Overview
Over the past decade, advances in laser technology have allowed cosmetic surgeons to diminish the appearance of scars and wrinkles using both ablative and nonablative lasers. Until recently, surgeons relied on chemical peeling, dermabrasion, surgical scar revision, electrosurgical planing, and dermal/subdermal filler substances (eg, collagen implantation, silicone injection, autologous fat transplantation) for the correction of scars and wrinkles. Today, physicians use 5 laser modalities for ablative skin resurfacing:
-
Scanned carbon dioxide laser
-
Pulsed carbon dioxide laser
-
Pulsed Er:YAG laser
-
Fractional Er:YAG laser resurfacing
-
Combination carbon dioxide and Er:YAG lasers
-
Fractionated photothermolysis [1]
Each of these treatments relies on the principles of selective photothermolysis in order to selectively target water-containing tissue and effect controlled tissue vaporization.
See the images below.
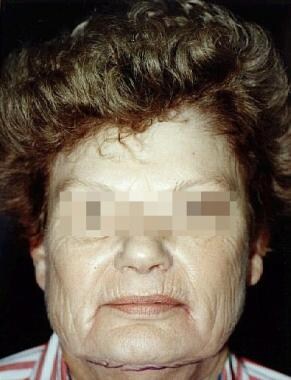 Before: Female patient with advanced dermatoheliosis and skin laxity before full face laser resurfacing with UltraPulse carbon dioxide laser.
Before: Female patient with advanced dermatoheliosis and skin laxity before full face laser resurfacing with UltraPulse carbon dioxide laser.
 After: Female patient with advanced dermatoheliosis and skin laxity 6 months after carbon dioxide laser resurfacing.
After: Female patient with advanced dermatoheliosis and skin laxity 6 months after carbon dioxide laser resurfacing.
The plasma skin regeneration system, Portrait (Rhytec; Waltham, Mass), was developed as a laser resurfacing device that used energy delivered via a burst of nitrogen plasma. One study reported that it was as effective as carbon dioxide laser resurfacing. [2] However, the manufacturer has since filed for bankruptcy and no longer makes the consumable tip used in the procedure. [3]
History and General Overview
The carbon dioxide laser became available in 1964 and soon became the most widely used laser in dermatologic practice. In the mid 1990s, carbon dioxide lasers became used for skin resurfacing, beginning the era of laser resurfacing. According to data collected by The American Society of Aesthetic Plastic Surgery, full-field and fractional laser resurfacing combined were the most popular nonsurgical procedures for skin rejuvenation in 2014. [4] The carbon dioxide laser emits an invisible infrared beam at a 10,600-nm wavelength, targeting both intracellular and extracellular water. When light energy is absorbed by water-containing tissue, skin vaporization occurs, with production of coagulative necrosis in the remaining dermis.
The conception of fractional photothermolysis in 2004 by Manstein and colleagues is considered one of the most important milestones in laser resurfacing. [5] During fractional photothermolysis, a pixilated pattern of full-thickness columns of coagulation is created. These columns of coagulation are termed microthermal zones (MTZ). [5, 6, 7] Over the past few years, fractional photothermolysis has been shown to be effective against many of the skin signs of photoaging (dyschromia, texture abnormalities, skin mottling, and moderate to severe rhytides). These effects are considered comparable to that of traditional ablative resurfacing but with significantly minimal side effects (scarring, dyspigmentation, severe erythema) with a down time of 5-7 days. [8] Short recovery time and rapid healing are attributable to the healthy tissue that surrounds the MTZs. [5, 6, 7]
Tissue vaporization is best accomplished with minimal coagulation or residual thermal damage when exposure times are shorter than 1 millisecond. In addition, 5 J/cm2 of energy is needed to exceed the vaporization threshold of the targeted skin. Two different carbon dioxide laser technologies can deliver sufficient energy to vaporize the skin in less than 1 millisecond. One involves the use of an ultra-short pulse to deliver the energy to tissue. The second uses a computer-controlled optomechanical shutter system, which scans a continuous wave beam so rapidly that the emitted light is prevented from contacting skin for more than 1 millisecond.
Several factors contribute to the fact that uniform laser parameters in clinical practice do not exist. While several clinical and histological studies have been reported in the medical literature, varying styles of laser practice between surgeons could affect end clinical results. In addition to the laser parameters chosen, for example, clinical effect is also influenced by the number of laser passes delivered, the degree of pulse or scan overlap, the complete/incomplete removal of partially desiccated tissue between each laser pass, preoperative preparation, and postoperative wound care.
Indications and Patient Selection
Indications
As with any modality, the surgeon must have a complete understanding of the indications and limitations of a given procedure. The carbon dioxide laser is a powerful tool in the cosmetic surgeon's armamentarium that can have beneficial effects when used properly for the correct indication.
