Overview
Coccidioidomycosis is caused by Coccidioides immitis, a dimorphic soil fungus native to the San Joaquin Valley of California, southern portions of Arizona, northern portions of Mexico, and scattered areas in Central America and South America, including Colombia. [1, 2, 3] It may be a neglected disease in rural northeast Brazil. [4] There is a possible endemic focus in China. [5] Imported endemics can occur anywhere along with migratory movements, with 94 patients described in Spain from clinical records in the years 1997-2014. [6] Coccidioidomycosis in California has increased more than 213%, from 6 cases per 100,000 population in 2014 to 18.8 cases per 100,000 population in 2017 and continues to do so. [7]
C immitis propagates as a saprophyte and as a parasite. In soil, it grows as a mold with branching septate hyphae. When the soil is disturbed, the hyphae fragment, which forms extremely hardy structures called arthroconidia, can become airborne. If inhaled by animals or humans, the arthroconidia can reach the pulmonary alveoli and transform into thick-walled, multinucleate spherules, which form septa and produce hundreds to thousands of uninucleate endospores. Each endospore is capable of producing new spherules or mycelia. With large-scale soil disturbance in Southern California’s Antelope Valley due to increased population, an increased incidence should be anticipated if land developers ignore the risk of grading land without implementing long-term dust mitigation plans. [8] In addition, global temperature rise has allegedly enhanced the geographic distribution of this fungus. [9]
Most infected individuals are without symptoms. Disseminated coccidioidomycosis is unusual. Immunosuppressed people and pregnant women with coccidioidomycosis should receive special attention because of the increased risk of dissemination. US military service members of Asian/Pacific Islander race assigned in endemic regions of the American Southwest have a significantly higher incidence rate of extrapulmonary disease compared with members of other racial/ethnic groups. [10] Rarely, disseminated coccidioidomycosis with cutaneous involvement may clinically mimic a cutaneous T-cell lymphoma. Primary cutaneous coccidioidomycosis is rare. [11]
Note the images below.
See A Chronic, Scaly Rash Mistaken for MRSA: Case Presentation, a Critical Images slideshow, to review additional images and details of a case of Coccidioidomycosis.
Go to Coccidioidomycosis, Ocular Coccidioidomycosis, and Coccidioidomycosis Imaging for complete information on these topics.
Patient History
The triad of fever, erythema nodosum, and erythema multiform may occur. Erythema nodosum and erythema multiform have a strong predilection for female patients. Migratory arthralgias are common.
There may be a history of travel or residence in an endemic area. It may also be considered an occupational disorder, as exemplified by an outbreak among highway construction crews in a highly endemic area, Kern County, California. [12] Although one tends to think of spores aerosolized in dust storms in Arizona and California producing outbreaks of coccidioidomycosis, an outbreak has been linked to a California earthquake. [13] In HIV-infected and other immunocompromised patients, one should be particularly concerned about possible mycotic co-infections, including with coccidioidomycosis, [14] which, in nonendemic areas, may be particularly perplexing. [15] Diabetes mellitus and black race may be risk factors for disseminated disease, justifying a California court decision exclusion of black inmates and those with diabetes from the two California prisons. [16]
Physical Examination
The skin is the most common site of dissemination. Involvement ranges from superficial maculopapules, keratotic nodules, and verrucous ulcers to subcutaneous fluctuant abscesses. (Nonhealing skin lesions may need to be evaluated by means of biopsy.) Cold subcutaneous abscesses may be the first or only sign of disseminated infection. [17] The morphology varies. Dissemination should be especially considered in the immunosuppressed, including liver transplant recipients, and may appear as firm, violaceous subcutaneous nodules. [18]
The lesions have a predilection for the nasolabial fold.
Erythema nodosum and erythema multiforme may occur; as previously stated, these have a strong predilection for female patients. Erythema nodosum may manifest as painful subcutaneous nodules and are typically located on the lower extremities. Erythema nodosum may be the first sign of systemic disease. Less commonly, erythema multiforme may develop instead of erythema nodosum, resulting in the typical target lesions. The triad of fever, erythema nodosum, and arthralgias is called desert rheumatism.
Buot et al reported finding specific cutaneous lesions of coccidioidomycosis during placement of a ventricular cardiac shunt for chronic meningitis. [19]
Skin Testing
Testing is available in the United States for assessing the cellular immune response in persons with coccidioidomycosis. Data suggest that archived coccidioidin retains its potency and specificity and that in vitro tests of coccidioidal immunity may have utility in the measurement of coccidioidal cellular immunity. Combined antibody and antigen detection to facilitate the diagnosis of coccidioidomycosis is desirable. [20] The diagnosis may have been missed if antigen detection was not performed. Furthermore, coccidioidal skin testing can be a useful epidemiologic and clinical tool for monitoring treatment response. [21]
A dermal delayed-type hypersensitivity reaction to coccidioidin is highly specific for coccidioidal infection. However, a positive result may not be related to currently acquired disease, because, in most persons, this skin test result remains positive for life after infection.
Although skin test results are useful for epidemiologic studies, the test has important limitations when it is used as a screening procedure for recent infections with C immitis.
In patients in whom coccidioidomycosis is diagnosed with the help of other tests, the results of skin testing may have prognostic significance.
With skin testing, the induration of the skin is measured at 24 hours and 48 hours after coccidioidin is injected intradermally. An induration greater than 5 mm is considered reactive. Erythema at the injection site does not aid in the diagnosis of coccidioidomycosis.
Histologic Findings
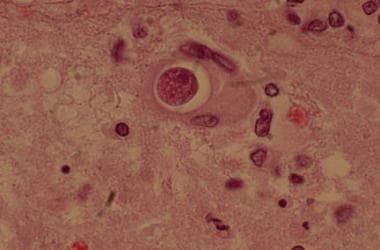
Cutaneous coccidioidomycosis with verrucous nodules tends to have an overlying hyperplastic epidermis with a dermal granuloma. Characteristic spores may be evident in the granuloma. Caseation necrosis may also be present. [22]
Primary inoculation disease results in a dense, mixed, inflammatory dermal infiltrate with occasional giant cells and the formation of small abscesses. Spores may be evident, although hyphae are less likely to be present.
The occasionally associated erythema nodosum has typical histologic features, with no alterations suggestive of coccidioidomycosis. The same is true of erythema multiforme, which is less commonly linked to coccidioidomycosis.
Treatment & Management
The need for surgery is determined by the nature of specific lesions on a case-by-case basis, because the manifestations, locations, and severity of progressive forms of coccidioidomycosis vary greatly among patients. Scanning with the F18-fluorodeoxyglucose (FDG) PET/CT imaging modality may be well suited to evaluate the extent of disseminated infection. [23] Fluconazole, the most commonly used antifungal for various forms of coccidioidomycosis, may be associated with a variety of skin effects, including dry skin and lips and alopecia. [24]
In some patients, especially those with extensive dermal involvement, debridement and drainage of the infected sites may be critical in controlling the infection.
A reason for performing this procedure may be that the spherule wall, a strong stimulus for inflammation, cannot be degraded easily or cleared from large coccidioidal lesions by macrophages and other elements of the reticuloendothelial system.
Therefore, even if therapy is effective in arresting fungal proliferation, fungal debris that is already present may continue to cause tissue destruction until it is surgically removed.
Use of tumor necrosis factor-α inhibitors for underlying inflammatory bowel disease was associated with an enhanced likelihood acquired coccidioidomycosis dissemination. [25]
-
Soft tissue abscess due to cocci.
-
Pulmonary cocci spherule (hematoxylin and eosin stain).