Overview
Tumescent liposuction involves the use of tumescent anesthetic and microcannulae. The small cannulae form tunnels in the subcutaneous tissue and allow for more effective and less traumatic fat removal than the large cannulae.
Liposuction is the most commonly performed cosmetic procedure in the United States. It is also referred to as liposculpture, lipoplasty, and suction-assisted lipectomy. The ideal candidate is physically fit and eats well-balanced meals but is unable to reduce a fatty deposit that is well localized and often seems to involve a genetic susceptibility.
In the past, the surgery required blood transfusions because blood loss in the aspirate was significant. Dr Jeffrey Klein, a dermatologic surgeon, is credited as the originator of the tumescent technique, which has allowed liposuction to be performed with the patient under local anesthesia while minimizing blood loss and the risks of general anesthesia. Since its inception, liposuction performed with the tumescent technique has had an excellent safety profile. [1]
History
In 1921, Dujarrier, a French surgeon, curetted a ballerina's knees to create a better shape, but the patient developed gangrene and required an amputation. In 1964, Schrudde developed curettage and suction. Georgio and Arpad Fischer, Italian surgeons, developed cannulae and an internally rotating planatome and cellusuctiontome. Other cannulae were developed by Kesselring and Meyer and Illouz, the latter also developed the wet technique. Fournier favored the syringe technique and instructed physicians to use the cross-tunneling technique. The dry technique uses general anesthesia without any preoperative infiltration of vasoconstrictive solution. The wet technique achieves a moderate reduction in blood loss by using a small amount of epinephrine.
Dermatologic surgeons began performing liposuction since its evolution, and the number of dermatologists performing liposuction increased as studies showed the safety provided by the tumescent technique and the physiologic basis for the benefit of the procedure. As the number of cases performed increased, surveys of physicians corroborated its safe track record.
Future directions
Future uses of liposuction may involve the harvesting of stem cells for facial revolumization, as well as other uses for stem cells, such as in the treatment of urinary incontinence and hair regrowth. [2]
Advantages
The several advantages of the tumescent approach include the following:
-
Less blood is lost.
-
Intravenous fluid replacement is not necessary.
-
Bacteriostatic lidocaine may decrease the risk of infections.
-
Tumescence magnifies defects; therefore, the likelihood of needing a secondary procedure may be less.
-
Lipid-soluble lidocaine is somewhat suctioned out with the aspirated fat.
-
Vasoconstriction minimizes absorption.
-
The epinephrine may increase the cardiac output, which, in turn, hastens the hepatic metabolism of the lidocaine.
-
The duration of anesthetic effect may last as long as 24 hours.
-
The lidocaine may be given safely up to 45 mg/kg and even higher in certain conditions.
A small study by Lipp et al, surveying and following up on 32 patients, indicated that tumescent liposuction produces safe, long-lasting results. At follow-up (mean overall follow-up 8.9 years; neck follow-up 9.9 years), a surgeon evaluator observed significant differences in neck volume (2.42 vs 0.71) and in skin laxity scales (1.17 vs 0.83 for laxity and 1.31 vs 0.83 for firmness). A blinded evaluator also determined differences on the laxity scales (1.14 vs 0.77 for laxity and 1.33 vs 0.75 for firmness). The investigators found that 85.7% of patients surveyed “would recommend liposuction to their friends and family members.” [3]
Alternatives
Cryolipolysis [4] (Zeltiq, California) involves freezing the fat at a temperature that is above the freezing point of skin. A 1-hour cycle of freezing can reduce, at 4 months, the volume of fat by 20%. Secondary treatments can be performed 1-4 months after the first treatment. Multiple applicators overlapping the fat bulge have been shown to produce some very good results, at times similar to liposuction but without any surgery.
External laser, ultrasound, and radiofrequency technologies have been cleared by the US Food and Drug Administration (FDA) for noninvasive fat reduction. [5]
Indications
Liposuction is generally performed for the reduction of fatty deposits that are well localized and often seem to involve a genetic susceptibility.
