Practice Essentials
Tooth discoloration is caused by multiple local and systemic conditions. [1] (See the image below.) Discoloration colors include brown, black, gray, green, orange, and yellow; on occasion, a metallic sheen is present.
Signs and symptoms
In most patients, the chief complaint is related to aesthetics. Some patients, however, may present initially with pain in addition to discoloration.
See Presentation for more detail.
Diagnosis
The patient's history provides useful information regarding the etiology of the discoloration. The scratch test is generally used to distinguish between extrinsic and intrinsic discoloration.
Dental radiographs can reveal defects in both tooth structure and alveolar bone. This information is critical for the identification of a potential cause of intrinsic discoloration.
See Workup for more detail.
Management
Dental treatment of tooth discoloration involves identifying the etiology and implementing therapy. The following treatments may be used:
-
Modification of diet and habits
-
Toothbrushing
-
Professional tooth cleaning
-
Enamel microabrasion
-
Bleaching (tooth whitening)
Surgical interventions include dental restorations, extractions, and implantations.
See Treatment for more detail.
Background
By this point in the 21st century, the treatment of tooth discoloration has evolved into an annual multibillion-dollar, highly sophisticated, scientific, and clinical discipline. However, the origins of the treatment date back thousands of years to ancient clinicians and beauticians who used rudimentary, yet innovative, natural materials to mask undesirable tooth discolorations.
Function
The oral cavity plays 3 important roles in the protection and preservation of systemic health; it is involved in nutritional intake, communication, and host defense. The teeth are involved in all 3 roles, and dental diseases can be a source of multiple problems, including oral and systemic infections and difficulty in chewing, swallowing, or phonation.
Anatomy
Cursory familiarity with basic dental anatomy and calcification and with the eruption sequence of teeth is helpful before physical examination. A tooth is composed of a crown (ie, the portion exposed to the oral cavity) and 1 or more roots (ie, the portion enveloped in bone and the periodontium). The crown of each tooth has 5 surfaces: buccal (facing the cheek or lip), lingual (facing the tongue), mesial (between the teeth), distal (between the teeth), and chewing (occlusal for molars and premolars, incisal for incisors and canines).
In the transverse section, the tooth has 3 distinct layers. These include a surface enamel layer covering only the crown; an inner layer of dentin in both the crown and root; and the core area known as the pulp, which contains nerves, arteries, and veins. Radiographically, the layers are easily identifiable because they have different radiopacities. Enamel is the most mineralized of the calcified tissues of the body, and it is the most radiopaque of the 3 tooth layers. Dentin is less radiopaque than enamel and has a radiopacity similar to that of bone. The pulp tissue is not mineralized and appears radiolucent. Note the image below.
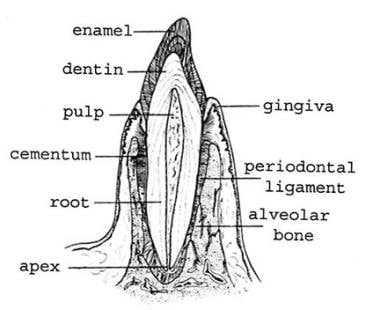 Transverse section of a central incisor illustrates the different soft and hard tissue layers of the tooth and the supporting dental-alveolar apparatus.
Transverse section of a central incisor illustrates the different soft and hard tissue layers of the tooth and the supporting dental-alveolar apparatus.
Primary (ie, deciduous) teeth number 20, and secondary (ie, adult) teeth number 32. A phase of mixed dentition exists, depending on the age of the patient (typically, 6-14 y). This phase is associated with simultaneous exfoliation or the eruption of primary and secondary teeth (see Tables 1-2).
