvement is least likely to occur in comparison with the other major salivary glands. Submandibular and sublingual gland involvement is usually bilateral and accompanied by swelling of the tongue.
Causes
Epidemics related to the mumps paramyxovirus have occurred in military populations and other communities, including prisons, boarding schools, ships, and remote islands. The spread of mumps in a community is also postulated to occur via children in schools and via those who secondarily infect their family members. In spite of vaccination, past outbreaks of mumps may be related to vaccine failure by using a single dose of the vaccine.
Differentials for bilateral parotid enlargement
See the list below:
-
Infections - Parainfluenza 3 virus, coxsackievirus, influenza A virus, CMV, Staphylococcus aureus (suppurative parotitis), or HIV-related parotitis
-
Drug-related - Phenylbutazone, thiouracil, iodides, or phenothiazines
-
Metabolic
Diet
A soft diet is indicated for patients experiencing trismus.
Avoidance of citric fruit juices is recommended for patients with mumps because they stimulate salivary production, which can induce pain in these patients
Medication
Analgesic antipyretics may be recommended to reduce pain and discomfort from parotitis. Warm or cold packs applied to the face also may be helpful. Cases of meningitis or pancreatitis require appropriate medical attention. See Medication.
Vaccination
The mumps vaccine (Jeryl-Lynn strain) is a live-attenuated vaccine that was licensed in 1967. The mumps vaccine may be administered alone or in combination with the rubella and measles vaccines (MMR vaccine). Over 97% of individuals who are vaccinated develop measurable antibodies to the mumps virus. Immunity from vaccination is estimated to last more than 25 years and is believed to be lifelong in many vaccinated individuals.
Two doses of mumps vaccine are routinely recommended in all children. Doses should be administered at least 1 month apart. The first dose is usually administered on or after the child's first birthday. A second dose is administered to ensure immunity in those who do not respond to the first dose. The second dose may be administered in children aged 4-6 years. Individuals born after 1957 should show documentation of at least 1 dose of the MMR vaccine. If this documentation is not available, a single dose of the MMR vaccine should be administered.
To prevent mumps infections from occurring in individuals vaccinated twice for mumps, it has been suggested that young adults receive a third dose of mumps vaccine. This has not been seen to work effectively. In cases in which a third booster dose was given to young adults, antibodies produced against the mumps virus were increased during the first month after administration of the vaccine. The antibody levels dropped to baseline levels 1 year after immunization. It was concluded that although the mumps vaccine could not prevent outbreaks, it might be beneficial in controlling outbreaks. [104]
Complications
In the CNS, aseptic meningitis is a relatively common complication that does not cause symptoms in 50-60% of patients. Aseptic meningitis manifests with symptoms of headache and stiff neck in approximately 15% of patients. Resolution occurs in 3-10 days.
Orchitis (testicular inflammation) is one of the most common complications of mumps infection. It occurs in approximately 20-50% of postpubertal males, usually after the onset of parotitis. Symptoms include testicular swelling and tenderness, nausea, vomiting, and fever. Pain and swelling diminish after 1 week, but tenderness may continue for several weeks. Testicular atrophy occurs in 50% of patients with orchitis, but sterility is uncommon.
Pancreatitis is an uncommon complication and may manifest in the absence of parotitis. Hyperglycemia is temporary and reversible. Infection with the mumps virus has been suggested to be related to type 1 diabetes mellitus; however, studies have not been conclusive thus far.
Mumps-related deafness is one of the major causes of acquired sensorineural deafness in children. This complication is estimated to occur in 1 in 20,000 patients with mumps.
Prognosis
The prognosis is good.
Education
Children who are infected with mumps should not attend school or daycare centers until 9 days after the onset of parotitis.
When attempting to control outbreaks, schools should exclude susceptible students from attending affected schools. The susceptible students may return to school after immunization. Students who are exempt from mumps vaccination for medical, religious, or other reasons should avoid affected schools for at least 26 days after the onset of parotitis in the last person who was infected.
Measles (Rubeola)
Background
Measles, also known as rubeola, is an acute, infectious, highly contagious disease that frequently occurs in children. In the United States, the incidence of measles has dramatically decreased as a result of the measles vaccine; however, it remains a significant problem in developing countries. [110] It is reemerging as a health problem in North America because of regional pockets where vaccination rates have fallen below 90-95%. It should not be dismissed as a simple nuisance childhood disease, since 1-2 of every 1000 infected patients die of this disease, with higher rates in immunosuppressed patients and those with congenital heart disease. [111]
Pathophysiology
The measles virus is a paramyxovirus belonging to the Morbillivirus genus. The paramyxovirus can survive for as long as 2 hours in the air and on surfaces. Measles is spread by direct contact via droplets from respiratory tract secretions in patients who are infected. It is considered one of the most communicable infectious diseases.
The initial site of infection is the respiratory tract epithelium. Multiplication of the measles virus in the respiratory tract epithelium and regional lymph nodes is followed by a primary viremia, with spread to the reticuloendothelial system. A secondary viremia occurs upon breakdown and necrosis of the reticuloendothelial cells, and the virus infects the leukocytes. During the secondary viremia, infection may spread to the thymus, spleen, lymph nodes, liver, skin, and lungs.
Frequency
An estimated 20 million cases occur globally each year. [112] Prior to the use of the measles vaccine in 1963, approximately 500,000 cases and 500 deaths were reported each year in the United States. Epidemic cycles occurred every 2-3 years. More than 50% of the population had measles by age 6 years, and greater than 90% were reported to have had it by age 15 years. After licensure of the vaccine in 1963, the number of reported cases of measles dropped by more than 98%, and the 2- to 3-year epidemic cycles no longer prevailed.