Other situations exist that may benefit from tumescent liposuction. These include lipoma removal, [6, 7] Madelung disease, axillary hyperhidrosis, [7] axillary bromhidrosis, [8] evacuation of hematomas, pseudogynecomastia, [7, 9] and the controversial staged liposuction for persons who are morbidly obese.
Contraindications
Contraindications are as follows:
-
Unrealistic patient expectations
-
Poor physical health of patient
-
Patient who underwent crash dieting immediately prior to consultation
-
Morbid obesity (megaliposuction controversial due to higher risk of mortality from fluid shifts)
Anesthesia
Klein [10, 11, 12, 13] noted that the correct maximum safe dose of lidocaine was at one time not investigated but rather extrapolated from procaine. However, research by Klein and Jeske has estimated preliminarily that for tumescent lidocaine, the maximum safe dosage without liposuction is 28 mg/kg and with liposuction is 45 mg/kg. According to the investigators, delayed systemic absorption of the lidocaine resulted in serum concentrations of the anesthetic that, over a 24-hour study period, were lower than those related to mild toxicity, being under 6 mcg/mL. [14]
Many of Klein's observations have been the opposite of what was intuitive. He reported that the peak serum lidocaine levels occurred at different times when infiltrating the subcutaneous tissue compared with the skin. Klein realized that lowering the concentration of the anesthetic provided a longer duration of action, with a lower concentration of epinephrine allowing for better vasoconstriction. The main elimination route of the anesthetic was not the liposuction; rather, it was resorbed and excreted. Drainage through open insertion sites also lessens the systemic absorption but by a minimal amount. Tumescent liposuction, as defined by Klein, includes using tumescent anesthetic and microcannulae. The small cannulae form tunnels in the subcutaneous tissue and allow for more effective and less traumatic fat removal than the large cannulae. Klein also found that his patients had less pain using the small cannulae.
A literature review by Bajwa et al indicated that in tumescent liposuction, the normal waiting time for stable analgesic and vasoconstrictive effects from local infiltration of lidocaine with epinephrine is between 10 and 60 minutes. In this way, hypoperfusion and hydrodissection are improved, allowing easier suction. [15]
Because lidocaine is metabolized by the hepatic cytochrome P-450 enzyme, concurrent medications that are similarly metabolized must be noted, otherwise lidocaine toxicity might result. Cimetidine (Tagamet), beta blockers, anxiolytics, and many other drugs are among this list. Because diazepam may interfere with lidocaine levels, Klein considers it not to be a prudent addition to the medications given before or during surgery. Furthermore, this medication may eliminate seizures as a warning of lidocaine toxicity, and cardiac dysrhythmias may be the surgeon's first sign of toxicity. However, some dermatologic surgeons have reported on the safe use of conscious sedation with tumescent liposuction.
Because the postoperative analgesia of tumescent anesthetic has an 18-hour duration, bupivacaine is not needed, and, in fact, it creates an added risk of cardiotoxicity. (However, a survey by the American Society of Plastic Surgeons of 320 plastic surgeons found that 22 of them [7%] reported using bupivacaine in tumescent liposuction, employing a dosage of 62.5-150 mg. No toxicity cases related to the anesthetic were reported. [16] )
Much less bleeding occurs as a result of tumescent liposuction than of liposuction performed with the wet technique. The blood-tinged infranatant of the aspirate obtained in tumescent liposuction has a hematocrit of less than 1%. Less than 12 mL of whole blood is lost per liter of fat extracted. [17]
A study by Wang et al indicated that in terms of lidocaine use in liposuction, tumescent anesthesia is better than local anesthesia for the preservation of adipose-derived stem cells (ASCs), with the local anesthesia causing significantly more ASC apoptosis than occurred in the tumescent procedure. [18]
Technique
Patient evaluation
The patient must have realistic expectations. The ideal candidate is only 10-20 lb overweight. Patients should realize that, although the cellulite's appearance may improve, it is not expected to lessen. The patient should be in good physical health. A healthy well-balanced diet is important in maintaining the postoperative results as well as in ensuring excellent healing during the convalescence. Crash diets immediately prior to the consultation to be considered a candidate for surgery may increase the risk of complications as a consequence of electrolyte imbalances or nutritional deficiencies. The physician should be confident that patients' motives are well founded and that the discontent with their physique is not a displaced unhappiness with a distinctly separate situation in their life, such as marital or employment difficulties.
