Overview
Within the specific context of 30,000 new cases of oral and pharyngeal cancer diagnosed each year in the United States and the associated 9000 deaths is the broader picture of individuals with potentially detectable precancerous lesions. Most cases include patients with asymptomatic oral and oropharyngeal mucosal alterations. The nature and behavior of these asymptomatic oral and oropharyngeal mucosal alterations may remain uncertain to the clinician. This has been emphasized to the public and to the professions in an effort to increase awareness of this disease, with the goal of early detection and thus improved end point results. [1]
Identification of each lesion in a safe and accurate fashion presumes that the person with the mucosal abnormality presents to a practitioner who possesses a level of understanding concerning mucosal abnormalities of the upper aerodigestive tract and/or oral cavity, that is to say, the oropharynx. This is emphasized within the context of Bouquot's study in 1986, which noted that as many as 10% of American adults have some form of oral abnormality. [2] The clinician wishing to investigate identified abnormalities may use a scalpel biopsy or a punch biopsy to obtain a representative tissue sample for pathologic analysis.
The most definitive, accurate, and reliable method for diagnosing oral mucosal abnormalities has been and remains the scalpel biopsy. However, when presented with the need to have an oral or oropharyngeal mucosal biopsy performed, the patient is often reluctant, and at times fearful, of such an invasive surgical procedure. The patient's reluctance may be compounded by the clinician's hesitation to perform a surgical procedure in an unfamiliar location or anatomical site. The clinician may be generally unfamiliar concerning the performance of any form of intraoral or upper aerodigestive tract biopsy.
In contrast to the sampling of cells of the uterine cervix, analysis of surface epithelial cells of the oral cavity and oropharynx by standard exfoliative cytology has proven to be unreliable in identifying as many as 31% of dysplastic lesions as demonstrated in one study. [3] Obtaining and sampling cells within the basal and parabasal region of the epithelium is central to the consistent and accurate diagnosis of early oral and oropharyngeal cancer or precancer. Although the standard scalpel biopsy accomplishes accurate identification of such changes, a less complex but consistent diagnostic approach with high levels of sensitivity and specificity would be welcomed within the practicing community.
With this in mind, the development of the brush biopsy (Oral CDx R) coupled with a computer-assisted method of analysis has brought accurate diagnosis, ease of performance, and patient acceptance into daily practice. The accuracy of this diagnostic modality has been noted beyond the initial studies, with positive predictive values of atypical and positive brush biopsy results being greater than 44%. [4] In contrast to traditional exfoliative cytology, the brush biopsy, using a specially designed circular bristled brush, is able to access and sample all epithelial layers, including the basal cell layer and the most superficial aspects of the lamina propria. Thus, the cellular material obtained is a true representation of all epithelial layers in a disaggregated form spread over the surface of an ordinary glass slide. In addition, this technique has been applied to other forms of analysis, including DNA image cytometry. [5, 6, 7, 8]
In 2008, Mehrotra et al emphasized the value of the brush biopsy technique in evaluating oral lesions without the aid of computer-assisted technology, although they reported marginally lower sensitivity and specificity. The emphasis was to put this valuable approach into widespread use in communities where resources are limited but the need is high. [9] More recently, the efficacy of this technique has been reported with a positive predictive value of 84% and negative predictive value of 98% in cases that were deemed minimally suspicious. [10] In a study of 70 cases of clinically suspicious oral mucosal lesions without evidence of malignancy, the brush biopsy was noted to provide a sensitivity of 55% and corresponding specificity of 100%. [11]
This technique has been used in conjunction with toluidine blue staining, with affirmation of the high degree of sensitivity and sensitivity for malignant lesions. [12] Further studies using analytical tools, including mass spectrometry in conjunction with brush biopsy specimens in distinguishing healthy and malignant oral mucosal tissue and between cancer and other noncancerous lesions have shown overall accuracy of 96.5%. [13]
Clinical Indications
The use of brush biopsy with computer-assisted analysis has wide clinical application in assessment of surface oral and oropharyngeal mucosal abnormalities, which include leukoplakia; erythroplakia; and mixed red and white lesions, such as erythroleukoplakia and speckled leukoplakia (see the images below). Early assessment of such lesions, leading to prompt identification of dysplastic preinvasive or early minimally invasive disease, is central to eliminating these lesions; additionally, it eliminates any uncertainty concerning the identity or characteristics of a surface oral mucosal abnormality that may represent a dysplastic or frankly malignant lesion. [14] This permits high cure rates even in cases where invasive disease is noted on subsequent scalpel biopsy. The broader application and further use of this procedure concerns the oral mucosal lesion that normally would otherwise not be indicated or subjected to scalpel biopsy. [15]
 A focal, slightly firm, and minimally elevated lesion on the left lateral part of the tongue is shown. Benign epithelial cells were noted on the brush biopsy, indicating a focal benign keratosis.