Skin resurfacing with a pulsed or scanned carbon dioxide laser is largely used for improvement of fine or moderate rhytids. [9] While deeper rhytids may also be improved, other procedures such as autologous fat transplantation, Contour Treadlifting, Sculptra injections, Gore-Tex/other implantation, or surgical lifting can be used to provide additional benefit. Dyschromias, including solar lentigines, are often improved with laser resurfacing, although they are not generally regarded as a primary indication for treatment. Improvement of melasma has been reported, although the recurrence rate after laser resurfacing is high.
Carbon dioxide laser resurfacing may greatly improve atrophic scars caused by acne, trauma, or surgery. [10, 11, 12, 13, 14] Deeper pitted acne scars often require ancillary procedures for optimal results, such as excision or punch grafting. These procedures can be performed either prior to or concomitant with carbon dioxide laser resurfacing.
Carbon dioxide fractional photothermolysis has been shown to be effective against treating many of the same skin conditions as traditional ablative carbon dioxide lasers. Several studies have shown carbon dioxide fractional photothermolysis to be effective against rhytids, postinflammatory hyperpigmentation, melasma, nevus of Ota, hypopigmented and hyperpigmented scars, dyschromia, laser-induced hypopigmentation and hyperpigmentation, and poikiloderma of Civatte. [8] The ultrapulsed fractional carbon dioxide laser has been shown to be particularly effective against posttraumatic and pathological scars. [15, 16] In addition, fractional carbon dioxide laser devices has been shown to improve periorbital rhytids with skin tightening and elevation of the eyebrows. [17]
Other conditions that have been shown to respond favorably to carbon dioxide laser resurfacing include rhinophyma, severe cutaneous photodamage (observed in Favre-Racouchot syndrome), sebaceous hyperplasia, xanthelasma, syringomas, actinic cheilitis, chronic lip fissures, [18] diffuse actinic keratoses, and cutaneous leishmaniasis. [19] Carbon dioxide laser ablation has also been suggested as a mode of therapy for cutaneous malignant melanoma metastases, but further studies are needed to confirm this. [20] The carbon dioxide laser was used more often in the past for tattoo removal (in conjunction with dermabrasion and salabrasion); however, its use for this purpose has been largely abandoned because of the availability of more tattoo-specific lasers.
Treatment areas
The success of a cutaneous resurfacing procedure relies upon the presence of skin appendages (eg, sweat glands, folliculo-infundibular units) to serve as sources of epithelium that can migrate upward to form the new epidermis. Therefore, the greater the number of skin appendages per square centimeter of skin, the more rapid the healing and the less risk for scarring. For this reason, carbon dioxide laser resurfacing is largely limited to the face. Resurfacing of the hands and neck has been successful, although much greater risk for scarring exists when treating these areas.
Patient selection
As with any cosmetic procedure, proper patient selection is essential. During the initial consultation, the surgeon should ascertain the patient's expectations of treatment. Also, ascertain how the patient arrived at the decision to have cosmetic surgery. A primary assessment of Fitzpatrick skin type, ethnicity, and skin condition to be treated (ie, pigmentation, wrinkles). The latter is essential in determining laser treatment, such as one-time, full-field or multiple fractional laser sessions, as well as the time commitment necessary for proper healing. [21] In addition, a complete medical and surgical history, including recent use of isotretinoin should be obtained, because its regular use within 6 months to 1 year of dermabrasion has shown a higher risk of hypertrophic scarring. History of previous laser resurfacing, dermabrasion, or deep phenol peel is noteworthy because these procedures could potentially slow the wound healing response owing to the presence of fibrosis. Patients with a prior history of transcutaneous lower blepharoplasty and limited infraorbital elasticity may have increased risk of ectropion. When applicable, patients should be discouraged from smoking before and after surgery to reduce the risk of delayed or impaired wound healing.
A thorough examination of the skin to be treated should be performed, carefully noting scarring, dyschromia, rhytid formation, and skin type. For patients desiring periorbital laser treatment, a careful examination of the eyes for scleral show, lid lag, and ectropion should be performed. Other cutaneous disorders should also be investigated, including seborrheic keratosis, solar lentigines, actinic keratosis, acne vulgaris, and cutaneous carcinomas. The latter should be treated prior to any resurfacing procedures.
With this information, the benefits of laser resurfacing must be assessed, along with its limitations, risks, and benefits. The required recovery period is a critical discussion during consultation. For example, some patients cannot afford to spend a full week healing; thus, multiple fractional laser sessions over a period of months may be a more feasible option. Perhaps most important, one must be certain the patient has realistic expectations and sound reasons for deciding to undergo the cosmetic laser surgical procedure. Other cosmetic surgery treatments should be reviewed so that the patient may make an informed decision.