Table 1. Calcification and Eruption Sequence of Primary Dentition (Open Table in a new window)
|
Primary Teeth Calcification Begins (Weeks In Utero) |
Enamel Completed (Months after Birth) |
Eruption (Months after Birth) |
Maxilla |
|
|
|
Central incisor |
13-16 |
1.5 |
8-12 |
Lateral incisor |
14.5-16.5 |
2.5 |
8-13 |
Canine |
15-18 |
9 |
16-22 |
First molar |
14. 5-16.5 |
6 |
13-19 |
Second molar |
16-23.5 |
11 |
25-33 |
Mandible |
|
|
|
Central incisor |
13-16 |
2.5 |
6-10 |
Lateral incisor |
14.5-16.5 |
3 |
10-16 |
Canine |
16-18 |
9 |
17-23 |
First molar |
14.5-17 |
5.5 |
14-18 |
Second molar |
17-19.5 |
10 |
23-31 |
Table 2. Calcification and Eruption Sequence of Secondary Dentition (Open Table in a new window)
|
Permanent Teeth Calcification Begins (Months) |
Eruption (Years) |
Maxilla |
|
|
Central incisor |
3-4 |
7-8 |
Lateral incisor |
10-12 |
8-9 |
Canine |
4-5 |
11-12 |
First premolar |
8-21 |
10-11 |
Second premolar |
24-27 |
10-12 |
First molar |
0-1 |
5-6 |
Second molar |
30-36 |
12-13 |
Mandible |
|
|
Central incisor |
3-4 |
6-7 |
Lateral incisor |
3-4 |
7-8 |
Canine |
4-5 |
9-10 |
First premolar |
21-24 |
10-12 |
Second premolar |
27-30 |
11-12 |
First molar |
0-1 |
5-6 |
Second molar |
30-36 |
12-13 |
Pathophysiology
Tooth discoloration is caused by multiple local and systemic conditions. [1] Extrinsic dental stains are caused by predisposing factors and other factors such as dental plaque and calculus, foods and beverages, tobacco, chromogenic bacteria, metallic compounds, and topical medications. Intrinsic dental stains are caused by dental materials (eg, tooth restorations), dental conditions and caries, trauma, infections, medications, nutritional deficiencies and other disorders (eg, complications of pregnancy, anemia and bleeding disorders, bile duct problems), and genetic defects and hereditary diseases (eg, those affecting enamel and dentin development or maturation).
Causes of Extrinsic Discoloration
Extrinsic stains are defined as stains located on the outer surface of the tooth structure and caused by topical or extrinsic agents.
The Nathoo classification system of extrinsic dental stain describes 3 categories as follows [2] :
-
Nathoo type 1 (N1): N1-type colored material (chromogen) binds to the tooth surface. The color of the chromogen is similar to that of dental stains caused by tea, coffee, wine, chromogenic bacteria, and metals.
-
Nathoo type 2 (N2): N2-type colored material changes color after binding to the tooth. The stains actually are N1-type food stains that darken with time.
-
Nathoo type 3 (N3): N3-type colorless material or prechromogen binds to the tooth and undergoes a chemical reaction to cause a stain. N3-type stains are caused by carbohydrate-rich foods (eg, apples, potatoes), stannous fluoride, and chlorhexidine.
Predisposing factors
Certain factors predispose children and adults to extrinsic stains, including enamel defects, salivary dysfunction, and poor oral hygiene. [3] Microscopic pits, fissures, and defects in the outer surface of the enamel are susceptible to the accumulation of stain-producing food, beverages, tobacco, and other topical agents.
Because saliva plays a major role in the physical removal of food debris and dental plaque from the outer and interproximal tooth surfaces, diminished salivary output contributes to extrinsic discoloration. Decreased output may be caused by local disease (eg, salivary obstructions and infections), systemic disease (eg, Sjögren syndrome), head and neck radiation therapy for cancer, chemotherapy, and multiple medications (eg, anticholinergics, antihypertensives, antipsychotics, antihistamines).
The most common cause of extrinsic stains is poor oral hygiene. [3] The inability to remove stain-producing materials and/or the use of dentifrices with inadequate cleaning and polishing actions cause discolorations.
Other factors
Accumulations of dental plaque, calculus, and food particles cause brown or black stains. Note the images below.
Deposition of tannins found in tea, coffee, and other beverages cause brown stains on the outer (buccal, labial) and inner (lingual, palatal) surfaces of the teeth.
Tobacco stains from cigarettes, cigars, pipes, and chewing tobacco cause tenacious dark brown and black stains that cover the cervical one third to one half of the tooth (midway on the tooth toward the gingival margin). Note the image below.