Between 1989 and 1991, the incidence of measles rose significantly, with approximately 55,000 cases reported in this 3-year period. The highest number of cases occurred in children younger than 5 years. These cases were prevalent in Hispanic and African American populations. This prevalence was determined to be a result of low vaccination rates among preschool-aged children in these groups. The incidence of measles decreased after this period, and since 1993, fewer than 500 cases have been observed in most years. In 2002, a record low measles rate of 0.15 cases per million individuals was reported, representing a 59% decrease from the rate reported in 2000, which was the lowest previously noted. [113]
Persons who are at higher risk for measles are unvaccinated students in colleges and postsecondary institutions because of large concentrations of susceptible people. Others who are at risk of exposure to measles are workers in medical facilities, regardless of whether they are medical or nonmedical staff. People who have refused vaccination for personal or religious reasons are also at high risk. Individuals who are traveling outside the United States are also at increased risk of being exposed to measles. The most likely factor causing measles outbreaks in the United States is when unvaccinated individuals return from travels abroad. Subsequently, transmission of the virus occurs to those who are intentionally unvaccinated, with resulting clusters of outbreaks. [114]
In March 2004, the Iowa Department of Public Health informed the CDC that a 19-year-old student had flown from India to the United States during the infectious stage of measles. Because of a nonmedical exemption, the students at this Iowa college had not been previously vaccinated and 6 of them had become infected with measles during a trip to India. The measles infection in these students while traveling abroad demonstrates how easily measles can be transmitted to unvaccinated individuals. [115]
Since 1993, the largest outbreaks in the United States occurred in groups of individuals who refused vaccination. Between January 1 and July 31, 2008, 131 cases were reported to the CDC, compared with an average of 63 cases per year from 2000 to 2007. Of these cases of measles, 76% were in individuals younger than 20 years and 91% were in those who were not vaccinated or whose immune status was unknown. Additionally, 89% of these cases were associated with importations from other countries. Many of the imported cases were from Europe, where outbreaks were occurring at the time. [116] Since then, these numbers have increased; 667 cases of measles occurred in the United States in 2014. [117]
In 2009, 71 reported cases of measles occurred in the United States. Twenty one cases of measles were deemed imported; 14 of these cases occurred in US residents who had travelled internationally. The remaining 7 cases were in individuals from other countries. Countries of origin of measles included United Kingdom, India, China, Philippines, Vietnam, Italy and Cape Verde. Of the nonimported cases of measles in 2009 that occurred in US residents, 44% of these individuals indicated personal or religious beliefs against vaccination and 22% of individuals were those whose parents had delayed MMR vaccination. [118]
In 2011, 222 cases of measles were reported in the United States. Seventeen outbreaks (3 or more cases linked in time or place) occurred in 2011 in the United States. Fifty percent or 112 cases were associated with outbreaks. Furthermore, 200 cases were reported to be imported with 52 cases occurring in residents of the United States who had travelled internationally. A significant percentage (85%) of individuals with measles were not vaccinated or were not sure as to their past history of vaccination for measles. [119]
When vaccination rates fall in the United States, measles is often the first disease to occur. Ongoing outbreaks appear to be occurring in Europe, where vaccination rates are lower than in the United States. The main countries involved are Austria, Italy, and Switzerland. In 2008, the United Kingdom reported endemic levels of measles cases due to a drop in vaccination levels.
Internationally, measles is endemic or epidemic in many parts of the world.
Mortality/morbidity
Complications have occurred in as many as 30% of patients with measles. The complications are more severe in young children and adults. The most commonly reported complication from 1985-1992 was diarrhea, followed by otitis media and pneumonia.
In the United States, there have been approximately 1-2 deaths per 1000 cases of measles. Young children and adults are at higher risk of death. Pneumonia causes approximately 60% of measles-related deaths, especially in children. In adults, encephalitis-related deaths are more common. Measles-related fatalities are increased in children with leukemia or HIV infection, who are immunocompromised.
Developing countries have higher rates of measles in children younger than 1 year. Malnourishment, particularly vitamin A deficiency, is a factor that influences the severity of measles. The mortality rate due to measles in populations with malnutrition can be as high as 25%. In Africa, measles is the leading cause of blindness in children.
Race
No racial predilection is reported.
Sex
No sexual predilection is apparent.
Age
Prior to the routine administration of the measles vaccine, measles affected school-aged children. After that, other groups were affected, including preschool-aged children younger than 5 years and adults older than 20 years.
Clinical history
The incubation period for measles is the time from exposure to the prodrome. This period is approximately 10-14 days; it is longer in adults than in children.
The prodrome phase lasts for several days and likely coincides with the secondary viremia phase. It is manifested by malaise, fever, anorexia, conjunctivitis, and respiratory symptoms. Toward the end of the prodrome and just prior to the appearance of the rash, Koplik spots are observed. The skin eruption of measles lasts approximately 5-6 days. The period of uncomplicated illness from the late prodrome to disappearance of skin lesions and fever lasts 7-10 days. [120]
Physical findings
The fever in affected individuals can peak as high as 103-105°F. Patients also experience respiratory symptoms, such as cough and coryza (runny nose), which may resemble a severe upper respiratory tract infection.
Koplik spots are pathognomonic for measles. They are located on the buccal mucosa in the premolar and/or molar area. Occasionally, in severe cases of measles, several areas of the oral cavity may be affected by the enanthem. The intraoral lesions may persist for several days and begin to slough with the onset of the rash.
Koplik spots consist of bluish-gray specks against an erythematous background. They have been compared to grains of sand. The number of Koplik spots can range from 1-50 or more. The lesions are plaquelike or nodular and oval or round. The measles rash often begins near the hairline and then involves the face and the neck; over the next few days, it progresses to the extremities and finally to the palms and the soles. The rash is erythematous and maculopapular and may become confluent as it progresses. It lasts approximately 5 days and resolves in the same order it appeared, from the face and the neck to the extremities.
Differentials
See the list below:
-
Koplik spots - Cheek chewing keratotic lesions
-
Large Fordyce granules
Laboratory studies
All specimens collected for viral culture in cases suggestive of measles should be sent to the nearest state public health laboratory or to the CDC. The measles virus can be isolated from blood, urine, or nasopharyngeal secretions. Clinical specimens and serologic specimens should be obtained at the same time and preferably within 7 days of the onset of the rash. The easiest method that aids in confirming the diagnosis is to test for immunoglobulin M (IgM) antibody levels in a single specimen from an individual who is infected. A person who is infected or has received the vaccine initially has an IgM response followed by an immunoglobulin G (IgG) response. IgM antibodies are present for 1-2 months after exposure to the measles virus, and IgG antibodies are present for many years.
IgG tests (eg, enzyme-linked immunoabsorbent assay, hemagglutination inhibition, indirect fluorescent antibody tests) are conducted on 2 specimens. The first specimen is obtained during the acute phase (within 4 days of the start of the rash), and the second specimen is collected during the convalescent phase (2-4 weeks later). Positive results show increased levels of IgG in the convalescent specimen.