Some patients have tried to diet many times in their life but tend to regain the weight. Not uncommonly, patients who undergo liposuction notice that their appetite decreases for several months postoperatively. This decreased appetite can provide the impetus for the patient to protect his or her investment by not overindulging in the future. Furthermore, some patients who are fixated on losing that last little bulge may adversely affect the quality of their life by excessively exercising at the expense of time that could be spent with their family, with their friends, or at work. Because that bulge may be refractory to exercise-induced volume reduction, they may increase their efforts unsuccessfully and further detract from other elements of their life. Liposuction could provide them an instantaneous relief. Another benefit of liposuction in women that has been described is possible breast enlargement in patients undergoing liposuction in other body areas.
Liposuction is generally performed for the reduction of focal adipose accumulations unresponsive to diet and exercise. Common anatomic areas for liposuction include the following:
-
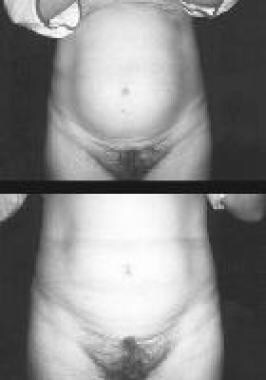
Upper and lower abdomen (see images below)
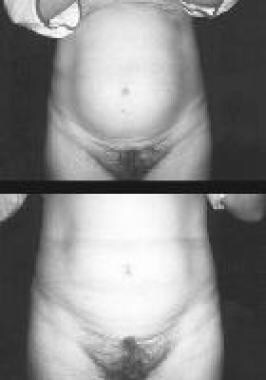 Top, preoperative view. Bottom, postoperative view 2 weeks after liposuction of the lower part of the abdomen.
Top, preoperative view. Bottom, postoperative view 2 weeks after liposuction of the lower part of the abdomen.
-
Ankles
-
Calves
-
Although controversial, liposuction alone, has been used for breast reduction as an alternative to traditional breast reduction surgery, which can leave inverted-T scars (see Liposuction Only Breast Reduction).
Other situations exist that may benefit from tumescent liposuction. These include lipoma removal, [6, 7] Madelung disease, axillary hyperhidrosis, [7] axillary bromhidrosis, [8] evacuation of hematomas, pseudogynecomastia, [7, 9] and the controversial staged liposuction for persons who are morbidly obese. Megaliposuction for persons who are morbidly obese performed in one session is extremely controversial because of the higher risk of mortality from fluid shifts.
The patient should be seen in consultation where the history is explored in detail. Medication intake; medication allergies; prior surgeries and results, including scarring; history of medical diseases, especially bleeding diatheses; personal and family history of cerebral vascular events; phlebitis; seizures; myocardial infarctions or angina; congestive heart failure; and hepatic disease all should be discussed. The patient's goals should be understood. Explanation of the procedure, its risks, alternatives, benefits, and convalescence should be explained, and questions should be answered. The insertion marks should be planned, if at all possible, to be placed in hidden areas while the patient is wearing the typical item of clothing (eg, swimwear, undergarment).
Technique
Many authors describe their approach to different body sites. Consent is obtained. Photographs are taken. The skin is prepared with a disinfectant. A sterile marking pen is used to draw a topographic map of the areas to be aspirated while the patient is standing. The insertion sites are marked. The patient is placed on sterile drapes and/or towels, and standard local anesthetic is used to infiltrate the skin of the insertion sites. A small entry is made into these sites by using a No. 11 blade, a NoKor needle, or a 1.5-mm punch.