Pan (a combination of betel nut of the areca palm, betel leaf, and lime) is commonly chewed by more than 200 million persons in the western Pacific basin and South Asian region. [4] It is used for its mild psychoactive and cholinergic effects, and it elicits a copious production of blood red saliva that results in a red-black stain on the teeth, gingiva, and oral mucosal surfaces. Note the image below.
 Image demonstrates a red extrinsic stain at the gingival margins and interproximal and incisal regions of the teeth in a patient with a habit of chewing pan (a combination of betel nut of the areca palm, betel leaf, and lime).
Image demonstrates a red extrinsic stain at the gingival margins and interproximal and incisal regions of the teeth in a patient with a habit of chewing pan (a combination of betel nut of the areca palm, betel leaf, and lime).
Chromogenic bacteria cause stains, typically at the gingival margin of the tooth. The most common is a black stain caused by Actinomyces species. The stain is composed of ferric sulfide and is formed by the reaction between hydrogen sulfide produced by bacterial action and iron in the saliva and gingival exudates. [5] Green stains are attributed to fluorescent bacteria and fungi such as Penicillium and Aspergillus species. [3] The organisms grow only in light and therefore cause staining on the maxillary surface of the anterior teeth. Orange stain is less common than green or brown stains and is caused by chromogenic bacteria such as Serratia marcescens and Flavobacterium lutescens.
Metallic compounds are also implicated in dental discolorations because of the interaction of the metals with dental plaque to produce surface stains. [3] Industrial exposure to iron, manganese, and silver may stain the teeth black. Mercury and lead dust can cause a blue-green stain; copper and nickel, green–to–blue-green stain; chromic acid fumes, deep orange stain; and iodine solution, brown stain.
Topical medications cause staining. Chlorhexidine rinse (0.12%) causes brown staining after several weeks of use, particularly on acrylic and porcelain restorations. Note the image below.
A study on the effectiveness of chlorhexidine dentifrice or gel (CHX DF/gel) compared to chlorhexidine mouthwash (CHX MW) on plaque, bleeding, gingival inflammation and tooth discoloration scores reported that significantly more tooth discoloration was observed with the CHX MW however altogether, when daily oral hygiene cannot be performed, CHX MW is the first product of choice. [6]
Cetylpyridinium chloride is an ingredient in several mouthwashes (eg, Cepacol, Scope) that can cause dental staining. [7] Iron-containing oral solutions used for treatment of iron deficiency anemia cause black stains. Potassium permanganate mouthwash (violet-black stain), silver nitrate (black stain), and stannous fluoride (brown stain) also can induce dental discolorations. [3] Some systemic medications (eg, minocycline, doxycycline) can cause extrinsic staining. See Medications in the Pathophysiology section below.
Causes of Intrinsic Discoloration
Numerous causes for intrinsic tooth discoloration exist. Stain distribution varies from localized (eg, 1 or 2 teeth) to a regional or generalized involvement of primary and secondary teeth. Localized discoloration may be a result of either preeruptive or posteruptive processes, whereas widespread involvement indicates a deviation in normal tooth formation. An understanding of the timing of tooth formation (particularly calcification and eruption sequences) can help explain the causes of intrinsic discoloration (see Causes).
Dental materials
Dental restorations most commonly cause intrinsic discoloration. Amalgam restorations can generate corrosion products (eg, silver sulfide), leaving a gray-black color in the tooth, especially in large cavity preparations with undermined enamel. Pins, composites, and glass ionomer and acrylic restorations gradually can leave a gray hue in the tooth adjacent to the material. Other dental materials that cause intrinsic discoloration include eugenol, formocresol, root canal sealers, and polyantimicrobial pastes. [3, 8]
Dental conditions and caries
Regarding attrition, abrasion, and erosion of tooth structure, as permanent teeth age, the dentition progressively becomes more gray and yellow. In the absence of extrinsic staining, this age-related phenomenon is due to a progressive loss in enamel from attrition or tooth wear that reveals the natural yellow color of underlying dentin. Note the image below.
 Image demonstrates dental attrition in a 75-year-old patient due to loss of occlusal enamel structure that reveals the underlying dentin.
Image demonstrates dental attrition in a 75-year-old patient due to loss of occlusal enamel structure that reveals the underlying dentin.