Histologic findings
Oral and cutaneous lesions show necrosis of the superficial aspects of the epithelium with an inflammatory infiltrate that consists of neutrophils. Multinucleated giant cells, known as Warthin-Finkeldey cells, may be present in lymphoid tissue and lungs.
Medical care
No specific treatment is necessary for Koplik spots.
Patients should be referred to an appropriate physician for care. Supportive treatment is recommended. Appropriate antibiotic therapy is necessary for secondary bacterial infections.
The World Health Organization has recommended that vitamin A supplementation be provided for children with measles living in areas that have a documented vitamin A deficiency problem.
Intravenous and aerosol administration of ribavirin have been used to treat severe cases of measles in patients who are immunocompromised; however, the FDA has not approved this drug for the treatment of measles.
The measles vaccine currently used in the United States is a live-attenuated Enders-Edmonston strain (formerly called the Moraten strain). This vaccine is combined with the rubella and mumps vaccines and is administered as the MMR vaccine. Antibodies to measles virus develop in approximately 95% of children vaccinated at age 12 months and in 98% of children vaccinated at age 15 months. The vaccine induces long-term, if not lifelong, immunity to measles in 99% of individuals who receive 2 doses. Two doses of the measles vaccine in the form of MMR are recommended for all children. Individuals born before 1957 should be able to show documentation of immunity either via vaccination or via history of disease. In an individual who has been exposed to measles, administration of the live vaccine within 72 hours can provide long-term immunity.
Complications
No oral complications are reported from measles. Diarrhea, otitis media, and pneumonia are the more common complications encountered from measles infection.
One case of acute encephalitis occurs in every 1000-2000 cases of measles. Acute encephalitis begins 6 days after the onset of the rash; symptoms include high-grade fever, headache, stiff neck, convulsions, and coma. The fatality rate is approximately 15%.
Subacute sclerosing panencephalitis is a previously unexplained CNS disease that occurs months to years after the initial measles infection. Progressive deterioration of intellect, convulsive seizures, motor abnormalities, and, eventually, death characterize subacute sclerosing panencephalitis.
When measles infection occurs during pregnancy, the likelihood of early labor, spontaneous abortion, and low birth weight increases. It is questionable whether birth defects are caused by measles infection during pregnancy.
Prognosis
The prognosis is good in well-nourished children.
Rubella
Background
Rubella, also known as German measles, is an acute exanthematous viral infection that is similar in appearance to mild measles (rubeola) infections. It occurs in children and adults. The major potentially serious manifestations are observed in fetuses infected with rubella, resulting in various congenital defects. [121]
Pathophysiology
The rubella virus is an RNA virus belonging to the Togavirus family and the Rubivirus genus. It is related to the group A arboviruses, specifically Eastern and Western encephalitis viruses. The rubella virus is unstable and is killed by lipid solvents, trypsin, formalin, ultraviolet light, and extremes in temperature and pH. The virus is spread via respiratory tract droplets from individuals who are infected. The virus replicates in the nasopharyngeal tissues and lymph nodes. A viremia results 5-7 days after initial exposure to other areas of the body. Patients are believed to be contagious when the rash is emerging. The virus may also be shed from the throat from 10 days before to 15 days after the onset of the rash. In congenital rubella infections, transplacental spread of virus occurs during viremia.
Rubella is moderately contagious. It is most transmissible when the rash begins. Infants with congenital rubella syndrome (CRS) shed large amounts of the virus in their body secretions for many months, and can spread rubella to caregivers vulnerable to rubella infection.
Outbreaks continue to occur in populations that are susceptible to rubella infections, including those exposed to certain individuals who have religious or philosophic beliefs regarding personal exemption to vaccination. Other outbreaks have occurred in workplaces with employees who were born in countries outside of the United States that do not advocate routine immunizations, including Latin American and Caribbean countries. [122]
Frequency
In the United States, the incidence of rubella infections was historically higher in late winter and spring. Prior to the licensure of the rubella vaccine in 1969, the number of cases of rubella was high and epidemics of rubella occurred every 6-9 years. The largest annual number of cases of rubella in the United States was 57,686 cases in 1969. After 1969, the incidence of rubella dropped significantly. Fewer than 1000 cases per year were reported after 1983. In 1988, the number of cases of rubella in the United States fell to an all time low of 223. However, in 1989, the number of cases nearly doubled from the previous year to 396. This was thought to have occurred together with the rise in measles cases, because of failure to perform timely vaccination of preschool children. After this resurgence, the number of cases of rubella fell steadily.
The demographics of rubella cases in the United States has changed since the 1990s. It now occurs more frequently in foreign-born Hispanic adults who are unvaccinated or in those who have unknown vaccination status. Furthermore, rubella infection continues to occur in women of childbearing age who were born outside the United States. [123]
Since 2001, the annual numbers of rubella cases in the United States have been the lowest in recorded history. Twenty-three cases were reported in 2001, 18 in 2002, 7 in 2003, and 9 in 2004. Approximately half of these cases occurred in persons born outside the United States, of whom most were born outside the Western Hemisphere.
In 2005, the United States declared that it had eliminated endemic rubella transmission. [124, 125] Between 2005 and 2007, 34 cases of rubella had been reported in the United States. A median of 25% (range 18-45%) of cases were imported between 2005 and 2007. The countries of origin included Brazil, France, Russia, Uganda, Philippines, Malaysia and Bangladesh. [126]
While rubella is endemic in many other parts of the world, the United States continues to maintain high vaccination rates in children, encourages vaccination in women of childbearing age (especially in those born outside the United States), and continues surveillance and response to future outbreaks of rubella. [127]
Internationally, rubella infections occur worldwide.
Mortality/morbidity
Complications of rubella infection occur more frequently in adults than in children.
Arthritis and/or arthralgias occur in as many as 70% of adult women who are infected with rubella. Joint involvement occurs at the same time as the rash and may last as long as 1 month.
Encephalitis is observed in 1 in 5000 cases and more often in adults than in children. Deaths rates related to encephalitis in the setting of rubella range from 0-50%.
Hemorrhagic complications occur in approximately 1 in 3000 cases and manifest more often in children than in adults. Thrombocytopenic purpura is common and likely due to low levels of platelets and vascular damage. GI and cerebral hemorrhage may also occur.