A focal, slightly firm, and minimally elevated lesion on the left lateral part of the tongue is shown. Benign epithelial cells were noted on the brush biopsy, indicating a focal benign keratosis.
 A 27-year-old woman with patchy, focally thickened, keratotic lesions over the right lateral and ventral tongue surfaces. Brush biopsy results indicated the presence of atypical cells leading to a scalpel biopsy, which proved the presence of focal moderate dysplasia.
A 27-year-old woman with patchy, focally thickened, keratotic lesions over the right lateral and ventral tongue surfaces. Brush biopsy results indicated the presence of atypical cells leading to a scalpel biopsy, which proved the presence of focal moderate dysplasia.
 A mixed red and white lesion on the right ventral part of the tongue with atypical brush biopsy results and corresponding severe dysplasia by scalpel biopsy.
A mixed red and white lesion on the right ventral part of the tongue with atypical brush biopsy results and corresponding severe dysplasia by scalpel biopsy.
 Initially, a biopsy was performed on this well-defined velvety patch of the maxillary alveolar ridge using the brush system, followed by excision because of the presence of positive cells as noted by the computer-assisted brush biopsy. The surgical specimen confirmed the presence of carcinoma in situ.
Initially, a biopsy was performed on this well-defined velvety patch of the maxillary alveolar ridge using the brush system, followed by excision because of the presence of positive cells as noted by the computer-assisted brush biopsy. The surgical specimen confirmed the presence of carcinoma in situ.
Lesions that require brush biopsy include unexplained clinically detectable alterations of the surface epithelium, whether cancer or precancer is suspected. This was emphasized in a multicenter study where nearly 5% of clinically benign-appearing mucosal lesions were sampled by this technique and later confirmed by typical scalpel biopsy to represent dysplastic epithelial changes or invasive cancer. [16] Other authors have also demonstrated the ability of the brush biopsy to uncover similar type lesions that were not clinically suspicious for carcinoma or preinvasive disease. [17] This latter study also amplified the efficacy of this technique by showing a positive predictive value of 38% by comparing brush biopsy results with subsequent scalpel biopsy analysis.
This author stresses the potential for development of invasive cancer caused by overlooking or downplaying the significance of clinically abnormal mucosa when the physician engages in a watchful waiting strategy in the absence of reliable and accurate tissue sampling and analysis. [18] Focus attention on the identification of an abnormality of the oral mucosal surface, the presence of persistent previously diagnosed benign surface lesions, or follow-up care of previously treated oral cancer or preinvasive cancer/dysplasia (see below).
 During a routine postradiation therapy examination, a focal red granular surface lesion was detected. Brush biopsy was helpful in noting the presence of positive cells, whereas scalpel biopsy helped in the identification of recurrent invasive squamous cell carcinoma.
During a routine postradiation therapy examination, a focal red granular surface lesion was detected. Brush biopsy was helpful in noting the presence of positive cells, whereas scalpel biopsy helped in the identification of recurrent invasive squamous cell carcinoma.
From the clinical perspective, the white or leukoplakic lesion or such lesions with an erythematous component (erythroplakia) have a widely variable presenting appearance, are often asymptomatic, and may appear innocuous (see the image below). Furthermore, more worrisome-appearing lesions may ultimately exhibit benign, reactive, or inflammatory cellular abnormalities when a biopsy is performed. Such lesions are in a dynamic state, changing appearance in a relatively rapid time frame [19] ; therefore, clinicians are not always able to accurately characterize or predict the behavior of such alterations based on the clinical characteristics alone. In the past, traditional histologic evaluation of these lesions has been recommended as a matter of routine. [20]
 A biopsy using the brush technique was performed on this relatively innocuous superficial erosion at the distal edge of a linear white lesion. An atypical result led to excision of the lesion with the presence of moderate dysplasia and dyskeratosis.