Areas of complete enamel loss are most commonly found on the incisal (chewing) surfaces of anterior teeth. This loss frequently occurs in older adults, whose teeth show a contrast in colors between enamel and dentin. Tooth abrasion manifests as yellow areas in which the enamel surface is lost (eg, buccal cervical regions) as a result of overzealous toothbrushing with a hard-bristled or medium-bristled toothbrush. Note the image below.
The erosion of enamel caused by frequent ingestion of acidic foods and beverages and from the regurgitation of acid from the stomach (eg, anorexia or bulimia nervosa) can lead to a yellow tooth discoloration. In patients with anorexia or bulimia, a yellow discoloration develops on lingual tooth surfaces where the acid reflux material makes contact with the teeth.
Certain tooth surfaces are at greater risk for dental caries. These surfaces include the occlusal grooves and pits of posterior teeth (class I caries), the smooth surfaces between teeth (class II caries for posterior teeth, class III caries for anterior teeth), and the smooth surfaces at the enamel-cementum interface at the free gingival margin (cervical, root surface, or class V caries). Caries also may involve the incisal edge of anterior teeth (class IV or VI). Note the image below.
The pathogenesis of dental caries begins with an incipient lesion confined to the enamel layer. Once the enamel layer is breached, caries tends to rapidly progress in the dentin, undermining the superficial enamel layer. Incipient carious lesions are associated with plaque accumulation and manifest as chalky white areas of discoloration secondary to hypocalcification.
Patients with orthodontic brackets are at great risk for caries because of suboptimal plaque removal. As caries progresses into the dentin, the overlying translucent enamel reveals the color of the underlying caries and appears yellowish brown. Extensive caries that involve destruction of both enamel and dentin produce a color that ranges from light brown, to dark brown or almost black as seen in the images below.
The brown color is attributed to the formation of Maillard pigments (reaction between proteins and small aldehydes produced by cariogenic bacteria), melanins, lipofuscins, and uptake of various food colors and bacterial pigments. [9] In some patients, the caries process can self-arrest, and remineralization may occur; however, the brown discolorations usually remain.
Trauma
Trauma to developing, yet unerupted, teeth can disturb enamel formation (amelogenesis) and may result in enamel hypoplasia, which is visualized as a localized opacity on the erupted tooth. Such teeth commonly are referred to as Turner teeth as seen in the image below. Unerupted permanent incisors commonly are affected after intrusion injuries to primary incisors in young children who fall on their faces.
 Severe enamel hypoplasia (ie, Turner tooth) on a secondary (permanent) maxillary central incisor. The patient had an intrusion injury of the primary central incisor during childhood that interrupted the development of the secondary central incisor.
Severe enamel hypoplasia (ie, Turner tooth) on a secondary (permanent) maxillary central incisor. The patient had an intrusion injury of the primary central incisor during childhood that interrupted the development of the secondary central incisor.
Trauma that occurs to erupted teeth also causes discoloration as seen in the images below. This discoloration frequently occurs in teeth that have fully formed roots and have sustained irreversible pulpal injury caused by avulsions, intrusions, luxations and subluxations, or fractures involving the pulp chamber.
 Severe enamel hypoplasia (ie, Turner tooth) on a secondary (permanent) maxillary central incisor. The patient had an intrusion injury of the primary central incisor during childhood that interrupted the development of the secondary central incisor.
Severe enamel hypoplasia (ie, Turner tooth) on a secondary (permanent) maxillary central incisor. The patient had an intrusion injury of the primary central incisor during childhood that interrupted the development of the secondary central incisor.
 Intrinsic dental discoloration caused by blunt trauma to the mandibular incisors that led to pulpal necrosis.
Intrinsic dental discoloration caused by blunt trauma to the mandibular incisors that led to pulpal necrosis.
Trauma can cause intrapulpal hemorrhage and iron sulfide deposition along the dentinal tubules, producing a bluish black cast.
Some occlusal trauma occurs over a protracted period of time (eg, excessive orthodontic forces). Rarely, this trauma leads to pulpal hemorrhage; however, it can produce a subtle grayish brown cast.
Infections
Periapical odontogenic infections of the primary teeth can disrupt normal amelogenesis of the underlying secondary (permanent) successors and involve a potential for localized enamel hypoplasia. Crown formation begins in utero; therefore, the potential for extensive intrinsic discoloration of the primary dentition may be present throughout pregnancy.