In 1964, 12.5 million cases of rubella were reported, with 20,000 infants born with CRS. In early pregnancy, rubella infection can lead to serious complications, including fetal death, premature delivery, and congenital defects. Spontaneous abortions and stillbirths are common. As many as 85% of fetuses infected during the first trimester are affected. Complications are rare when rubella infection occurs after the 20th week of pregnancy.
All organ systems may be affected in CRS. Some investigators have reported developmental defects, including enamel hypoplasia and delayed eruption of deciduous teeth; however, other groups have debated the validity of such findings in CRS. Deafness is the most common manifestation and, occasionally, the only one of congenital rubella infection. Ocular defects, such as glaucoma, cataracts, and retinopathy, are possible sequelae. Cardiac defects, including patent ductus arteriosus, ventricular septal defect, pulmonary stenosis, and coarctation of the aorta, may be observed. Neurologic manifestations, such as microcephaly and intellectual disability, are other potential complications.
Race
No racial predilection is reported.
Sex
No sexual predilection is apparent.
Age
Rubella is considered a childhood disease; however, it can affect adolescents and adults.
Clinical history
The incubation period is approximately 12-23 days. A prodrome is observed more often in older children and adults than in others; it lasts 1-5 days. Symptoms include low-grade fever, swollen lymph nodes, malaise, and upper respiratory tract symptoms. The rash of rubella follows the prodrome and lasts approximately 3 days. Lymphadenopathy can be observed as long as 1 week before the onset of the rash and up to several weeks later. [128]
Physical findings
Symptoms are often mild, and 30-50% of patients are asymptomatic or subclinical. The major manifestation of rubella is the presence of lymphadenopathy involving the postauricular, posterior cervical, and suboccipital lymph nodes. The rash of rubella begins on the face and progresses down the body. The rash consists of erythematous macules and, at times, small papules.
Intraorally, an enanthem consisting of petechial lesions, known as the Forchheimer sign, is observed in approximately 20% of patients. Clinically, these dark-red papules are observed on the soft palate. These lesions may arise at the onset of the rash. Palatal petechiae are also occasionally observed. The Forchheimer sign is not pathognomonic of rubella infection.
Other manifestations of rubella infection include conjunctivitis, orchitis, and arthritis.
Differentials for the Forchheimer sign
See the list below:
-
Trauma
-
Chronic cough
-
Infectious mononucleosis
-
Thrombocytopenia
-
Trauma from fellatio
-
Hemophilia
-
Leukemic thrombocytopenia
-
Hereditary hemorrhagic telangiectasia
-
Nonthrombocytopenic purpura
Laboratory studies
The rubella virus can be isolated from various secretions, including nasal, throat, blood, urine, and cerebrospinal fluid (CSF) specimens. The virus should be isolated in all cases suggestive of rubella or CRS. Serologic analysis is the most common means of confirming the diagnosis of rubella exposure.
Enzyme-linked immunoabsorbent assay is a readily available and easily performed test. It is used to detect IgM antibodies early in infection or IgG antibodies during the postinfection and/or vaccination period. Positive IgM test results for rubella imply recent postnatal infection or congenital infection. False-positive results for rubella IgM have been documented in patients with positive rheumatoid factor, parvovirus infections, and positive heterophile testing for infectious mononucleosis.
Histologic findings
No intraoral histologic findings are specific to rubella.
Medical care
Treatment for rubella is supportive care. Patients should be referred to an appropriate physician for care. Individuals with rubella infection should be isolated from places, such as school and work, for 7 days after the onset of the rash. No specific treatment is indicated for the oral manifestations of rubella.
The currently used rubella vaccine is a live-attenuated virus. The rubella vaccine can be administered as a single agent or in combination with the measles and mumps vaccines as the MMR vaccine. Of individuals who are vaccinated, 90% or more are protected against clinical rubella for at least 15 years. A single dose of the vaccine likely provides long-term immunity. Immunizing postpubertal males and females is recommended. The goal of rubella vaccination is to prevent CRS.
Prognosis
The prognosis is good in postnatal rubella.
The prognosis is guarded in CRS, depending on the severity of the manifestations.
Medications
Local anesthetics
Local anesthetics stabilize the neuronal membrane and prevent the initiation and transmission of nerve impulses. Agents used include dyclonine and lidocaine.
Dyclonine (Dyclone) details are as follows:
-
Description - Oral local anesthetic that blocks impulses at peripheral nerve endings in skin and mucous membranes by changing permeability of cell membrane to certain ions. Used for temporary relief of pain associated with oral mucosa.
-
Adult dose - 5-10 mL of 0.5% or 1% solution applied to oral mucosa (swab or swish and expectorate) tid/qid prn; not to exceed 200 mg or 40 mL of 0.5% solution or 20 mL of 1% solution
-
Pediatric dose – For < 2 years, adjust dose according to weight and age; for >2 years, 1 children's strength (1.2 mg) lozenge, dissolved slowly in mouth q2h prn
-
Contraindications – Documented hypersensitivity
-
Interactions – None reported
-
Precautions - Hypotension; bradycardia; cardiac arrest; excitation; drowsiness; nervousness; dizziness; seizures; blurred vision; respiratory arrest; allergic reactions; slight stinging or irritation may occur upon application; reduce dose in children and patients who are debilitated, elderly, or acutely ill; patients who use topical anesthetics may experience impaired swallowing and increased risk of aspiration (avoid consumption of food for 60 min after oral application); numbness of tongue or buccal mucosa may increase risk of biting trauma
-
Pregnancy - -Category C; fetal risk revealed in studies in animals but not established or not studied in humans; may use if benefits outweigh risk to fetus
Lidocaine (Xylocaine) details are as follows:
-
Description - Topical anesthetic for mucous membranes of mouth and pharynx that binds selectively to sodium channels, thus blocking entry of sodium ions into axon. Depolarization and progression of action potential is prevented.
