Practice Essentials
The various types of pemphigus include pemphigus erythematosus, pemphigoid, pemphigus vegetans, pemphigus vulgaris, and pemphigus foliaceus.
Pemphigus erythematosus, also known as Senear-Usher syndrome, is an overlap syndrome with features of lupus erythematosus (LE) and pemphigus foliaceus. Pemphigus is demonstrated by acantholysis and immunoglobulin deposits in the interkeratinocyte substance (see the image below).
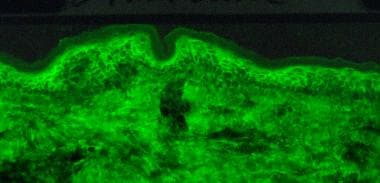 Direct immunofluorescence microscopy performed on epithelial biopsy specimen obtained from a patient with pemphigus vulgaris detects immunoglobulin G deposits at the epithelial cell surfaces.
Direct immunofluorescence microscopy performed on epithelial biopsy specimen obtained from a patient with pemphigus vulgaris detects immunoglobulin G deposits at the epithelial cell surfaces.
Pérez-Pérez et al hypothesized that pemphigus erythematosus is a multiple autoimmune disease. [1]
High doses of UV light are suggested to be the cause of cleavage of the desmoglein-1 ectodomain. As in cases of pemphigus foliaceus the circulating anti–desmoglein-1 antibodies precipitate this cleaved off ectodomain along with the basement membrane zone, resulting in a lupus band–like appearance.
The lupus component of pemphigus erythematosus is demonstrated by circulating antinuclear antibodies (ANA) and sometimes by immunoglobulin and complement deposits at the dermoepidermal junction.
Signs and symptoms
Patients with pemphigus erythematosus present with vesiculobullae or superficially eroded lesions, which may ooze and crust, particularly in sun-exposed areas, such as the face, the upper part of the chest, and the back.
Onset and progression of pemphigus erythematosus are typically slow. Although the distribution of the pemphigus erythematosus lesions should suggest induction by sunlight, the patient may be completely unaware of the photosensitive nature of the disorder.
Pemphigus erythematosus lesions typically involve the scalp, the face, the upper part of the chest, and the back. [2] Patients with classic pemphigus erythematosus present with small, flaccid bullae with scaling and crusting. Occasionally, the appearance may suggest a papulosquamous disorder. On the face, pemphigus erythematosus presents on the bridge of the nose and on the malar areas as in the butterfly distribution seen in LE.
Secondary infection may occur, resulting in impetiginization, in healing with pigment changes, and in scarring.
With extensive involvement, pemphigus erythematosus patients may present with an exfoliative erythroderma. The skin may be tender. Patients with pemphigus erythematosus do not typically develop mucous membrane involvement. Electrolyte imbalance and loss of temperature control can occur with extensive skin involvement.
Diagnostics
In pemphigus erythematosus, select an early vesicle or bulla for skin biopsy. Perilesional skin is tested on immunofluorescence studies.
With direct immunofluorescence (see the image above) in pemphigus erythematosus, linear deposits of immunoglobulin G (IgG) and C3 are present in the intercellular space of the epidermis. Granular deposits of C3 and IgG at the dermoepidermal junction are present in 80% of patients, particularly in biopsy specimens from the face or other sun-exposed areas. [3]
With immunoelectron microscopy in pemphigus erythematosus, IgG and C3 deposits are localized to the epidermal cell membranes and the upper dermis.
Enzyme-linked immunosorbent assay (ELISA) has also been suggested as a useful diagnostic method in suspected cases of pemphigus erythematosus with equivocal immunofluorescence results. [4]
Patients with pemphigus erythematosus may have other laboratory abnormalities suggestive of systemic lupus erythematosus (SLE); these include anemia, lymphopenia, thrombocytopenia, renal abnormalities, proteinuria, or a positive rheumatoid factor.
Also see Histologic Findings.
Management
Also see Medication.
Topical therapy
Topical corticosteroids are useful for pemphigus erythematosus patients with limited disease or as an adjunct to systemic therapy. Selection of the appropriate topical steroid strength and vehicle depends on the body site, the age of the patient, and the potential for steroid adverse effects. [5] Use of daily sunscreen and sun protection is necessary. Griffies et al reported promising results in treating discoid lupus and pemphigus erythematosus in dogs with topical application of 0.1% tacrolimus, an immunomodulator produced by a fungus. [6] Remission with tacrolimus occurred alone in some dogs, whereas steroid use was decreased or discontinued in other dogs.
Systemic therapy
Systemic steroids have been the mainstay of therapy for widespread pemphigus since their first use in 1950. Prednisone at 1-2 mg/kg/d as a single morning dose or as intravenous pulses may control the disease. Appropriate monitoring is critical.
Dapsone is effective in some patients with pemphigus erythematosus. [7, 8] Patients tend to respond relatively quickly, with improvement within several weeks. It can be a steroid-sparing drug. The possible mode of action is stabilization of lysosomal membranes and inhibition of polymorphonuclear leukocyte (PMN) toxicity. The recommended dose is 100-200 mg/d. Hemolytic jaundice may result in people with G-6-PD deficiency. Other adverse effects include agranulocytosis, leading to death, headaches, malaise, hepatitis, hypersensitivity reactions, and neuropathy. Caution is required.