Although rare, maternal rubella or cytomegalovirus infection and toxemia of pregnancy can lead to tooth discoloration, which generally manifests as a focal opaque band of enamel hypoplasia that is confined to the primary teeth forming enamel at the time of maternal infection as seen in the image below.
 Enamel hypoplasia of the incisal half of the maxillary and mandibular secondary incisors caused by rubella infection when the patient was aged 4 months.
Enamel hypoplasia of the incisal half of the maxillary and mandibular secondary incisors caused by rubella infection when the patient was aged 4 months.
Crown formation of the secondary dentition occurs until the child is aged approximately 8 years. Systemic postnatal infections (eg, measles, chicken pox, streptococcal infections, scarlet fever) can also cause enamel hypoplasia. The bandlike discolorations on the tooth are visualized where the enamel layer has variable thickness and becomes extrinsically stained after tooth eruption.
Medications
Since the 1950s, drugs from the tetracycline family have been associated with intrinsic tooth discoloration. Once in the bloodstream, tetracycline can be incorporated into the calcification process of developing teeth, in which it affects either primary or secondary dentition after maternal or childhood ingestion, respectively.
Tetracyclines diffuse through dentin to the enamel interface, chelating calcium ions and incorporating into hydroxyapatite as a stable orthophosphate complex. The amount of drug incorporation is ultimately determined by the distribution of tooth discoloration and is equivalent to serum blood levels and the duration of exposure. When the affected teeth first erupt, they have a bright-yellow bandlike appearance that fluoresces under ultraviolet light, although upon exposure to sunlight, the color gradually changes to gray or red-brown. [10] Tetracycline use does not lead to discoloration once tooth formation is complete. Note the image below.
 Tetracycline staining of mandibular teeth caused by the ingestion of tetracycline when the patient was aged 3 years.
Tetracycline staining of mandibular teeth caused by the ingestion of tetracycline when the patient was aged 3 years.
Minocycline is a second-generation derivative of tetracycline. The ingestion of minocycline can lead to a green-gray or blue-gray intrinsic staining of teeth. Unlike with other tetracyclines, staining occurs during and after the complete formation and eruption of teeth. [11] Minocycline is a poor chelator of calcium ions, but it is believed to bind to iron ions. This binding causes the formation of insoluble salts that are either exuded from gingival crevicular fluid to extrinsically stain the enamel or intrinsically incorporated into the secondary dentin. [12] Minocycline is prescribed for long-term acne therapy in adolescents and adults, although it is being replaced by medications such as clindamycin and isotretinoin that do not cause tooth discoloration.
Doxycycline has recently been reported to cause extrinsic staining of teeth, [13, 14] possibly by binding to glycoproteins in the dental pellicle in patients with poor oral hygiene in whom oxidation occurs (eg, sunlight exposure, bacterial) or via mechanisms similar to those for minocycline.
Dental fluorosis is characterized by enamel discoloration resulting from subsurface hypomineralization due to the excessive ingestion of fluoride during the early maturation stage of enamel formation. [15]
Fluorosis affects primary and secondary dentitions with a broad range of clinical findings. In its mildest form, fluorosis appears as faint white lines or streaks on the enamel. Moderate fluorosis has more obvious opaque regions referred to as enamel mottling, whereas severe fluorosis appears with extensive mottling that readily chips and stains and leads to pitting and brown discoloration. Note the image below.
An increase in the prevalence of mild-to-moderate fluorosis has been observed in the United States over the last decade, even in areas with nonfluoridated public water supplies. [16] The trend is explained by early overuse and ingestion of fluoridated toothpaste; the inappropriate use of fluoride supplements; and in fluoridated areas, the use of powdered infant formula mixed with local water. Clinicians can help in preventing fluorosis by teaching parents about fluoride use and good toothbrushing habits for children.