-
Adult dose - 1 tbsp (15 mL) or less undiluted solution, swish in mouth then expectorate; alternatively, apply up to 1 tbsp of solution to affected area with a cotton-tipped applicator; do not repeat more frequently than q3h; not to exceed 8 doses/d
-
Pediatric dose – For < 3 years, not established; for >3 years with lean body mass and normal body development, maximum dosage is calculated according to weight or age; based on weight, 1.5-2 mg/lb is recommended
-
Contraindications – Documented hypersensitivity
-
Interactions - Potential for increased toxicity with class I antiarrhythmic drugs (eg, tocainamide, mexiletine); effects are additive
-
Precautions - Reduce dose in children and patients who are debilitated, elderly, or acutely ill based on age, weight, and physical condition; patients who use topical anesthetics may experience impaired swallowing and increased risk of aspiration (avoid consumption of food for 60 min after oral application); numbness of tongue or buccal mucosa may increase risk of biting trauma
-
Pregnancy - Category B; fetal risk not confirmed in studies in humans but has been shown in some studies in animals
Analgesics
These agents ensure patient comfort, promote pulmonary hygiene, and have sedating properties. Agents used include acetaminophen.
Acetaminophen (Tylenol) details are as follows:
-
Description – Used to treat pain and fever. Has no anti-inflammatory effects. Inhibits synthesis of prostaglandins in CNS and peripherally blocks pain impulse generation. Causes antipyresis by inhibiting hypothalamic heat-regulating center.
-
Adult dose – 325-650 mg (1-2 tab) q4-6h or 1000 mg tid/qid; not to exceed 4 g/d (4000 mg)
-
Pediatric dose – For < 12 years, 10-15 mg/kg/dose q4-6h prn (not to exceed 2.6 g/d); for >12 years, administer as in adults
-
Contraindications – Documented hypersensitivity; G-6-PD deficiency
-
Interactions – Long-term increased ingestion of alcohol and high doses leads to liver toxicity; cholestyramine decreases plasma levels and may lower response; INH increases blood levels; hepatotoxicity has been reported; barbiturates may increase hepatotoxicity caused by large amounts of acetaminophen; phenytoin can increase the hepatotoxic potential of high doses; warfarin can lead to increased anticoagulation
-
Precautions – May cause hepatic toxicity in extremely high doses; use with caution in patients with alcoholic cirrhosis; liver damage has been observed in patients taking 5-8 g/d over several wk or 3-4 g/d for 1 y
-
Pregnancy – Category B; fetal risk not confirmed in studies in humans but has been shown in some studies in animals
Nonsteroidal anti-inflammatory drugs
These agents have analgesic, anti-inflammatory, and antipyretic activities. Their mechanism of action is not known, but they may inhibit cyclo-oxygenase activity and prostaglandin synthesis. Other mechanisms may also exist, including inhibition of leukotriene synthesis, lysosomal enzyme release, lipoxygenase activity, neutrophil aggregation, and various cell membrane functions. Agents used include ibuprofen.
Ibuprofen (Motrin, Advil) details are as follows:
-
Description – Used in management of dental pain and swelling. For inflammatory conditions, mild to moderate pain, fever, dysmenorrhea, and acute migraine headaches. Inhibits prostaglandin synthesis by blocking action of cyclo-oxygenase.
-
Adult dose – 400-800 mg/dose PO tid/qid; not to exceed 3.2 g/d
-
Pediatric dose – 4-10 mg/kg/dose PO q6-8h
-
Contraindications – Documented hypersensitivity; unsafe if administered during third trimester
-
Interactions – Decreases platelet aggregation, thus increases anticoagulant action of warfarin; may lower prostaglandin-induced renal clearance of lithium, with resultant elevated levels of lithium in plasma and potential lithium toxicity; may raise levels of methotrexate (MTX), with potential development of MTX toxicity; aspirin can lower serum levels; raloxifene (Evista) can interact with other highly protein-bound drugs, including ibuprofen; raloxifene can displace ibuprofen and vice versa, resulting in increased levels of either drug
-
Precautions – Use with caution in patients with CHF, decreased renal or hepatic function, and GI disease; use with caution in patients taking anticoagulants; confusion, agitation, and hallucination possible with high doses
-
Pregnancy – Category B; fetal risk not confirmed in studies in humans but has been shown in some studies in animals
Antihistamines
Antihistamines are type 1 histamine receptor blockers that act to block the action of histamine after its release from mast cells and basophils. They are most effective when used prophylactically. The 2 classes of antihistamines are sedating and nonsedating. Typically, the sedating antihistamines are stronger and have more adverse anticholinergic effects. Agents used include diphenhydramine.
Diphenhydramine (Benadryl, Benylin) details are as follows:
-
Description – Competes with histamine for H1 receptors on effector cells of the GI tract, blood vessels, and respiratory tract, thereby leading to symptomatic relief of allergic symptoms caused by the action of histamine. Can induce local anesthetic effects through infiltration of mucous membranes.
-
Adult dose – 12.5 mg with 5 mL elix, swish with 1 tbsp (15 mL) of solution for 1-2 min and expectorate; may repeat several times per day prn; a 50/50 mixture of the 12.5 mg/5 mL solution mixed with kaolin susp, sucralfate susp, Kaopectate, or Maalox can also be used; swish 1 tbsp (15 mL) in mouth and expectorate; repeat up to 4 times/d
-
Pediatric dose – A maximum of 5 mg/kg/d; swish with 1 tbsp (15 mL) of solution for 1-2 min and expectorate; may repeat several times per day prn
-
Contraindications – Documented hypersensitivity; do not use during acute asthma attacks
-
Interactions – Do not administer with CNS depressants because diphenhydramine may worsen CNS and/or respiratory depression; may interact with MAOIs and lead to increased anticholinergic effects; do not administer elix to patients taking drugs that can cause disulfiram reactions (eg, metronidazole, chlorpropamide) because of high alcohol content
-
Precautions – Use with caution in patients with narrow-angle glaucoma, peptic ulcers, urinary tract obstruction, and hyperthyroidism; elix has high sedative and anticholinergic effects and may not be appropriate for prolonged use in elderly patients
-
Pregnancy – Category C; fetal risk revealed in studies in animals but not established or not studied in humans; may use if benefits outweigh risk to fetus
Antivirals
Nucleoside analogs are initially phosphorylated by viral thymidine kinase to eventually form a nucleoside triphosphate. Acyclovir triphosphate interferes with HSV DNA polymerase and inhibits viral DNA replication. The triphosphate can be incorporated into growing chains of DNA by viral DNA polymerase, resulting in termination of the DNA chain. Acyclovir is preferentially taken up and selectively converted to the active triphosphate form by HSV-infected cells. It is much less toxic to normal uninfected cells. In herpes zoster, acyclovir may decrease the prevalence of postherpetic neuralgia. These agents may also relieve and decrease the duration of symptoms. [129, 130, 131, 132, 133]
Agents used include acyclovir; acyclovir, topical 5%; valacyclovir; famciclovir; and penciclovir.