A biopsy using the brush technique was performed on this relatively innocuous superficial erosion at the distal edge of a linear white lesion. An atypical result led to excision of the lesion with the presence of moderate dysplasia and dyskeratosis.
One manner of sampling the broad array of white and red-white oral lesions is by way of the brush biopsy technique. This efficient and readily accepted form of tissue biopsy allows the clinician access to the full thickness of the involved epithelial layer, harvesting and delivering cells to a slide followed by fixation. This technique's ease of use, absence of the need for a local anesthetic agent, trivial bleeding, and lack of need for suturing has made clinical acceptance universal.
Clinical Technique
Use of the brush biopsy technique involves the use of a specially designed circular brush, which is used to sample the epithelial lesion in question. Details of sampling within the context of the family physician or nonspecialist were described by Naugler, with emphasis on the initial use of this technique over excisional biopsy. [21]
The brush may be moistened with water or the patient's saliva and applied to the surface of the lesion. Contact between the brush and the mucosal surface may be along either the flat end or the rounded surface, with moderate pressure applied (see the first image below). The brush is then rotated until pinpoint bleeding is noted, signaling entry into the lamina propria and, thus, obtaining epithelial cells through the full-thickness of the epithelium (see the second image below). Removed cells are transferred to a glass slide by distributing the obtained material evenly over the glass surface. A fixation step follows immediately by flooding the slide with fixative solution (alcohol/propylene glycol) and allowing it to air dry.
 Firm, circular rotation of the head of the supplied brush is performed over the surface of an alteration on the ventral part of the tongue.
Firm, circular rotation of the head of the supplied brush is performed over the surface of an alteration on the ventral part of the tongue.
 At the notice of superficial perforation of the epithelium by virtue of pinpoint bleeding, the brush biopsy is completed. The clinician is assured of a full-thickness epithelial sampling, which is transferred to the glass slide and immediately flooded with fixative solution.
At the notice of superficial perforation of the epithelium by virtue of pinpoint bleeding, the brush biopsy is completed. The clinician is assured of a full-thickness epithelial sampling, which is transferred to the glass slide and immediately flooded with fixative solution.
Upon completion of air-drying of the fixative, the cellular sample on the slide is stained with a modified Papanicolaou method and scanned by an automated computer-driven microscope system.
Neural network-based image processing software specifically tailored and designed for detection of oral mucosal premalignant and malignant cells is used to analyze the stained and scanned slides. Any abnormality in cell morphology, including altered cell size, degree of keratinization, nuclear staining intensity, and size are characterized and analyzed. Images produced by this software are further analyzed and refined to the level in which as few as 2 abnormal cells among thousands of other keratinocytes, inflammatory cells, erythrocytes, and debris can be detected within the brush biopsy specimen.
Once identified by the software, a pathologist reviews the images of the detected abnormal cells on a high-resolution monitor for verification. Once verified, specimens are classified as negative (ie, no epithelial abnormality), atypical (ie, abnormal epithelial cells, but of uncertain diagnostic significance), and positive (ie, unequivocal). In one small study, an extension of this sampling technique involved the use of DNA image cytometry as an adjunctive method to determine the degree or presence of aneuploidy [5]
Finally, in cases in which a full-thickness (transepithelial) specimen was not obtained, an inadequate reading is offered, which signals the need for a repeat of the brush biopsy procedure (at no cost to the patient).
Upon receipt of a report and an accompanying digitized color image (see the image below) demonstrating the presence of atypical or positive cells, the clinician is mandated to perform a standard incisional/excisional scalpel biopsy, which renders a full architectural representation of all epithelial cells to each other and the underlying lamina propria. Therefore, a more traditional form of pathologic analysis follows from an abnormal result of a scanned and confirmed brush biopsy. Ease of use is emphasized by the absence of local or topical anesthetic, absence of an incision and associated suturing, and elimination of potential postoperative sequel. In cases in which an existing painful or tender lesion is to be sampled, a small amount of anesthetic solution may be deposited deep to the site of the biopsy. In such cases, do not use a topical anesthetic because distortion of epithelial cell morphology may result.
