Background
Bloom syndrome (congenital telangiectatic erythema) is a rare autosomal recessive disorder. It was first described in 1954 by David Bloom in a series of patients with telangiectatic erythema on the face and dwarfism. [1] Bloom syndrome has three cardinal features: sun sensitivity, telangiectatic erythema of the face, and stunted growth.
Owing to the genomic instability present in this disease, patients with Bloom syndrome show a much higher incidence of malignant neoplasms, which is the major cause of death in such patients. No patients have been reported to reach age 50 years.
Variable degrees of immunodeficiency are present in these patients, predisposing them to various infections; this acts as an additional factor for the high incidence of cancers in Bloom syndrome patients.
Pathophysiology
Bloom syndrome (congenital telangiectatic erythema) is caused by a mutation in both alleles of the gene designated BLM, traced to band 15q26.1. [2, 3, 4, 5] (see the image below). BLM encodes 1417 amino acids that code for a protein in the nuclear matrix of growing cells, which is a member of the RecQ family of helicases. This protein plays a pivotal role in DNA recombination and repair. BML mutations thus result in defects in DNA repair and genomic instability in the somatic cells, predisposing the patients to cancer development. [6]
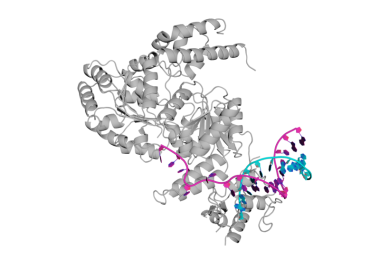 Crystal structure of the Bloom syndrome helicase BLM in complex with DNA (PDB ID: 4CGZ). Courtesy of Arthur Zalevsky (own work), via Wikimedia Commons.
Crystal structure of the Bloom syndrome helicase BLM in complex with DNA (PDB ID: 4CGZ). Courtesy of Arthur Zalevsky (own work), via Wikimedia Commons.
The BLM mutations can be found in compound heterozygous forms, homozygous forms, or as single gene mutation forms.
There is a 10-fold increase in the sister chromatid exchanges, [7] in addition to the presence of chromatid gaps, breaks, and gross structural rearrangements. [7, 8] Sister chromatid exchanges are considered a sensitive indicator for cell genome instability, as they are thought to be the outcome of DNA double-strand breaks resulting from homologous recombination repair. [9]
Over 60 mutations of the BLM gene have been found in Bloom syndrome. The most common mutation is the deletion of 6 nucleotides at position 2281 and their replacement with 7 others, which occurs most commonly in Ashkenazi Jews. [10]
In 1989, Nicotera et al suggested that the major biochemical defect in persons with Bloom syndrome is chronic overproduction of the superoxide radical anion. They thought that inefficient removal of peroxide might be responsible for the high rates of sister chromatid exchange and chromosomal damage in Bloom syndrome cells. [11]
MM1 and MM2 are proteins identified in Bloom syndrome and Fanconi anemia, creating a link between them. The gene encoding these proteins is FANCM. Both diseases show phenotypical similarity and both demonstrate bone marrow failure, skeletal growth deficiency, short stature, and predisposition to hematological malignancies, although they are genetically unrelated. Both diseases involve the BRAFT and FANCM complexes, which are important in DNA repair. [12, 13]
Bugreev et al suggest that a function of BLM is stimulation of RAD51 DNA pairing; results from their study show the importance of the RAD51 nucleoprotein filament conformation for stimulating DNA pairing by BLM. [14]
Photosensitivity in Bloom syndrome patients is a result of increased susceptibility to 313-nm light, approaching the ultraviolet (UV)–A range. The minimal erythema dose threshold for both UV-A and UV-B are reduced. [15] Cellular sensitivity in Bloom syndrome patients is in the form of phototoxicity and not photocarcinogenicity, as is seen in xeroderma pigmentosa. [16] Bloom syndrome patients exhibit a greater vulnerability of their DNA to UV radiation than DNA of healthy populations.
Bloom syndrome patients also demonstrate impairment in lymphocytic proliferation, deficient immunoglobulin synthesis, and lowered response to mitogen stimulation, resulting in impairment of both cellular and humoral immune responses. [17]
The overall result of the genomic instability in the proliferating cells is a high risk of malignancy, reduced fertility or infertility, B- and T-cell immunodeficiencies, and cutaneous manifestations, including photosensitivity, poikiloderma, and telangiectatic erythema.
Etiology
Bloom syndrome (congenital telangiectatic erythema) is genetic with an autosomal recessive pattern of inheritance. The gene locus is band 15q26.1.
Cytogenetic findings in a Bloom syndrome patient with acute myeloid leukemia of the French-American-British subtype M1 showed preferential occurrence of total or partial loss of chromosome 7.
Mutation of the DNA ligase I gene may account for the primary metabolic defect in Bloom syndrome, not due to a reduction in the number of protein molecules or to inhibitory substances, but rather to the ATP-binding and hydrolytic activity of the enzyme. DNA ligase I and DNA polymerase alpha are enzymes that function during DNA replication; DNA ligase II and DNA polymerase-beta function during DNA repair. [18]
Epidemiology
Frequency
United States
More than 170 case reports of Bloom syndrome (congenital telangiectatic erythema) have been made. The frequency of parental consanguinity is much greater than in the general population.
International
Bloom syndrome (congenital telangiectatic erythema) is more common in Ashkenazi Jews, with an estimated carrier frequency of 1:120 and a reported prevalence of approximately 1 in 48,000 persons, accounting for 25% of the patients in the Bloom syndrome patient registry. [19]
The Bloom Syndrome Registry (BSR) was established in 2009. The total number of patients is less than 300. Of the registered patients, 75.2% were non-Jews. [20] However, it has been reported in Japan and other countries, with increased risk in cases with parental consanguinity.
Race
Bloom syndrome (congenital telangiectatic erythema) is more common in eastern European Ashkenazi Jews.
Sex
The male-to-female ratio for Bloom syndrome (congenital telangiectatic erythema) is 1.3:1.
Age
Bloom syndrome (congenital telangiectatic erythema) occurs in the first few months of life.
Prognosis
Increased risk of premature death in the second or third decade occurs secondary to malignancies. Patients with Bloom syndrome (congenital telangiectatic erythema) are estimated to develop malignancy at a rate 150-300 times higher than the general population. Twenty percent of Bloom syndrome patients develop malignancy during their life time. [21] Various types of leukemia develop at a mean age of 22 years. Patients who survive beyond age 22 years develop solid tumors at an average age of 35 years. Fortunately, these tumors are sensitive to chemotherapy and radiotherapy.
Early diagnosis of leukemia is, at present, not known to improve the chances of curative therapy. Frequent hematologic examinations in children are not advised for fear of untoward psychologic effects. Allogeneic marrow grafting has not been performed in Bloom syndrome patients. Men with Bloom syndrome are sterile; women have reduced fertility and a shortened reproductive span. Bloom syndrome patients who become pregnant are at high risk for premature delivery. Intelligence is usually normal, although mild deficiency has occurred in a few affected persons. Diabetes occurs in approximately 10% of individuals with Bloom syndrome.
Resistance to infections gradually improves with age, as do erythema and photosensitivity.
Patient Education
Bloom Syndrome Registry
Laboratory of Human Genetics
New York Blood Center
310 East 67th Street
New York, NY 10021
(212) 570-3075; Fax (212) 570-3195
Contact person: James L German III, MD
-
Crystal structure of the Bloom syndrome helicase BLM in complex with DNA (PDB ID: 4CGZ). Courtesy of Arthur Zalevsky (own work), via Wikimedia Commons.