Fluoride sources are numerous and include naturally or artificially fluoridated drinking water, commercially available beverages, foods prepared in fluoridated water, chewable vitamins, oral healthcare products (eg, toothpastes, mouthrinses, oral fluoride supplements), and professional fluoride products prescribed by dentists. The fluoride concentration of naturally fluoridated water varies depending on geographic location. For example, in some areas of Africa, the concentration may be as high as 10 parts per million (ppm), whereas many other regions have a concentration of 0 ppm. Artificially fluoridated water supplies usually have a fluoride concentration of 1 ppm. [17]
Similar to tetracycline exposure, the dose and duration of fluoride exposure in developing teeth is correlated with the extent and severity of the clinical findings. Several clinical indices have been developed to measure fluorosis. [18]
Kumar et al studied the impact of various medications on discoloration of the teeth. [19]
Nutritional deficiencies and other disorders
Regarding nutritional deficiencies, vitamins C and D, calcium, and phosphate are required for healthy tooth formation. Deficiencies can result in dose-related or exposure-related enamel hypoplasia.
Diseases that can cause hyperbilirubinemia and intrinsic tooth discoloration include sickle cell anemia; thalassemia; hemolytic disease of the newborn (HDN) due to either Rhesus factor, ABO, or other erythrocyte antigen incompatibility; biliary atresia [20] ; and other rare pediatric diseases. These diseases have the potential to cause hyperbilirubinemia and the subsequent dose-dependent incorporation of biliverdin (a by-product pigment of bilirubin) into developing teeth, producing a jaundicelike yellow-green tint on the tooth surfaces. [21]
Intrinsic tooth discoloration is reported in patients with blood dyscrasias such as sickle cell anemia, thalassemia, and HDN. These diseases have the potential to cause hemolysis and the subsequent dose-dependent incorporation of biliverdin (by-product pigment of bilirubin) into developing teeth, producing a jaundicelike yellow-green tint on the tooth surfaces. [21]
Genetic defects and hereditary diseases
Genetic defects in enamel or dentin formation include amelogenesis imperfecta (AI), dentinogenesis imperfecta (DI), and dentinal dysplasia (DD). These are hereditary diseases with a propensity for intrinsic tooth discoloration.
AI affects both primary and secondary dentitions and demonstrates numerous clinical manifestations that are classified into the following 4 types [22] :
-
Type 1 AI involves hypoplastic dentition. Hypoplastic teeth with rough or pitted enamel surfaces are at a greater risk for extrinsic staining. The teeth typically have an abnormally thin enamel layer that reveals the yellow color of dentin beneath the enamel. Note the image below.
-
Type 2 AI involves hypomaturation. Teeth with hypomaturation have soft enamel with a mottled opaque white, yellow, or brown discoloration. Note the image below.
-
Type 3 AI involves hypocalcification. The enamel in the hypocalcified type is yellow to orange, soft, and lost soon after eruption. Therefore, hypocalcified teeth develop dark stains and are at high risk for dental caries.
-
Type 4 AI involves hypomaturation or hypoplastic dentition with taurodontism.
DI occurs in 2 types. One type is associated with osteogenesis imperfecta, and the other type affects the teeth alone. The primary and secondary teeth are affected, and they have a brown or blue appearance with a distinctive translucent quality. The enamel chips off easily, and the teeth are prone to occlusal wear and caries.
DD occurs in 2 types. Teeth with type 2 DD have a blue, amber, or brown translucence. Teeth with type 1 DD have crowns with normal morphology and coloration.
Other hereditary diseases include erythropoietic (congenital) porphyria and epidermolysis bullosa (EB). Erythropoietic porphyria is a rare disease of porphyrin metabolism. The abnormally high levels of reddish brown or burgundy-red porphyrin pigments have an affinity for calcium phosphate and are incorporated into teeth during dental formation. The entire primary and secondary dentitions are pink, although case reports also describe the color as reddish brown or purple. [23] Teeth fluoresce red under ultraviolet light. Patients with EB may have enamel hypoplasia and pitting, which produce a yellowish tint. Patients are at risk for caries.