Contraindications and Cautions
Patient safety
Absolute contraindications include isotretinoin use within the previous 6 months; active cutaneous bacterial, viral, or fungal infection in the area to be treated; and ectropion (for infraorbital resurfacing). Additionally, those with appendageal abnormalities involving the hair follicles and sebaceous glands should not undergo laser treatment. Wound healing is dependent on precursor cells present within and adjacent to these appendages. Owing to their lack of proper appendages, the presence of skin grafts in the treatment area is a contraindication to deep full field resurfacing.
Relative contraindications include patient history of keloid formation or hypertrophic scarring, ongoing ultraviolet exposure, prior radiation therapy to treatment area, and collagen vascular disease.
Caution should be taken with patients who smoke or who have a history of previous laser resurfacing, phenol chemical peel, dermabrasion, and/or transcutaneous lower blepharoplasty. Also, patients planning to undergo neck or extremity laser resurfacing should be forewarned of the increased risk of fibrosis in these areas.
Laser safety
Detailed guidelines have been published on proper laser safety practices. In both ablative and nonablative laser therapy, practitioners should take precautionary steps to prevent the occurrence of fire and to ensure adequate eye safety. Though rare, laser use may ignite fire in the presence of open oxygen sources (ie, nasal cannula), paper products, and other flammable materials. Placing wet towels around the face is recommended by some in order to prevent this hazard. Concerning eye protection, patients and all present in the treatment room must use laser-specific eye shields that can be an external or internal contact lens-type model.
Antiviral Agents and Antibiotics: Their Roles in Laser Resurfacing
Oral antiviral agents
Because laser skin resurfacing can cause reactivation of latent herpes simplex infection or can predispose the patient to a primary infection during the reepithelialization phase of healing, surgeons are recommended to routinely prescribe the prophylactic use of an antiviral medication during the postoperative period, regardless of a patient's herpes simplex virus history. Some surgeons begin the regimen 24 h prior to surgery, while others initiate treatment on the morning of surgery. Commonly used regimens include famciclovir 250 mg PO bid, acyclovir 400 mg PO tid, and valacyclovir 500 mg PO bid for 7-10 d.
Antibiotics
Some surgeons routinely prescribe antibiotics for bacterial prophylaxis; however, little data exist to support their use, given the relatively low incidence of postoperative bacterial infection. [22] When used, a cephalosporin (cephalexin), semisynthetic penicillin (dicloxacillin), macrolide (azithromycin), or quinolone (ciprofloxacin) is begun 1 day before or on the day of surgery and continued until reepithelialization is complete. The use of topical antibiotics on the laser-induced wound is not routinely recommended because of the possibility of contact dermatitis.
Anesthesia
For localized areas, local infiltration with 1% lidocaine with epinephrine or tumescent anesthesia using standard Klein solution is usually sufficient to produce adequate anesthesia. For larger areas, such as full-face resurfacing, nerve blocks (eg, supraorbital, supratrochlear, infraorbital, mental) are often used with local infiltration. However, a 2016 study on whole-face carbon dioxide laser resurfacing found a statistically significant reduction in pain experienced by patients with topical anesthetic treatment after the addition of microneedle anesthetic application using a roller-type device. [23] This method may prove to be an effective and a less invasive option than nerve blocks. Some surgeons use tumescent anesthesia with or without nerve blocks to provide local anesthesia, while others prefer to use conscious sedation (or twilight anesthesia) alone or in conjunction with other techniques.
Commonly Used Laser Parameters and Other Variables
While clinical and histologic studies using various laser parameters and different laser systems have been performed, no consensus has been reached regarding the optimal parameters to use in every clinical setting. Most surgeons use their experience and the experience of others as guidance in determining the parameters to use in each case. [24]
A 1998 study by Weisberg and colleagues [25] evaluated different laser parameters using both pulsed and scanning carbon dioxide lasers in order to determine threshold fluences and to compare the effects of tissue debridement.
Maximal skin shrinkage of 5.1 ± 0.1% shrinkage per pass occurred using the scanned laser (Sharplan Silktouch) at 2.7 W (5.9 J/cm2) with debridement between passes. If not debrided between passes, skin shrinkage is maximal at 13 ± 5 J/cm2 (6 ± 2 W), which yields 2.4 ± 0.5% shrinkage per pass. These findings were compared with the pulsed laser (Coherent Ultrapulse), which achieved a maximal shrinkage of 3.6% at 2.5 J/cm2 (220 mJ). Without debridement, results were similar with 2.3-2.4% shrinkage using the pulsed laser at 990 mJ (11 J/cm2) and the scanned laser at 13 J/cm2 (6 W). Skin thermal denaturation, however, was shown to be a maximum of 25 µm with the pulsed carbon dioxide laser at 320 mJ (3.5 J/cm2) and 77 µm with the scanned laser at 9.1 J/cm2 (4.2 W).
