Background
Cholesterol embolism, or atheroembolism, is a condition that has historically been a diagnostic challenge owing to its nonspecific symptoms and because it often mimics other more common conditions and diseases. Autopsy studies have revealed that up to 15-20% of individuals older than 60 years with a history of atherosclerosis had cholesterol emboli present, which suggests that cholesterol embolism may be more frequently undiagnosed than originally believed. [1] Cholesterol embolism is categorized as a disorder of occlusion due to emboli, wherein there is luminal obstruction of small- and medium-caliber arteries (100-200 μm in diameter) by cholesterol crystals (see the image below) that form from fragmentation of ulcerated atheromatous plaques inside vasculature. Although it was initially reported by Panum over a century ago, the diagnosis of cholesterol embolism is often missed or overlooked, resulting in potentially devastating and even fatal consequences. In 1987, Fine et al. described certain hallmark skin findings in patients with cholesterol embolism, thereby linking cholesterol embolism to recognizable signs and symptoms that could be identified clinically. [2] In 1999, Belenfant et al reported new treatment regimens for the management of cholesterol embolism, allowing for breakthrough advances in patients with this disease. [3] Despite these medical developments, cholesterol embolism remains a challenging entity to accurately diagnose and effectively treat. Numerous comorbid conditions can be associated with the development of cholesterol embolism, including hypertension, hyperlipidemia, diabetes mellitus, peripheral vascular disease, and tobacco use. [4]
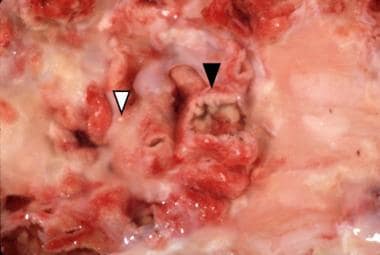 Aorta with an ulcerated plaque (black arrowhead) on the luminal side photographed under water to enhance reflection of cholesterol crystals (white arrowhead).
Aorta with an ulcerated plaque (black arrowhead) on the luminal side photographed under water to enhance reflection of cholesterol crystals (white arrowhead).
A high index of suspicion is imperative because the signs and symptoms of cholesterol embolism are often atypical, unrecognized, not temporally correlated with the onset of physical findings, and/or simply overlooked. Unfortunately, there is no laboratory testing that is specific for cholesterol embolism, although serologic markers checking for eosinophilia and inflammation may be helpful. [5] Additionally, diagnosis is suggested by progressive increases in blood urea nitrogen and creatinine levels following an invasive arterial procedure. On physical examination, the presence of netlike or lacelike, bluish to deep-purple patches with a mottled appearance involving the distal extremities and blue fingers or toes can be invaluable clinical features in diagnosing cholesterol embolism (see the image below). On pathology, cholesterol embolism can be identified by characteristic needle-shaped cholesterol clefts and intravascular microthrombi; however, one or both of these findings may be absent and do not necessarily correlate directly with a patient's clinical disease.
 Symmetric involvement of the feet with livedo reticularis on the plantar surface of the forefoot and cyanosis of the left fifth toe. The painful cyanotic toe is typical of blue toe syndrome.
Symmetric involvement of the feet with livedo reticularis on the plantar surface of the forefoot and cyanosis of the left fifth toe. The painful cyanotic toe is typical of blue toe syndrome.