Etiology
The causes of extrinsic and intrinsic dental discoloration are as follows (see also Pathophysiology):
Extrinsic causes
-
Brown stain
Tobacco products
Dental plaque
Tea, coffee, wine, and other beverages
Certain foods
Metals
Iodine
Chlorhexidine rinse
Cetylpyridinium chloride rinse
Stannous fluoride
Khat leaf
Doxycycline
-
Black stain
Tobacco products
Betel nut
Dental plaque
Chromogenic bacteria
Tea, coffee, wine, and other beverages
Certain foods
Metals
-
Green stain
Chromogenic bacteria
Tea
Metals
-
Orange stain
Chromogenic bacteria
Metals
Doxycycline
Intrinsic causes - Localized color changes (in 1 or 2 adjacent teeth)
-
White (opaque) stain
Mild trauma to teeth during enamel formation (secondary teeth), eg, Turner tooth
Periapical infection of primary tooth
Traumatic injury to primary tooth or teeth
Incipient caries (primary or secondary teeth)
-
Yellow stain
Moderate trauma to teeth during enamel formation (secondary teeth), eg, Turner tooth
Periapical infection of primary tooth
Traumatic injury to primary tooth or teeth
Trauma without hemorrhage
Composites or glass ionomer or acrylic restoration
Caries (active)
Focal tooth abrasion
-
Brown stain
Severe trauma to teeth during enamel formation (secondary teeth), eg, Turner tooth
Periapical infection of primary tooth
Traumatic injury to primary tooth or teeth
Composite, glass ionomer, or acrylic restoration
Caries (active or remineralized)
Pulpal trauma with hemorrhage
-
Blue, gray, or black stain
Amalgam restoration
Glass ionomer or acrylic restoration
Metal crown margin associated with porcelain fused to metal crown
Pulpal trauma with hemorrhage
Intrinsic causes - Regional color changes
-
White (opaque) stain
Infection (maternal or childhood) during enamel formation
Trauma to multiple teeth during enamel formation
Mild fluorosis (short-term exposure)
Nutritional deficiency
-
Yellow stain
Infection (maternal or childhood) during enamel formation
Moderate fluorosis (short-term exposure)
Trauma to multiple teeth during enamel formation
Nutritional deficiency
Epidermolysis bullosa
Regional tooth abrasion or erosion
Diseases causing hyperbilirubinemia
-
Brown stain
Infection (maternal or childhood) during enamel formation
Severe fluorosis (short-term exposure)
Trauma to multiple teeth during enamel formation
-
Blue, gray, or black stain - Tetracycline therapy (short-term exposure)
-
Green stain - Diseases causing hyperbilirubinemia (eg, HDN, biliary atresia)
Intrinsic causes - Generalized changes (involving primary and/or permanent dentitions)
-
White (opaque) stain
Mild fluorosis
Amelogenesis imperfecta
-
Yellow stain
Moderate fluorosis
Amelogenesis imperfecta
Dentinogenesis imperfecta
Dentinal dysplasia
Epidermolysis bullosa
Diseases causing hyperbilirubinemia
Hemolytic diseases
Generalized tooth attrition, abrasion, or erosion
-
Brown stain
Porphyria
Tetracycline therapy (long-term exposure)
-
Blue, gray, or black stain
Tetracycline therapy (long-term exposure)
Minocycline therapy
-
Green stain - Diseases causing hyperbilirubinemia (eg, HDN, biliary atresia)
Epidemiology
United States data
An increase in the prevalence of mild-to-moderate fluorosis has been observed in the United States over the last decade, even in areas with nonfluoridated public water supplies. [16] The trend is explained by early overuse and ingestion of fluoridated toothpaste; the inappropriate use of fluoride supplements; and in fluoridated areas, the use of powdered infant formula mixed with local water.
International data
A study conducted in Australia found that 1 in 10 adults had dental fluorosis. The prevalence and severity of fluorosis were higher among persons born during the 1970s and 1980s than among those born after 1990, when measures were introduced to limit exposure to discretionary fluorides. [24]
Race-, sex-, and age-related demographics
No racial predilection exists for tooth discoloration.
The fluoride concentration of naturally fluoridated water varies depending on geographic location. For example, in some areas of Africa, the concentration may be as high as 10 parts per million (ppm), whereas many other regions have a concentration of 0 ppm. Artificially fluoridated water supplies usually have a fluoride concentration of 1 ppm. [17]
No sex predilection exists for tooth discoloration.
Teeth generally become more yellow and gray with increasing age. Depending on the etiology, persons of different ages are susceptible to various types of internally induced and externally induced tooth discolorations.
