Background
Warty dyskeratoma (WD) is a benign epidermal proliferation first reported in 1957 because of its distinctive histologic findings. [1] WD presents as an umbilicated papule with a keratotic plug, usually limited to the head, neck, or face. Lesions are generally solitary and sporadic and may be associated with a follicular unit. Oral involvement, [2, 3] particularly the hard palate, eyelid, [4] and genital involvement have been reported. [5] Multiple lesions may occur in the same patient. [6, 7, 8, 9]
Although originally referred to as isolated keratosis follicularis, no data support that patients with a WD bear germline mutations in ATP2A2, the gene responsible for Darier disease. Patients with Darier disease have been reported with WDs occurring spontaneously or during treatment with systemic retinoids. [10]
Pathophysiology
Warty dyskeratoma (WD) represents a sporadic localized error in epithelial maturation and cohesiveness. James Fitzpatrick, MD, of Dermatopathology Consultants of Colorado, has shown using immunohistochemistry that these tumors lack SERCA2 thus providing evidence that an acquired genetic mutation in ATP2A2 plays a role in tumor development. Malunion and premature keratinization of epithelial cells occur. Attempts to demonstrate that human papillomavirus plays a role have proven unsuccessful. [11] Other adhesion molecules may also play a role.
Etiology
James Fitzpatrick, MD, of Dermatopathology Consultants of Colorado, has demonstrated using immunohistochemistry (unpublished work) that warty dyskeratoma demonstrates absence of SERCA2. This finding suggests that acquired genetic mutations in ATP2A2, as demonstrated by the absence of its protein product, SERCA2, play a role in the development of WD. See the image below.
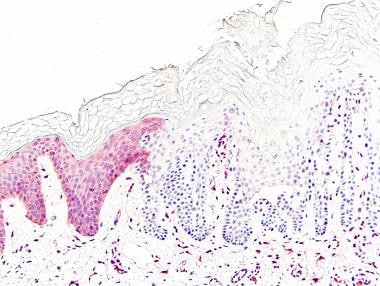 Absence of sarco/endoplasmic reticulum Ca2+ ATPase 2 (SERCA2) staining by immunohistochemistry within a warty dyskeratoma (right side of image), in contrast to the unaffected epidermis (left side of image). Photomicrograph courtesy of James E. Fitzpatrick, MD.
Absence of sarco/endoplasmic reticulum Ca2+ ATPase 2 (SERCA2) staining by immunohistochemistry within a warty dyskeratoma (right side of image), in contrast to the unaffected epidermis (left side of image). Photomicrograph courtesy of James E. Fitzpatrick, MD.
To date, genetic evaluations of warty dyskeratoma (WD) for mutations in ATP2A2 (gene encoding SERCA2) have not been reported in the literature.
Two reports have demonstrated immunohistochemical staining of WD with antikeratin antibodies HKN-6 and HKN-7, and this reaction was interpreted as suggesting a follicular origin for WD.
Ultrastructural findings have been interpreted to suggest that acantholysis is due to a defect in desmosome-tonofilament complexes.
Epidermal viral infection with secondary hyperproliferation and acantholysis has also been proposed as a causative mechanism. However, a 2002 study showed that 13 of 13 cases did not show human papillomavirus DNA after polymerase chain reaction testing, and no data support a viral etiology at this time. [11]
Epidemiology
Frequency
Warty dyskeratoma (WD) is an uncommon lesion. Involvement of the mucosal surfaces is also uncommon.
Race
No racial predilection is known.
Sex
By a modest margin, warty dyskeratoma affects men more commonly than women.
Age
The average patient age at diagnosis for focal, oral warty dyskeratoma is 52.2 years; 10 of 13 reported patients were between the fifth and seventh decades of life.
Prognosis
There is no known risk of malignant transformation of warty dyskeratoma (WD). Recurrence after surgical removal is extremely uncommon. Although WD is histologically similar to Darier disease and appears to share the same absent protein (SERCA2) in at least some cases, no evidence indicates that patients with warty dyskeratoma are at risk for other disorders, including Darier disease.
Patient Education
Patients should be reassured that warty dyskeratoma (WD) is benign. While patients with Darier disease have been reported with WD, [12] the diagnosis of WD does not imply that the patient has Darier disease nor is at risk for transmitting Darier disease to offspring. Isolated WD is not associated with other systemic diseases and patients with a WD do not need routine follow-up in dermatology.
-
Absence of sarco/endoplasmic reticulum Ca2+ ATPase 2 (SERCA2) staining by immunohistochemistry within a warty dyskeratoma (right side of image), in contrast to the unaffected epidermis (left side of image). Photomicrograph courtesy of James E. Fitzpatrick, MD.
-
Warty dyskeratoma. An endo-exophytic squamous proliferation of cytologically benign, acantholytic, and dyskeratotic keratinocytes.
-
Villi lined by acantholytic keratinocytes, some of which are dyskeratotic (corps ronds and corps grains).