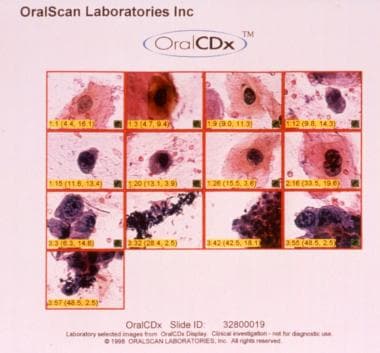 The clinician receives atypical or positive results in a digitized color format. This can be used as an aid to instruct the patient as to the significance of these findings and the need for further treatment.
The clinician receives atypical or positive results in a digitized color format. This can be used as an aid to instruct the patient as to the significance of these findings and the need for further treatment.
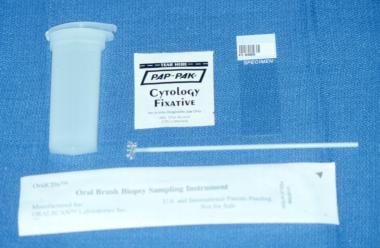
All components of the sampling procedure are contained in a kit, shown below, which includes instructions, a requisition form, a sterile brush, a glass slide, and a plastic slide container.
Conclusion
A simple, rapid, and highly accurate method is currently available for the assessment of oral epithelial abnormalities, which may include precancerous and cancerous lesions. [22]
Oral brush biopsy with computer-assisted analysis is highly valuable in such circumstances, with scalpel biopsy remaining the standard for arriving at a definitive diagnosis. The use of the technique in office practice offers the clinician a tool to help analyze surface oral mucosal abnormalities in a valid, scientifically based fashion. The clinical utility and corresponding degree of accuracy has been demonstrated; a positive predictive value of 44.1% for results related to atypical or positive findings has been noted. [4] Reddy et al noted that the sensitivity and specificity of the computerized analysis of oral brush biopsy specimens within the context of premalignant lesions had a positive predictive value of 58.3% and, with the use of molecular markers including tenascin and cytokeratins, accurate diagnostic results are achievable. [23]
Related Medscape Reference articles include Cancers of the Oral Mucosa and Noncandidal Fungal Infections of the Mouth, among others.
-
A focal, slightly firm, and minimally elevated lesion on the left lateral part of the tongue is shown. Benign epithelial cells were noted on the brush biopsy, indicating a focal benign keratosis.
-
A 27-year-old woman with patchy, focally thickened, keratotic lesions over the right lateral and ventral tongue surfaces. Brush biopsy results indicated the presence of atypical cells leading to a scalpel biopsy, which proved the presence of focal moderate dysplasia.
-
A mixed red and white lesion on the right ventral part of the tongue with atypical brush biopsy results and corresponding severe dysplasia by scalpel biopsy.
-
Initially, a biopsy was performed on this well-defined velvety patch of the maxillary alveolar ridge using the brush system, followed by excision because of the presence of positive cells as noted by the computer-assisted brush biopsy. The surgical specimen confirmed the presence of carcinoma in situ.
-
During a routine postradiation therapy examination, a focal red granular surface lesion was detected. Brush biopsy was helpful in noting the presence of positive cells, whereas scalpel biopsy helped in the identification of recurrent invasive squamous cell carcinoma.
-
A biopsy using the brush technique was performed on this relatively innocuous superficial erosion at the distal edge of a linear white lesion. An atypical result led to excision of the lesion with the presence of moderate dysplasia and dyskeratosis.
-
Firm, circular rotation of the head of the supplied brush is performed over the surface of an alteration on the ventral part of the tongue.
-
At the notice of superficial perforation of the epithelium by virtue of pinpoint bleeding, the brush biopsy is completed. The clinician is assured of a full-thickness epithelial sampling, which is transferred to the glass slide and immediately flooded with fixative solution.
-
The clinician receives atypical or positive results in a digitized color format. This can be used as an aid to instruct the patient as to the significance of these findings and the need for further treatment.
-
Contents of the diagnostic kit include the sterile circular brush, a barcode-labeled slide, a fixative pouch, and a plastic transport container. Also included is a history form with a barcode corresponding to that on the slide and a prepaid Express Mail container.