Prognosis
The prognosis is excellent if an etiology is identified and if the appropriate dental and medical care providers are involved in the comprehensive diagnosis and treatment of the condition.
Morbidity/mortality
If tooth discoloration is not treated, it can affect the appearance of a person's smile and craniofacial complex, causing temporary, as well as permanent, social and psychological sequelae.
Smiling is the end result of a complex neurologic, muscular, sensory, and psychological process. Because a smile is universally understood, an unattractive smile, due in part to discolored teeth, can have negative psychological, social, and clinical implications.
Complications
All irreversible dental treatments have the potential to cause complications.
Bleaching (eg, home bleaching) and restorative procedures are safe if performed by or under the supervision of a dentist with appropriate training and experience.
-
Vital bleaching causes short-term tooth sensitivity (1-4 d) in two thirds of patients (see Medical Care).
-
Patients with preexisting restorations, cervical erosions, enamel cracks, large pulp chambers, or sensitive teeth before treatment are at higher risk for postbleaching sensitivity.
-
The use of a mild bleaching agent, shortened application time and frequency, and topical fluoride therapy can reverse this sensitivity. [25]
-
Allergic reactions to bleaching agents are rare.
Restorative procedures, including bonding and the use of laminate veneers and fixed prostheses (eg, crowns and bridges), can result in pulpal or periodontal complications; however, careful treatment planning and therapy can minimize these complications.
Depending on the anatomic site, the proximity to vascular and neurologic vessels, and the oral and systemic condition of the host, oral surgical procedures infrequently can cause sequelae such as hemorrhage; pain; swelling; infection; and motor, nerve, or sensory deficits.
Patient Education
Educate patients about the necessity of daily oral hygiene and about the medications implicated in dental discoloration. Changes in dietary and toothbrushing habits and professional cleaning and treatment may help in preventing tooth discoloration (see Medical Care).
Educate patients who are treated for medical disorders associated with dental discoloration about the risks of tooth-related disorders.
Clinicians can also help in preventing fluorosis by teaching parents about fluoride use and good toothbrushing habits for children.
-
Transverse section of a central incisor illustrates the different soft and hard tissue layers of the tooth and the supporting dental-alveolar apparatus.
-
Dental calculus accumulations on the mandibular anterior teeth.
-
Stained supragingival plaque and calculus deposits.
-
Severe tobacco staining.
-
Image demonstrates a red extrinsic stain at the gingival margins and interproximal and incisal regions of the teeth in a patient with a habit of chewing pan (a combination of betel nut of the areca palm, betel leaf, and lime).
-
Extrinsic dental staining caused by long-term topical use of 0.12% chlorhexidine mouthrinse.
-
Image demonstrates dental attrition in a 75-year-old patient due to loss of occlusal enamel structure that reveals the underlying dentin.
-
Severe dental abrasion and gingival recession due to long-term traumatic toothbrushing habit.
-
Root surface caries, severe periodontitis, and amalgam restorations.
-
Extensive dental caries.
-
Severe root surface and occlusal caries that necessitated tooth extraction.
-
Severe enamel hypoplasia (ie, Turner tooth) on a secondary (permanent) maxillary central incisor. The patient had an intrusion injury of the primary central incisor during childhood that interrupted the development of the secondary central incisor.
-
Intrinsic dental discoloration caused by blunt trauma to the mandibular incisors that led to pulpal necrosis.
-
Dental radiograph demonstrates external resorption and periapical bone loss in a patient with intrinsic dental discoloration caused by blunt trauma to the mandibular incisors that led to pulpal necrosis. Image was obtained in the same patient as in Image 15.
-
Enamel hypoplasia of the incisal half of the maxillary and mandibular secondary incisors caused by rubella infection when the patient was aged 4 months.
-
Tetracycline staining of mandibular teeth caused by the ingestion of tetracycline when the patient was aged 3 years.
-
Mild dental fluorosis causing mottled white intrinsic discoloration of the teeth.
-
Severe fluorosis of the teeth.
-
Amelogenesis imperfecta (hypoplastic type 1 form) and associated enamel pitting and extrinsic dental discoloration.
-
Amelogenesis imperfecta (hypomaturation type 2 form).
-
Porcelain laminate veneers for the treatment of tetracycline staining.

