These findings are consistent with previous studies showing that the Ultrapulse laser typically causes less thermal injury to surrounding tissue than the scanned Silktouch.
In 2013, Tsung-Hua and colleague Jung-Yi tested an alternative method to traditional histology to adjust laser parameters in real time to provide more individualized therapy for patients. [26] Multiphoton microscopy was used to monitor skin reactions immediately after carbon dioxide laser irradiation in vivo using nude mouse skin. This study found a significant difference using multiphoton microscopy to determine the zone of tissue ablation and disruption of the surrounding stratum corneum, keratinocytes, and dermal extracellular matrix after high-fluence carbon dioxide laser treatment. In addition, quantification of collagen damage in the residual thermal zone was successful in control, low-fluence laser-treated, and high-fluence laser-treated skin by using second harmonic generation microscopy signals. Multiphoton and second harmonic generation microscopy may prove to be effective noninvasive imaging modalities in the clinical setting when assessing patient carbon dioxide laser-skin reactions and thermal damage in real time.
Berlin et al report that carbon dioxide laser resurfacing using a fractional ablative, scanned, nonsequential technique is safe and effective to repair photodamaged skin. Ten patients (Fitzpatrick types I-III) experienced cosmetic improvement and had light microscopy evidence of wound repair and electron microscopy evidence of new collagen deposition. [27]
Postoperative Care and Complications
Postoperative wound care
Postoperative wound care varies considerably from surgeon to surgeon. Wounds reepithelialize more rapidly in a moist environment. Also, crust and eschar impede keratinocyte migration and retard the healing process. Therefore, most surgeons advocate maintaining a moist environment either with topical emollients and/or with semiocclusive dressings.
Postoperative wound care can follow an open or closed method. With the closed method, a semiocclusive dressing (usually involving hydrogel) is placed on the denuded skin. These wound dressings have been shown to accelerate the rate of reepithelialization by maintaining a moist environment. In addition, decreased postoperative pain has been reported with their use. However, some believe that occlusive dressings also yield a low-oxygen environment that may promote the growth of anaerobic bacteria, thereby causing infection and impeding wound healing. As such, many proponents of the closed technique now combine the use of semiocclusive dressings with topical emollients. Others simply advocate the use of an open postoperative method, involving the application of copious amounts of topical emollients to promote rapid reepithelialization without risking prolonged occlusion and inability to observe the wound surface.
Complications after laser resurfacing [28]
Carbon dioxide laser resurfacing imparts a thermal injury to denuded skin. Therefore, side effects are expected and must be differentiated from complications. Nearly all patients encounter side effects ranging from postoperative pain and edema to pruritus and tightness.
Mild complications sometimes occur and usually are of minimal consequence. Minor complications include milia formation, perioral dermatitis, acne and/or rosacea exacerbation, contact dermatitis, and postinflammatory hyperpigmentation. Treatment with hydroquinone can effectively attenuate hyperpigmentation. Providers might consider the addition of serial glycolic acid peels in patients with Fitzpatrick skin types III-VI, as they are more prone to pigmentary changes. [29, 30]
Moderate complications include localized viral, bacterial, and candidal infection; delayed hypopigmentation; persistent erythema lasting up to 10 months; and prolonged healing. Braun et al report two cases of successful reduction of posttreatment erythema after topical brimonidine tartrate gel without rebound erythema after treatment cessation. [31] Ideally, to reduce the appearance of hypopigmentation, the entire face, or at least regional subunits, should be treated in order to minimize demarcation between treated and untreated areas.
The most severe complications are hypertrophic scarring, disseminated infection, and ectropion.
Early detection of complications and rapid institution of appropriate therapy are extremely important. Delay in treatment can have severe deleterious consequences, including permanent scarring and dyspigmentation.
-
Before: Female patient with advanced dermatoheliosis and skin laxity before full face laser resurfacing with UltraPulse carbon dioxide laser.
-
After: Female patient with advanced dermatoheliosis and skin laxity 6 months after carbon dioxide laser resurfacing.
Tables
What would you like to print?
- Overview
- History and General Overview
- Indications and Patient Selection
- Contraindications and Cautions
- Antiviral Agents and Antibiotics: Their Roles in Laser Resurfacing
- Anesthesia
- Commonly Used Laser Parameters and Other Variables
- Postoperative Care and Complications
- Show All
- Media Gallery
- References









