Practice Essentials
Pityriasis alba, a common skin disorder in children and young adults, most commonly between ages 3 and 16 years. [1] It is characterized by the presence of ill-defined, scaly, faintly erythematous patches. These lesions eventually subside, leaving hypopigmented areas (see the image below) that then slowly return to normal pigmentation. The term is derived from the words pityriasis (scaly) and alba (white).
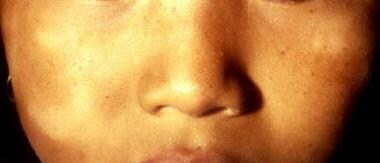
 Note the characteristic, ill-defined, hypopigmented macules in this 6-year-old child with pityriasis alba.
Note the characteristic, ill-defined, hypopigmented macules in this 6-year-old child with pityriasis alba.
Signs and symptoms
Pityriasis alba lesions often occur on the face, with the cheek being a particularly common site. [2] Initially, erythema may be conspicuous, and minimal serous crusting of some lesions may occur. The individual lesions are characterized as follows:
-
Rounded, oval, or irregular plaques that are red, pink, or skin colored and have fine lamellar or branny scaling with indistinct margins
-
Usually 1-4 cm in diameter
-
Most commonly range in number from 4 or 5 to 20 or more
-
Found on the face, upper arms, neck, or shoulders; the legs and trunk are less commonly involved; in approximately one half of all patients, the lesions are limited to the face [3]
Uncommon variants of pityriasis alba are as follows:
-
Pigmenting pityriasis: Typical lesion has a central zone of bluish hyperpigmentation surrounded by a hypopigmented, slightly scaly halo of variable width; the lesions are usually confined to the face and are often associated with dermatophyte infection [4] This entity is typically found in darker skin types from South Africa and the Middle East. [1]
-
Extensive pityriasis alba (see Differentials): Differentiated from the classic form by the widespread and symmetrical involvement of the skin, the absence of a preceding inflammatory phase, a higher female-to-male ratio, and, histologically, the absence of spongiosis [5]
In the extensive variant, lesions are less erythematous, less scaly, more persistent, asymptomatic, and more frequently seen on the trunk and less often on the face. [6]
See Clinical Presentation for more detail.
Diagnosis
A workup, as follows, may be undertaken to exclude other causes of hypopigmentation:
-
Wood's light examination: May help in determining the presence of vitiligo, which will glow more brightly and have edges with sharper demarcation
-
Potassium hydroxide (KOH) stain of a skin scraping: Will be positive if the patient has tinea versicolor (also called pityriasis versicolor), tinea faciei, or tinea corporis
-
Skin biopsy: Not usually necessary or particularly helpful in establishing a diagnosis of pityriasis alba but may be indicated if a diagnosis of mycosis fungoides (cutaneous T-cell lymphoma) is a significant possibility [7]
See Workup for more detail.
Management
Pityriasis alba resolves spontaneously; treatment consists primarily of good general skin care and education of a young patient’s parents about the benign nature of this self-limited disorder. Therapy may also include the following:
-
Low-potency topical steroids (eg, hydrocortisone 1%, desonide 0.05%): May help with erythema and pruritus associated with the initial lesions and may accelerate repigmentation of existing lesions; use should be limited, however, to avoid long-term skin atrophy and steroid changes
-
Tar paste: May be helpful for chronic lesions on the trunk
-
Bland emollient cream: Used to reduce the scaling of lesions, especially on the face
-
Psoralen plus ultraviolet light A (PUVA) photochemotherapy: May be used to help with repigmentation in extensive cases; recurrence rate is high after treatment is stopped [8]
-
Laser therapy: Treatment with a 308-nm excimer laser twice a week for 12 weeks has been shown to be effective against pityriasis alba [12]
See Treatment and Medication for more detail.
Background
Pityriasis alba, a relatively common skin disorder in children and young adults, is characterized by the presence of ill-defined, scaly, faintly erythematous patches. These lesions eventually subside, leaving hypopigmented areas that then slowly return to normal pigmentation (see the images below). [1, 13] Lesions may progress through the following three clinical stages (see Clinical Presentation):
- Papular (scaling) erythematous
- Papular (scaling) hypochromic
- Smooth hypochromic
 Note the characteristic, ill-defined, hypopigmented macules in this 6-year-old child with pityriasis alba.
Note the characteristic, ill-defined, hypopigmented macules in this 6-year-old child with pityriasis alba.
The duration of pityriasis alba varies from 1 month to 10 years, with most cases resolving over a period of several months to a year. [2] Diagnosis is made clinically, and treatment consists of skin care and education of a young patient’s parents about the benign nature of the disorder. Hydrocortisone may decrease erythema, scaling, and pruritus, if present. (See Prognosis, Workup, and Treatment.)
Pityriasis alba, although a nonspecific finding, is commonly associated with atopic dermatitis. The etiology of pityriasis alba is unknown, but xerosis that presents in individuals with atopic diathesis is an important element in the development of the disease. (See Pathophysiology and Etiology.)