The site is widened and pretunneled into the subcutaneous tissue by using a small, curved hemostat. A blunt infusion catheter is then inserted via this tunnel into the proposed surgical site, and tumescent anesthetic is delivered first to the deepest layer in a radial fashion and then successively more superficially. Infiltration of anesthetic is achieved with an electric-powered peristaltic pump. Some physicians prefer to use a spinal needle for infiltration without regard to specific insertion sites.
Although the addition of hyaluronidase may hasten the diffusion of anesthetic, this addition may allow for increased absorption, different peak levels, and duration of anesthetic effect. The addition of corticosteroid is also avoided because it has not been found to decrease postoperative soreness and because it may increase the risk of infection.
Cross-tunneling, or inserting the cannulae from 2 different axes (usually perpendicularly), creates a smoother result and is often used during the tumescent local infiltration as well. Peripheral mesh-undermining is a process in which the cannulae are introduced beyond the topographic map of the surgical area, without suction aspiration, to blend the affected area with the peripheral normal contour. This technique helps avoid a sharp step-off contour at the edge of the surgical site.
The liposuction cannulae, whether hooked up to machine aspirations or a syringe technique, are placed through insertion sites while the nondominant hand continually monitors the placement and the trajectory of the cannula. This "brain hand" also enables the surgeon to feel the progress of the area and to determine the endpoint of surgery. Once the desired result is obtained on the surgical table, the physician can have the awake patient stand up to judge if certain areas were missed and immediately return the patient to the table to complete the surgery. This technique has decreased the number of secondary procedures compared with the initial wet technique when patients were under general anesthesia or sedation. An orthostatic table does exist for surgeons to turn their patients who are under general anesthesia, in a "standing" position to check for their results, but this table has not yet become popular with American surgeons.
Some surgeons choose to suture the insertion sites immediately postoperatively, whereas other surgeons allow them to heal with second intent to allow for more drainage, less bruising, and less inflammation. Compression garments and absorptive pads are applied for the immediate postoperative period. This varies from several days to several weeks depending on the surgeon. The garments actually provide better comfort for many patients. The immediate swelling is related to the anesthetic, and, as this decreases, surgical swelling is noted in the first 2 weeks. The size of the garment is often decreased as this swelling resolves. Return to physical activities may be within a few days depending on the patient's comfort. Mild activity in the initial postoperative period is better than bed rest because it allows for better drainage and resorption of fluids, and it decreases stasis of blood flow in the extremities.
Postoperative care
Liposuction is performed on an outpatient basis, requiring only several hours, and the patient can return to home that evening.
Return to a normal activity level can occur within a few days to a couple of weeks.
Laser liposuction
Laser liposuction has received wide media attention as a procedure with similar efficacy but with less downtime than traditional liposuction. [19] The procedure has been marketed as SmartLipo, which uses a pulsed 1064-nm Nd:YAG system to help heat and possibly liquefy fat. Coagulation produced by the laser has been suggested as a possible benefit.
When combined with traditional tumescent liposuction, the results appear to be similar to those achieved with tumescent liposuction. Treatment of large areas with this technique also appears to be cumbersome, and most surgeons have limited its use to small anatomic areas such as the neck. Whether future refinements of the laser technique will truly add any value to tumescent liposuction, the criterion standard in fat removal, remains to be seen.
Complications
Complications of liposuction performed with a pure tumescent technique have been minimal. The most significant complications have been attributed to concurrent sedation or general anesthesia or fluid shifts secondary to large volume liposuction. [20] Fatalities have been associated with other concurrent surgical procedures, for example abdominoplasty performed with abdominal liposuction.
In an American Society for Dermatologic Surgery study of 15,336 patients, [21] no deaths were noted. In addition, no reports of pulmonary emboli, viscus perforation, thrombophlebitis, hypovolemic shock, seizures, or toxic reactions were described. Four cases of toxic shock syndrome were recognized, but, overall, the prevalence of infection ranged from 0.34-0.6%. Skin irregularity ranged from 0.26-2.1%. The rate of hematoma or seroma was only 0.17-1.6%, the rate of unacceptable scarring was 0.02%, the rate of sensory nerve impairment was 0.03-2.6%, and the rate of contact dermatitis was 0.12%.
