Practice Essentials
Commonly known as a skin tag, an acrochordon is a small, soft, common, benign, usually pedunculated neoplasm that is found particularly in persons who are obese. It is usually skin-colored or hyperpigmented, and it may appear as surface nodules or papillomas on healthy skin. Most acrochordons vary in size from 2-5 mm in diameter, although larger acrochordons up to 5 cm in diameter are sometimes evident. The most frequent localizations are the neck and the axillae, but any skin fold, including the groin, may be affected.
Birt-Hogg-Dube (BHD) syndrome is a rare autosomal dominant genodermatosis characterized by skin tumors, including multiple fibrofolliculomas, trichodiscomas, and acrochordons. [1] These patients tend to develop renal and colonic carcinomas. [2] The defective gene in BHD syndrome has been identified and is suspected of being a tumor suppressor gene. Several mutations of the BHD gene have been reported. [3, 4] All skin lesions in the syndrome may actually represent fibrofolliculomas cut in various planes of section.
Interestingly, skin tags have been used for reconstruction of the ear and of the nose, particularly for distal nasal reconstruction. [5]
Related Medscape articles of possible interest include Premalignant Fibroepithelial Tumor (Pinkus Tumor), Benign Vulvar Lesions, and Skin, Benign Skin Lesions.
Patient education
Advise patients that these are benign tumors.
Signs and symptoms
Also see History.
Skin tags may occur singly or multiply, and they are most often found in intertriginous areas (eg, axillae, neck, eyelids) (see the image below). They are also commonly located on the trunk, the groin, the abdomen, and the back.
FEPs of the oral mucosa, anus, and vulvovaginal areas may be found. These lesions may be flesh-colored or hyperpigmented. Pedunculated lesions may become twisted, infarcted, and fall off spontaneously.
Three types of acrochordons are described, as follows:
-
Small, furrowed papules of approximately 1-2 mm in width and height, located mostly on the neck and the axillae
-
Single or multiple filiform lesions of approximately 2 mm in width and 5 mm in length occurring elsewhere on the body
-
Large, pedunculated tumor or nevoid, baglike, soft fibromas that occur on the lower part of the trunk
Giant acrochordons garner considerable attention, producing considerable discomfort for patients when located in the axillae and genital regions. [6, 7, 8]
Other disorders may appear within an acrochordon. An acrochordon with histological features of lichen sclerosis was observed. [9]
Diagnostics
Also see Imaging Studies.
Acrochordons are characterized by acanthotic, flattened, or frondlike epithelium. A papillarylike dermis is composed of loosely arranged collagen fibers and dilated capillaries and lymphatic vessels (see the images below). Appendages are generally absent. Acrochordons were thought to be marked by decreased numbers of elastic fibers, though 1 study of elastic tissue in fibroepithelial polyps (FEPs) showed no deficiency of this tissue.
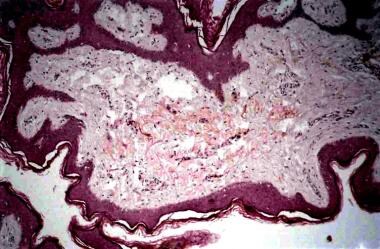 A hyperplastic epidermis showing papillomatosis, hyperkeratosis, and acanthosis overlying loosely arranged collagen fibers and many capillaries.
A hyperplastic epidermis showing papillomatosis, hyperkeratosis, and acanthosis overlying loosely arranged collagen fibers and many capillaries.
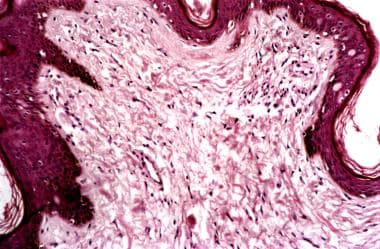 A higher-power view demonstrating to better advantage loosely arranged collagen fibers and many capillaries.
A higher-power view demonstrating to better advantage loosely arranged collagen fibers and many capillaries.
Acrochordons (skin tags) are often considered clinically insignificant cutaneous redundancies that should be removed without histopathologic analysis. [10] However, one may rarely find another neoplasm within an acrochordon. A squamous cell carcinoma that had features resembling a keratoacanthoma was described. [11]
Management
See Treatment for a full discussion.