Extensive pityriasis alba
Extensive pityriasis alba is believed to be a primary, acquired hypopigmentation observed in females aged 18-25 years of mixed ethnic origin; it is characterized by hypochromic, nonscaly macules developing on the back and abdomen, increasing in number and progressively coalescing over the whole trunk into larger patches surrounded by smaller, well-defined macules. Although the single skin lesions of extensive pityriasis alba do not differ substantially from those of pityriasis alba, consistent differences are as follows [14] :
-
A widespread and symmetrical involvement of the trunk by numerous round, nonscaly, hypomelanotic patches without a preceding inflammatory phase and chronic in duration (this is as opposed to face predominance, as found in pityriasis alba)
-
A decrease in epidermal melanin, as found on histologic examination; spongiosis is absent
-
Ultrastructural studies suggest a reduced number of active melanocytes and a decrease in number and size of melanosomes
-
No reported atopy, associated pathologies, or familial occurrences
-
The age of occurrence and the sex ratio (female preponderance) differ from those of pityriasis alba
Widespread lesions of classical pityriasis alba can be observed in atopic dermatitis, but they should not be confused with those of extensive pityriasis alba
Debate exists as to the validity of the term extensive pityriasis alba, which some believe to be a confusing misnomer applied to a pathoetiologically different entity. Some authors believe that extensive pityriasis alba overlaps with another condition, described as "progressive and extensive hypomelanosis" in persons of mixed racial background and also reported as "progressive and confluent hypomelanosis of the melanodermic metis" or "creole dyschromia.” The alternate name of "progressive extensive hypomelanosis" has been proposed. [14]
Patient education
Educate the parents about the benign, self-limited nature of pityriasis alba.
Pathophysiology
Pityriasis alba
Ultrastructural studies in patients with pityriasis alba have noted that despite reduced pigment in lesional skin, there is no difference in melanocytes between lesional and nonlesional skin in the same patient, although this finding is still under debate. Degenerative changes in melanocytes and reduced keratonocyte melanosomes have also been noted. [15]
Extensive pityriasis alba
Hypopigmentation in extensive pityriasis alba may be primarily caused by the reduced numbers of active melanocytes and the decrease in the number and size of melanosomes in the affected skin.
In a study by Zaynoun et al of 9 patients with extensive pityriasis alba, the density of functional melanocytes was found to be reduced in affected areas, although cytoplasmic activity and the transfer of melanosomes to keratinocytes were generally normal. While the number and size of melanosomes tended to be reduced, they demonstrated a normal distribution pattern in the keratinocytes. [16]
In the same study, the presence of hyperkeratosis and parakeratosis was inconsistent, and these conditions were thought unlikely to contribute significantly to the pathogenesis of the hypomelanosis. Various amounts of intercellular edema were found.
Etiology
No known cause of pityriasis alba has been reported. The condition is not contagious, and no infectious agent has been identified.
Leading theories as to the origin of the lesions in pityriasis alba involve atopy and postinflammatory changes, with a large number of patients with pityriasis alba having a history of atopic disease, and atopic patients are being more prone to developing the condition. [17, 2]
Theories of origin also include hypopigmentation secondary to pityriacitrin, a substance produced by Malassezia yeasts that acts as a natural sunscreen.
In one study, atrophic sebaceous glands were noted in almost half the cases of pityriasis alba. In another study, iron deficiency anemia was reported in 16.5% of patients [2] ; this may be a coincidental finding, however, and the clinical relevance of anemia is not yet known. Excessively dry skin, which is frequently exacerbated by cold, dry environments, also appears to be a common factor in pityriasis alba.
Reported contributory factors related to the development of pityriasis alba are excessive and unprotected sun exposure, poor hygienic habits, and environmental influences such as temperature, humidity, and altitude. [18, 19] In addition, one study has shown patients with pityriasis alba were more likely to have low levels of serum copper, possibly contributing to tyrosinase dysfunction, and therefore a decrease in the production of melanin. [20]
Epidemiology
Occurrence in the United States
Although the exact incidence has not been described, up to 5% of children may have pityriasis alba. [21] The disorder is not seasonal, but the dry, slightly scaly appearance tends to worsen during cold months, when the air is relatively dry inside the home. In addition, sun exposure may make the lesions more obvious during spring and summer. The condition is more common in patients with a history of atopy.
International occurrence
In a study of 9955 schoolchildren aged 6-16 years who lived in a tropical region, the prevalence of pityriasis alba was 9.9%. [22, 23] Another study, in Nepal, showed that the prevalence of pityriasis alba within a wide range of dermatoses was 5.2%. [24]
Race-, sex-, and age-related demographics
Pityriasis alba occurs in people of all races. One study found the incidence to be slightly higher in light-skinned people, while other studies have demonstrated the opposite. The condition is frequently more apparent and cosmetically bothersome in patients with darker complexions. [17, 19] Both sexes are equally susceptible to the disease, but a slight male predominance has been noted. [2, 18]
Pityriasis alba is most common in children aged 3-16 years, with 90% of cases occurring in children younger than 12 years. The disease occasionally is found in adults. [17]
Prognosis
Pityriasis alba is generally self-limited, and the prognosis is good, with eventual complete repigmentation. No long-term residual effects are expected.
Cosmetic appearance while the lesions are present may be an issue with some pediatric patients but is more likely to be of concern to their parents. Risk of sunburn is slightly increased in areas of hypopigmentation.
The duration of symptoms is different for each patient. Recurrent crops of new lesions may develop at intervals, with the duration of pityriasis alba varying from 1 month to 10 years. Usually, however, cases resolve over a period of several months to a year. [2] Treatment may shorten the duration of the lesions to several weeks in certain cases. (See the image below.)
-
Note the characteristic, ill-defined, hypopigmented macules in this 6-year-old child with pityriasis alba.
-
Lesions of pityriasis alba are usually bilateral and located on the face, arms, and neck.
-
The hypopigmentation produced by pityriasis alba may take a year or longer to return to normal.
-
This older patient with areas of hypopigmentation on the face has a common problem that would be included in the differential diagnosis of pityriasis alba. Several months earlier, he had areas of irritant contact dermatitis on his cheeks. When those resolved, he was left with areas of postinflammatory hypopigmentation. These should eventually repigment to an even skin tone.
-
Pityriasis alba.