In another survey, of 261 dermatologic surgeons who had performed 66,570 liposuction procedures, no deaths were reported.
Nonsurgical Alternatives
Nonsurgical adipose reduction technologies that have been developed include cryolipolysis, ultrasonic reduction treatment, and electromagnetic stimulation of underlying muscle contractions. Earlier attempts at adipose reduction using external laser sources were not successful in inducing long-term fat reduction.
Cryolipolysis
It has been shown that freezing kills fat cells. However, because the temperature required for adipocyte necrosis is higher than that at which skin freezes, the skin is preserved in this procedure, while the fat is affected. Several applicators have been developed to fit different body sites, with the therapy consisting of applying one or more applicators to the desired area of fat loss. Treatment lasts a minimum of 1 hour per applicator, and the procedure can be repeated at 1-2 months, if needed. There is some to moderate discomfort in the first 5-10 minutes of treatment, after which most patients feel numb for the rest of the session.
Cryolipolysis is a noninvasive procedure with minimal risk. Twenty percent volume reduction of adipose tissue has been shown by ultrasonographic studies to occur after one CoolSculpting treatment.
Ultrasound
The UltraShape ultrasound treatment is performed in a series of three biweekly sessions and is usually painless. The results are not as significant as those seen in cryolipolysis.
ThermiTight radiofrequency
There is a relatively new treatment, known as injectable radiofrequency, or Thermitight, which has been used either in place of or in conjunction with liposuction. [22] In this procedure, after local anesthetic is injected, a small cannula is inserted into the skin through a needle puncture. The fat is heated by radiofrequency energy, which not only causes the fat to melt but also results in adipocyte necrosis (cell death).
ThermiTight creates swelling and bruising for a few weeks; as in liposuction, compression garments are used.
-
Submental liposuction of the neck and the jowls. Left, preoperative view. Right, 3-month postoperative view.
-
Top, preoperative view. Bottom, postoperative view 2 weeks after liposuction of the upper arm.
-
Top, preoperative view. Bottom, postoperative view 2 weeks after liposuction of the lower part of the abdomen.
-
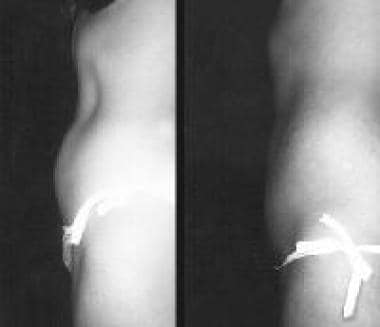
Left, preoperative view. Right, postoperative view 2 months after abdominal liposuction. The patient was a 30-year-old woman who exercised every day and, regardless of a healthy diet, could not lose the last inch off her abdomen until liposuction was performed.
-
Left, preoperative view. Right, postoperative view 3 months after liposuction of the love handles.
-
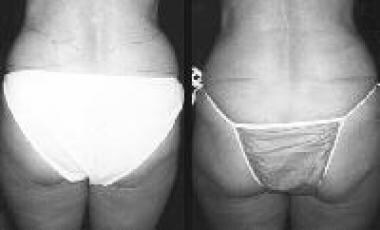
Top, preoperative view. Bottom, postoperative view 6 months after liposuction to the lateral parts of the thighs.
-
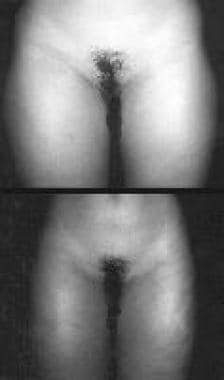
Left, preoperative view. Right, postoperative view 6 months after liposuction to the anterior parts of the thighs.
-
Top, preoperative view. Bottom, postoperative view immediately after liposuction to the inner parts of the knees.