Acyclovir, oral (Zovirax) details are as follows:
-
Description – Cap, oral susp, and tab dosages are bioequivalent. In patients who are otherwise healthy and immunocompetent, use for moderate-to-severe primary or recurrent HSV (HHV-1, HHV-2) infections, moderate-to-severe chickenpox, or acute herpes zoster. In patients who are immunocompromised, use for primary or recurrent mucocutaneous HSV (HHV-1, HHV-2) infections, chickenpox, herpes zoster, oral hairy leukoplakia, or CMV oral ulcerations. Poorly absorbed from GI tract, 10-20% bioavailability. Oral absorption not significantly affected by food. Widely distributed into tissues and body fluids. Subject to renal elimination by both glomerular filtration and tubular secretion. Half-life in adults with normal renal function is 2.5-3.3 h. Renal function impairment significantly increases half-life.
-
Adult dose for primary HSV – 200 mg q4h PO 5 times/d for 10 d; alternatively, 500 mg tid PO for 7-10 d (In patients who are immunocompromised, duration of treatment may need to be prolonged until lesions have reepithelialized; alternatively, increase oral dose to 400 mg q4h PO 5 times/d for 10 d)
-
Adult dose for recurrent HSV (intermittent therapy; < 6 episodes/y) - 200 mg q4h PO 5 times/d for 5 d
-
Adult dose for recurrent HSV (long-term suppressive therapy; ≥6 episodes/y) - 400 mg bid PO or 200 mg PO 3-5 times/d for up to 12 mo
-
Adult dose for prophylaxis against recurrent HSV - 400 mg q12h PO
-
Adult dose for herpes zoster: 800 mg 5 times/d PO for 7-10 d; for severe infection, 5 mg (base) per kg body weight q8h IV for 5-7 d (administer at constant rate over at least 1 h); patients with acute or chronic renal impairment may require dose reduction (200 mg q12h PO when CrCl 0-10 mL/min or 0-0.17 mL/s
-
Pediatric dose – For < 2 years, data limited; for >2 years, data limited but 3000 mg/m2/d or 80 mg/kg suggested (no unusual toxicity or pediatric-specific problems); half-life of IV form in children >1 y similar to that in adults with normal renal function
-
Contraindications – Documented hypersensitivity to acyclovir, ganciclovir, or valacyclovir; caution in renal function impairment or dehydration because risk of adverse effects is increased; caution in elderly patients with neurologic abnormalities
-
Interactions – Nephrotoxic medications (eg, aminoglycosides, carbamazepine, ciprofloxacin, cisplatin, cyclosporin, lithium, meperidine, intrathecal MTX, metronidazole, parenteral penicillins, tiopronin); concurrent use with oral or parenteral acyclovir may increase potential for nephrotoxicity, especially in the presence of renal function impairment; probenecid may decrease renal tubular of acyclovir, resulting in increased serum and CSF levels, prolonged elimination half-life in serum and CSF, and potentially increased toxicity
-
Adverse effects - Malaise, GI disturbances (nausea, vomiting, diarrhea, abdominal pain), headache, lightheadedness, insomnia, somnolence, paraesthesia, acute renal failure, encephalopathic changes, hematologic abnormalities (anemia, leukocytosis, neutropenia or neutrophilia, thrombocytopenia or thrombocytosis), hematuria, allergy, anaphylaxis, urticaria, DIC, fever, hypotension, leukopenia, lymphadenopathy, peripheral edema, psychological disturbances (confusion, delirium, hallucinations, mental obtundation, psychosis), seizures, skin reactions (erythema multiforme, pruritus, rash, Stevens-Johnson syndrome, toxic epidermal necrolysis), and visual abnormalities; adverse effects may be more pronounced in elderly patients, which is likely due to age-related decrease in renal function; elderly patients may require adjustment of dose or dosing interval
-
Breast milk precautions - Distributed into breast milk in concentrations from 0.5-4 times the corresponding plasma concentration, which would potentially expose a nursing infant to a dose as high as 0.3 mg/kg/d; however, toxicity has not been observed
-
Renal precautions – Half-life increased in patients with renal function impairment; in dialysis, adjust dosage according to patient's CrCl ; a single 6-h period of hemodialysis reduces plasma concentration by approximately 60%; patient may require additional dosage after each dialysis treatment; peritoneal dialysis does not substantially alter clearance
-
Other precautions - May alter BUN and LFT values; in missed dose, take as soon as possible but do not take if almost time for next dose; do not double dose
-
Pregnancy – Category C; fetal risk revealed in studies in animals but not established or not studied in humans; may use if benefits outweigh risk to fetus
Acyclovir, topical 5% (Zovirax) details are as follows:
-
Description – Treatment of initial and recurrent non–life-threatening mucocutaneous HSV infections in nonimmunocompromised patients. Used as adjunctive therapy to improve localized herpes zoster in immunosuppressed patients being treated systemically with other treatment regimens for herpes zoster. Resistance has been reported with prolonged treatment in immunocompromised patients. Resistance does not appear to be significant in immunocompetent patients. Minimal systemic absorption following topical administration. Patients with impaired renal function may have elevated serum levels.