Pathophysiology
Rupture and subsequent fragmentation of ulcerated atherosclerotic plaques inside of vessels leads to the formation of cholesterol emboli, which can then result in intraluminal obstruction of vessels. Thus, patients with cholesterol embolism usually have some degree of atherosclerosis. Fracturing of unstable atheromatous plaques can occur spontaneously, albeit rarely. Reports describe spontaneous cholesterol embolism in patients with likely unstable atheromatous plaques. [6, 7, 8] More commonly, cholesterol emboli typically occur in several clinical settings that serve as triggering events for the embolization process. These settings include vascular intervention procedures (eg, arterial catheterization), long-term use of anticoagulants (including warfarin), [9] and administration of acute thrombolytic therapy (as in the treatment of myocardial infarctions or cerebrovascular attacks). [10]
Regardless of the particular etiology, the rupture of atheromatous plaques inside of arteries releases a shower of fragmented cholesterol crystals into the bloodstream. These crystals then migrate distally until they lodge in smaller arterioles, where they provoke an acute inflammatory response. This response triggers a cascade of multiple events culminating in intravascular thrombus formation, endothelial proliferation, and vessel fibrosis. Microvascular ischemia leads to tissue loss, organ dysfunction, and, in some cases, catastrophic organ collapse such as renal failure. [5, 11]
The presenting clinical syndrome that a patient manifests depends on the location of the source of embolism as well as the pattern and distribution of vascular flow downstream. The most common sites of involvement for severe atheromatous disease are the abdominal aorta and the iliac and femoral arteries. Accordingly, the signs and symptoms of cholesterol embolism more commonly result from embolism to the lower half of the body, such as the lower legs, feet, and toes. In fact, 80% of cases are associated with disruption and fragmentation of aortoiliac atheromatous plaques. When the primary source of cholesterol crystals is inside of the aortic arch, the signs and symptoms of embolization may present in the eyes and the CNS. [12] Clinical manifestations may be detected immediately after the inciting event or may only present after a period of time has passed (anywhere from hours to weeks). A 1999 study by Belenfant et al of a group of patients diagnosed with cholesterol embolism found that the precipitating event occurred an average of 2 months prior to recognition of fulminant clinical disease. [3]
Etiology
Cholesterol embolism may occur spontaneously in patients with a history of atherosclerosis; however, a triggering event much more commonly results in full clinical manifestation of cholesterol embolism syndrome. There are various precipitating factors that can contribute to the development of cholesterol embolism and these are described below. [10]
Long-term use of anticoagulation and acute thrombolytic therapy
A history of antecedent therapy with anticoagulant agents, including warfarin, is present in approximately 30-35% of patients with cholesterol embolism. [13, 14, 15] These therapies are thought to predispose an individual to the development of cholesterol embolism by two distinct mechanisms. First, use of anticoagulants and thrombolytics progressively lyses a blood clot, thereby stripping away the protective layer of fibrin isolating subintimal deposits of cholesterol. Removal of this shieldlike coating exposes the friable cholesterol plaque to shearing forces of arterial blood flow, resulting in fragmentation. Second, hemorrhage of blood into a cholesterol plaque after therapy is administered can undermine the overall stability and integrity of the plaque and can lead to lysis of the fibrin cap. This causes cholesterol crystals to become dislodged and enter the circulation, where they can cause downstream intraluminal obstruction. [16]
Interventional vascular techniques
Various surgical or radiologic vascular procedures are reported to precede cholesterol embolism in nearly 65% of patients. [17] The introduction of a foreign object such as an arterial catheter or stent into a blood vessel may cause intimal trauma, exposing the underlying cholesterol-rich matrix to the arterial circulation. This risk is proportionally increased with increased sheath size of the catheter. With novel intravascular techniques becoming more common in medical practice, the risk of disease may be increasing. An Italian study of 354 patients demonstrated that the most common precipitating factor among that group of individuals was coronary angiography via the femoral artery. Cholesterol embolism has also been reported after peripheral stenting procedures for arterial claudication. [18] Additional predisposing risk factors for the development of cholesterol embolism after cardiac catheterization include older age, male sex, hypertension, a history of smoking, and elevated preprocedural C-reactive protein levels. [19] Although most reports of cholesterol embolism are noted to occur with endovascular procedures involving the large vessels, it is important for the clinician to be aware that this complication may occur after manipulation of any vascular bed.
Trauma
External trauma or injury may also predispose an individual with a history of atherosclerosis to the development of cholesterol embolism. This can include cardiopulmonary resuscitation or sudden deceleration injury as may occur in motor vehicle accidents. The forces generated by the traumatic event may cause an unstable ulcerated atheromatous plaque to become dislodged and fragment into numerous pieces, releasing cholesterol clefts into the vasculature.
Epidemiology
Frequency
The true incidence of cholesterol embolism is unknown because it is likely underdiagnosed and/or underrecognized. Reported estimates vary widely among populations. Reasonable estimation of cholesterol embolism incidence is complicated by the discrepancy between histologic and clinical disease. Published estimates in the medical literature approximate an average incidence of 2-4%, with reports ranging widely. One of the largest epidemiological studies performed was by Moolenaar and Lamers, using the Dutch National Pathology Information System. [20] They estimated an incidence of 6.2 cases per million per year in the general population living in the Netherlands, and a prevalence of 0.31% in all performed autopsies. However, these results are not necessarily generalizable to other populations given the supposed low prevalence of both atherosclerosis and invasive vascular procedures in the Dutch population.