Skin tags are generally treated for noncosmetic reasons. Failure to clearly delineate how the skin tag is producing a problem for the patient when removing a symptomatic acrochordon may be a cause for concern. This documentation may be obligatory for insurance coverage because most plans do not cover cosmetic procedures. Additionally, inform the patient that the insurance company may not cover the procedure if the physician believes that he or she is performing the removal for cosmetic reasons.
Pathophysiology
Skin tags are cutaneous manifestations of obesity. [12]
Previous theories have suggested that a localized paucity of elastic tissue may result in sessile or atrophic lesions. It is also thought that pendulous variations may be caused by losses of large confluent areas of elastin; however, a 1999 study of elastic tissue in fibroepithelial polyps (FEPs) showed no significant abnormalities. [13]
A cross-sectional study of adult patients at a university teaching hospital, including 98 patients and 103 controls, found that the presence of multiple skin tags was strongly associated with insulin resistance, irrespective of other risk factors. [14]
In another survey, 113 patients with skin tags and 31 healthy subjects were evaluated. This work linked obesity, dyslipidemia, hypertension, insulin resistance, and elevated high-sensitive C-reactive protein with skin tags, suggesting they may serve as a marker of increased risk of atherosclerosis and cardiovascular disease. [15]
Etiology
Frequent irritation seems to be an important causative factor, especially in persons who are obese. An opinion also exists that acrochordons are simply the effect of skin aging, with many factors responsible for their development. Hormone imbalances may facilitate the development of acrochordons (eg, high levels of estrogen and progesterone during pregnancy, high levels of growth hormone in acromegaly). Epidermal growth factor (EGF) and alpha tissue growth factor (TGF) have also been implicated in the development of tumors such as these. Whether any infective factors initiate acrochordon growth is still not clear.
Human papillomavirus (HPV) types 6/11 DNA were found in a high percentage of skin tag biopsy samples obtained from 49 white patients. According to the authors of the study, viral infection should be considered as a pathogenic cofactor. [16]
Acrochordons associated with fibrofolliculomas and trichodiscomas have been described as components of BHD syndrome, an autosomal dominant disorder. They have been reported to accompany other neoplasms, especially tumors of the gastrointestinal tract and kidneys. Neoplasms are suggested to produce and release growth factors that cause acrochordon growth into the circulation. The results of a recent study refute the theory that an association of acrochordons and colonic polyps actually exists.
An association with type 2 diabetes mellitus has been observed. [17, 18, 19] A study of 118 research subjects with acrochordon reported an incidence of 40.6% of either overt type 2 diabetes mellitus or impaired glucose tolerance. Reports exist suggesting that the mechanism is through the effect of insulin and glucose starvation. [20] The previous study showed no correlation between the location, size, color, or number of acrochordons with impairment of glucose tolerance. However, they may suggest early metabolic syndrome. [21] A possible role for insulinlike growth factor in the etiology of acrochordons was suggested in a study of 30 nondiabetic persons and 30 controls. [22]
Epidemiology
Acrochordons have been reported to have an incidence of 46% in the general population.
An equal prevalence of acrochordons exists in males and females.
When present, acrochordons increase in frequency up through the fifth decade. As many as 59% of persons may have acrochordons by the time they are aged 70 years.
Prognosis
Acrochordons are benign tumors. On rare occasions, histologic examination of a clinically diagnosed FEP reveals a basal or squamous cell carcinoma. In 1 study, 5 of 1335 clinically diagnosed FEP specimens were malignant. Four were basal cell carcinomas, and 1 was a squamous cell carcinoma in situ. None of these specimens was submitted by a dermatologist. This study concluded that clinically diagnosed FEPs have a low probability of having malignant characteristics on histologic examination.
-
A 53-year-old man with multiple, small, axillary skin tags.
-
A hyperplastic epidermis showing papillomatosis, hyperkeratosis, and acanthosis overlying loosely arranged collagen fibers and many capillaries.
-
A higher-power view demonstrating to better advantage loosely arranged collagen fibers and many capillaries.