-
Adult dose – Apply to affected area q3-4h, for a total of 6 times/d, for 7 d; apply a sufficient quantity to adequately cover all lesions
-
Pediatric dose – For >2 years, safety and efficacy not established; 3000 mg/m2/d or 80 mg/kg suggested (no unusual toxicity or pediatric-specific problems)
-
Contraindications – Documented hypersensitivity to acyclovir, ganciclovir, or valacyclovir; caution in renal function impairment or dehydration because risk of adverse effects is increased; caution in elderly patients with neurologic abnormalities
-
Interactions – None reported
-
Precautions – Adverse effects may include mild pain with transient burning or stinging (10-30%) and itching (1-10%%); for breastfeeding, small amount absorbed across disease tissues and because total daily topical dose is small, unlikely that significant amount is distributed in breast milk; no geriatric-specific problems reported, but no appropriate studies have not been performed; may lead to skin sensitization, resulting in hypersensitivity reactions with subsequent topical or systemic use; avoid contact with eyes; in missed dose, apply as soon as possible and do not apply if almost time for next dose
-
Pregnancy – Category C; fetal risk revealed in studies in animals but not established or not studied in humans; may use if benefits outweigh risk to fetus
Valacyclovir (Valtrex) details are as follows:
-
Description – Prodrug that is nearly completely converted to acyclovir and L-valine. Phosphorylated by thymidine kinase to acyclovir monophosphate, which is then converted to diaphorase and triphosphate. Acyclovir is selectively converted to active triphosphate form by cells infected with herpes viruses. Used for treatment of acute herpes zoster in patients who are healthy and immunocompetent. Therapy is most effective when started within 48 h after onset of symptoms. Minimizes pain and duration of postherpetic neuralgia more effectively than acyclovir.
-
Absorption properties - Oral form is rapidly absorbed and converted to acyclovir by first-pass intestinal and hepatic metabolism. Food not found to alter bioavailability. Half-life < 30 min. Acyclovir is widely distributed in tissues and body fluids. Acyclovir concentrations in CSF are approximately 50% of plasma concentration. In addition, acyclovir crosses the placenta. Plasma concentration of acyclovir is elevated in patients with impaired renal function, which may require dose change.
-
Adult dose – Primary HSV, 1000 mg bid PO for 7-10 d; recurrent episodes, 500 mg bid PO for 5 d; long-term suppression, 1000 mg/d PO
-
Pediatric dose – Not established
-
Contraindications – Documented hypersensitivity to acyclovir, ganciclovir, or valacyclovir; caution in renal function impairment or dehydration because risk of adverse effects is increased; caution in elderly patients with neurologic abnormalities
-
Interactions – Cimetidine and probenecid decrease rate but not to extent of conversion of valacyclovir to acyclovir; both drugs reduce renal clearance of acyclovir, resulting in increased plasma concentration
-
Adverse effects - Adverse effects may include acute hypersensitivity reactions and anaphylaxis, dysmenorrhea, aplastic anemia, hemolytic anemia, hepatitis with LFT abnormalities, renal insufficiency, thrombocytopenia, facial edema, skin reactions (erythema multiforme, photosensitivity, rash), tachycardia, GI disturbances (nausea, vomiting, diarrhea, abdominal pain, constipation), hypertension, microangiopathic, CNS disturbance (headache, somnolence, agitation, confusion, hallucinations, dizziness), and fatigue
-
Adverse effects in special populations - Increased risk of adverse effects in patients with renal or hepatic disease, advanced HIV infection, bone marrow transplant, or kidney disease; kidney disease may increase blood levels; concurrent administration with potentially nephrotoxic agents may increase risk of renal dysfunction and/or reversible CNS manifestations; patients with a CrCl < 50 mL/min require dose reduction; adverse effects may be more pronounced in older adults, which is more likely due to age-related decrease in renal function; elderly patients may require dose or dose interval adjustment; ensure elderly patients at high risk of dehydration have adequate fluid intake
-
Breast milk precautions - Not known whether distributed into breast milk; major metabolite (acyclovir) is distributed into breast milk at concentrations from 0.5-4 times the corresponding plasma concentration, which would potentially expose nursing infant to a dose as high as 0.3 mg/kg/d; however, toxicity not observed
-
Renal precautions - Half-life of acyclovir is increased in patients with renal function impairment; adjust dosage according to patient's CrCl; a single 4-h period of hemodialysis reduces plasma acyclovir concentration by approximately 33%; half life of acyclovir is approximately 4 h during hemodialysis; patient may require additional dosage after each dialysis treatment; long-term ambulatory peritoneal dialysis and continuous arteriovenous hemofiltration/dialysis do not substantially remove acyclovir
-
Other precautions – For missed dose, take as soon as possible but do not take if almost time for next dose; do not double dose
-
Pregnancy – Category B; fetal risk not confirmed in studies in humans but has been shown in some studies in animals
Famciclovir (Famvir) details are as follows:
-
Description – Prodrug of penciclovir. Penciclovir is further metabolized by viral thymidine kinase to penciclovir triphosphate. Active drug inhibits viral DNA synthesis, thereby inhibiting viral replication. Used for treatment of acute herpes zoster in patients who are healthy and immunocompetent or immunocompromised. Has been found to decrease duration of postherpetic neuralgia compared with placebo (55-62 d vs 128 d). Found to be equivalent to acyclovir in decreasing duration of acute pain. Therapy is most effective when initiated within 48 h of rash onset. Used for recurrent mucocutaneous HSV infections in HIV-infected patients.
-
Absorption properties - Oral form rapidly absorbed in upper intestine and rapidly converted in intestinal wall to active drug, famciclovir. Oral absorption not significantly affected by food.
-
Adult dose for primary HSV - 500 mg q8h PO for 7 d
-
Adult dose for long-term suppression - 250 mg q12h PO for up to 1 y
-
Adult dose for HSV, HIV-associated (treatment) - 500 mg q12h PO for 7 d
-
Adult dose possible dose change for impaired renal function - CrCl 20-39 mL/min, 500 mg/d; CrCl < 20 mL/min, 250 mg/d
-
Pediatric dose – Not established
-
Contraindications – Documented hypersensitivity to penciclovir or famciclovir
-
Interactions – Coadministration of probenecid or cimetidine may increase toxicity; coadministration increases bioavailability of digoxin
-
Precautions – Caution in renal failure or coadministration of nephrotoxic drugs
-
Pregnancy – Category B; fetal risk not confirmed in studies in humans but has been shown in some studies in animals
Penciclovir, topical (Denavir) details are as follows:
-
Description – Taken up by infected cells. Metabolized by viral thymidine kinase to penciclovir triphosphate. Active drug inhibits viral DNA synthesis, thereby inhibiting viral replication. Treatment of initial and recurrent non–life-threatening mucocutaneous HSV infections in nonimmunocompromised patients. Has in vitro inhibitory activity against HSV-1 and HSV-2. Minimal systemic absorption following topical administration. Has not been detected in urine of male volunteers following daily topical application at doses 67 times higher than estimated clinical dose.