Race
Cholesterol embolism is much more commonly described in White populations than in other racial groups. This observation may be related to ascertainment bias and the failure to detect the subtle cutaneous findings in individuals with darkly pigmented skin. Additionally, evidence suggests that access to health care, including invasive vascular procedures (which can serve as inciting events), may be more limited in certain populations as in lower socioeconomic areas for example, and this may contribute to the sizeable epidemiological difference.
Sex
Cholesterol embolism occurs more often in males than in females, with an approximate male-to-female ratio of about 3.4:1. This could reflect the excess risk of cardiovascular disease due to atherosclerosis conferred by the male sex.
Age
The reported age range for cholesterol embolism is 26-90 years, and the mean age of patients who develop cholesterol embolism is 66-72 years.
Prognosis
Despite medical advances in both the diagnosis and treatment of cholesterol embolism, the overall prognosis remains poor. Cholesterol embolism is considered a marker for severe atherosclerosis and the associated morbidity and mortality reflect the gravity of the diagnosis of cholesterol embolism. Mortality rates are reported to be as high as 60-87% within 1 year of cholesterol embolism diagnosis in some studies, which are worse than the reported mortality rates associated with acute myocardial infarction. [19] Death from cholesterol embolism may occur via ruptured aortic aneurysm, CNS infarction, myocardial or gastrointestinal infarction, sepsis, cerebrovascular disease, critical limb ischemia, cachexia, and renal failure. [21]
Preexisting renal disease is a known marker for higher mortality in the setting of cholesterol embolism. [22] Furthermore, longstanding and poorly controlled hypertension is a recognized risk factor for the development of end-stage renal disease in these patients (P< .001). [23] Patients with visceral involvement (many of whom also present with skin findings) are reported to have mortality rates of 50% and 65% within 6 and 12 months, respectively. The presence of cutaneous manifestations does not appear to predict survival because the features may occur in patients with minor-to-severe disease. However, patients with peripheral manifestations alone have a 38% mortality rate within 15 months. Those who survive may be left with chronic renal insufficiency requiring hemodialysis, [22] stroke resulting in paraplegia, unstable angina, amputation of the affected extremity (5-15% of patients), and malnutrition or significant weight loss (70% of patients). [21]
Patient Education
For patient education resources, visit the Cholesterol Center. Also, see the patient education articles High Cholesterol, and Cholesterol FAQs.
-
A 76-year-old man with a history of aortobifemoral bypass graft developed this eruption after an angiographic procedure. This image shows the plantar surface of the right foot with some of the discoloration resulting from petechiae arranged in a reticulated pattern. This is not livedo reticularis. Petechiae do not blanch on diascopy, but the lesions of livedo reticularis do blanch.
-
Aorta with an ulcerated plaque (black arrowhead) on the luminal side photographed under water to enhance reflection of cholesterol crystals (white arrowhead).
-
Low-power view of a skin biopsy specimen demonstrating an arteriole within the subcutaneous fat occluded with thrombus material that contains (black arrowhead) needle-shaped cholesterol clefts (hematoxylin and eosin stain, original magnification X40).
-
High-power view of occluded vessel (hematoxylin and eosin stain, original magnification X100).
-
Symmetric involvement of the feet with livedo reticularis on the plantar surface of the forefoot and cyanosis of the left fifth toe. The painful cyanotic toe is typical of blue toe syndrome.
-
Dorsal surface of the toes of the right foot of a patient with discoloration resulting from petechiae. This image shows cyanosis of the fourth toe. The dominant eruption is petechial. Note the pallor of the tip of the great toe and the second toe. This finding indicates acute loss of perfusion.
-
Plantar surface of the right foot. The distal half of the great toe is gangrenous, with a sharp demarcation between the necrotic tissue and the normal proximal skin. Livedo reticularis is present on the distal plantar forefoot, and petechiae are present on the distal pad of the second and fourth toes.
-
The lower extremities show well-developed livedo reticularis and focal areas of erosion and ulceration.
-
Photomicrographs of histologic sections of an aorta with van Gieson stain. (Left) An atherosclerotic plaque with the fibrous cap (black arrowhead) overlying a necrotic core of cellular debris, extracellular lipids, and cholesterol clefts (white arrowhead). Underneath the plaque is the elastic media (arrow). (Right) A ruptured atherosclerotic plaque exposing the atheromatous debris containing cholesterol crystals to the bloodstream on the luminal side of the aorta.
-
CT scan of an infrarenal abdominal aortic aneurysm showing the mural thrombosis (white arrowhead) and the bright atherosclerotic calcifications (black arrowhead).