-
Adult dose – Apply to affected area q2h for 4 d; apply sufficient quantity to adequately cover all lesions
-
Pediatric dose – Not established
-
Contraindications – Documented hypersensitivity to penciclovir or famciclovir
-
Interactions – None reported
-
Precautions – Adverse effects may include hypoesthesia, taste perversion, and erythematous rash; with breastfeeding, small amount absorbed across disease tissues and because total daily topical dose is small, it is unlikely that significant amount is distributed in breast milk; adverse effects profile in elderly patients comparable to that in younger patients, but appropriate studies have not been performed; avoid contact with eyes; in missed dose, apply as soon as possible but do not apply if almost time for next dose
-
Pregnancy – Category B; fetal risk not confirmed in studies in humans but has been shown in some studies in animals
-
Human herpesvirus (HHV) type 1. Primary herpetic gingivostomatitis often affects children or young adults. The initial clinical presentation can be severe, with vesicles throughout the oropharynx and perioral skin, in contrast to the much more limited presentation typical of recurrent herpes. Courtesy of A.K. ElGeneidy, DDS.
-
Human herpesvirus (HHV) type 1. Additional intraoral view of the same patient in Image 1. Note the redness around the marginal gingiva, representing healing ulcers, which days earlier would have appeared as vesicles. This extensive ulceration often makes eating painful. Courtesy of A.K. ElGeneidy, DDS.
-
Human herpesvirus (HHV) type 1. Primary herpes can affect the lips, and the ruptured vesicles may appear as bleeding of the lips (same patient as in Images 1-2). Courtesy of A.K. ElGeneidy, DDS.
-
Human herpesvirus (HHV) type 1. Recurrent herpes is most often noted clinically as herpes labialis, with clustered vesicles (often coalescing) on the lip vermilion and often on the perioral skin. Recurrences generally occur in the same area each time, although their severity may vary.
-
Human herpesvirus (HHV) type 1. Recurrent herpes is occasionally observed intraorally. Inside the oral cavity, recurrent herpes typically affects only keratinized tissues, such as the gingiva or the hard palate. Vesicles often break quickly, so the clinician may observe small clustered ulcers. Courtesy of Sheldon Mintz, DDS.
-
Human herpesvirus (HHV) type 3. The initial manifestation of Varicella-Zoster Virus infection is chickenpox (varicella), and vesicular lesions may be noted on the oral mucosa in addition to the characteristic and better-known skin lesions.
-
Human herpesvirus (HHV) type 3. Intraoral herpes zoster closely resembles recurrent HHV-1 infection, but the lesions generally follow a dermatome and stop sharply at the midline, as shown here. However, the rules for common sites of occurrence of HHV-1 and HHV-3 often do not apply to patients who are immunocompromised. Courtesy of Sheldon Mintz, DDS.
-
Human papillomavirus (HPV). Verruca vulgaris on the lateral border of the tongue exhibits the multiple, sharp-tipped, white, verrucous appearance, which is classic for this lesion in the oral cavity. Not all verrucae are so clinically diagnostic. Courtesy of Rose Yin Geist, DDS.
-
Human papillomavirus (HPV). This verruca on the retromolar pad shows much less keratinization and a broader base. Verrucae and papillomas may be difficult to differentiate, but both are usually surgically excised.
-
This is a verruca vulgaris of the anterior maxillary gingiva in a healthy young male. He had recently resolved a wart on his finger.
-
Papillomas, which are of questionable viral origin, are frequent findings in the oral cavity, especially on the lateral/ventral tongue and soft palate.
-
These small papillomas on the lateral tongue of a young woman showed histologic evidence of HPV in the form of extensive koilocytosis.
-
Multiple condylomas are seen in this HIV+ male with a CD4 count of 11, and recent neurosyphilis.
-
Human papillomavirus (HPV). Condyloma acuminatum of the oral cavity usually appears as a pinker, more cerebriform lesion (as shown here) compared with the whiter, more verrucous appearance of verruca vulgaris. Courtesy of A.K. ElGeneidy, DDS.
-
Human papillomavirus (HPV). Some patients with condyloma acuminatum present with multiple oral lesions. Lesion on the lingual frenum occurred in the same man shown in Image 14. Courtesy of A.K. ElGeneidy, DDS.
-
Human papillomavirus (HPV). Condylomata on the lower lip, as well as other sites at the initial presentation (same patient as in Images 14-15). This presentation is unusually extensive. Multiple condylomata may be synchronous or metachronous. This patient did not present with genital condylomata; however, the appropriate health care practitioner should examine patients with condyloma to determine the extent of the disease. The source of infection (eg, a partner who is infected) should also be determined and treated. Courtesy of A.K. ElGeneidy, DDS.
-
A mnemonic for remembering the microscopic and clinical shapes of verruciform oral lesions: Verruca vulgaris is shaped like a series of inverted V's. Condyloma acuminata are shaped like a series of C's placed on their sides. Papillomas are pedunculated like the letter P.
-
Human papillomavirus (HPV). Verrucae and papillomas appear as frondlike epithelial proliferations. Verrucae tend to be more keratinized with sharper projections than papillomas.
-
Human papillomavirus (HPV). Condyloma acuminatum generally has a papillary architecture and may microscopically resemble verruca vulgaris and papilloma (hematoxylin and eosin stain, original magnification X10). Courtesy of AK ElGeneidy, DDS.
-
Human papillomavirus (HPV). Koilocytes in the upper epithelium are a helpful, although not completely reliable, indication that a lesion is associated with human papillomavirus. Koilocytes display a dark small nucleus with clear cytoplasm (hematoxylin and eosin stain, original magnification X100). Courtesy of Sheldon Mintz, DDS.
-
Human papillomavirus (HPV). Condyloma acuminatum may show brisk mitotic activity, although oral condyloma acuminatum is not considered a premalignant lesion (hematoxylin and eosin stain, original magnification X40). Courtesy of A.K. ElGeneidy, DDS.
-
Human papillomavirus (HPV). Heck disease in the buccal mucosa of a 7-year-old boy. Courtesy of Sheldon Mintz, DDS.
-
This patient with mumps has marked bilateral swelling of the salivary glands. Courtesy of Sheldon Mintz, DDS.
-
A 21-year-old woman with infectious mononucleosis presents with a petechial lesion on her palate.
-
Lesions on the buccal mucosa caused by human papillomavirus.