Azathioprine is a potent immunosuppressive agent that has been used as a steroid-sparing agent. The usual doses are 0.5 -2.5 mg/kg/d, based on results of thiopurine methyltransferase activity. Those who are deficient are at an increased risk of bone marrow toxicity with this agent, as are patients who are taking allopurinol.
Other useful drugs in pemphigus erythematosus treatment are as follows:
-
Tetracycline and niacinamide [9]
-
Methotrexate [12]
-
Parenteral gold
-
Hydroxychloroquine
-
Plasmapheresis [13]
-
Mycophenolate mofetil [14]
-
Extracorporeal photochemotherapy
-
Rituximab
Dexamethasone-cyclophosphamide combination therapy has recently been studied. In 2009, Kandan and Thappa reported good outcomes in 65 cases of pemphigus treated with dexamethasone-cyclophosphamide pulse therapy. [19]
Pasricha and Poonam reported the effects of a few modifications in the regimen in 123 patients treated with the dexamethasone-cyclophosphamide pulse/dexamethasone pulse (DCP/DP) regimen over a period of 5 years (1998-2002). The 3 modifications introduced into the regimen were: (1) an additional daily dose of oral betamethasone sufficient to control the disease activity during phase I, which was progressively tapered completely as the patient recovered; (2) use of systemic antibiotics, if the patient had skin lesions, and oral anticandidal drugs, if the patient had oral ulcers, until complete healing; and (3) insistence on thorough cleaning of the skin and scalp, with a normal soap and shampoo, and proper maintenance of oral hygiene in spite of skin/mucosal lesions. The regimen consisted of DCP/DP repeated in exactly 28-day cycles, along with cyclophosphamide at 50 mg/d, insistence on completing treatment, and avoidance of irregular pulses in all patients. [20]
Cyclophosphamide is contraindicated in patients who wish to have children. [21]
Pawar and Singh pointed out that systemic steroid therapy can lead to increased fecal-oral shedding in Senear-Usher patients, thus raising the risk of viral disease transmission in these patients. [22]
Activity
Patients with pemphigus erythematosus should use appropriate sun-smart behaviors and protective clothing to minimize sun exposure that may exacerbate disease activity.
Diet
Patients on long-term glucocorticoid therapy should increase their intake of calcium and vitamin D, as well as engaging in weight-bearing activity. Dual-energy x-ray absorptiometry (DEXA) scanning and bisphosphates should be discussed with a rheumatologist.
Complications
The types of medications used to control severe pemphigus erythematosus may lead to serious iatrogenic disorders. Monitoring by a dermatologist is recommended if these medications are employed.
Etiology
Patients with pemphigus develop an autoimmune response directed against desmosomes. [23] In patients with pemphigus foliaceus and its variant, pemphigus erythematosus, the target antigen is desmoglein 1. Desmogleins are desmosomal proteins important in keratinocyte adhesion. The binding of autoantibodies is postulated to result in a cascade of biochemical intracellular events that eventuates in the loss of desmosome function. Additionally, certain HLA haplotypes (A10 or A26, DRW6) are thought to be associated, suggesting a genetic predisposition.
Relapse of pemphigus erythematosus has been associated with atorvastatin intake. [24]
A single new case of pemphigus erythematosus after treatment with topical ingenol mebutate has been described. [25]
Epidemiology
Frequency
The incidence of pemphigus is 0.5-3.2 cases per 100,000 population per year. Patients with pemphigus erythematosus comprise only a small subgroup of those with pemphigus. Kumar from India, in a 2008 article, reported a high prevalence (4.4 cases per million population). [26] However, in northern Finland, pemphigus foliaceus and pemphigus erythematosus are the most common pemphigus subtypes. [27]
Race
Pemphigus erythematosus, like other variants of pemphigus erythematosus and LE, may be increased in patients who express specific human leukocyte antigen (HLA) haplotypes. Those identified to have pemphigus erythematosus are positive for human leukocyte antigen A10 (HLA-A10) or human leukocyte antigen A26 (HLA-A26) and human leukocyte antigen DRW6 (HLA-DRW6).
Sex and age
Reports generally find no difference in occurrence of pemphigus erythematosus between the 2 sexes.
Pemphigus erythematosus may occur at any age, but it is unusual in children.
Prognosis
The prognosis of pemphigus erythematosus is better than that of pemphigus vulgaris. With good dermatologic care, patients with pemphigus erythematosus are often able to live normal lives. Some patients may ultimately develop symptoms classified as criteria for systemic lupus erythematosus (SLE) by the American College of Rheumatology (ACR).
Patient Education
Patient education about possible triggers for the pemphigus erythematosus is important. Patients should minimize sun exposure. Additionally, as in all photosensitive disorders, patient education on the use of sunscreens, protective clothing, and sun-smart behaviors is a cornerstone of therapy.
-
Direct immunofluorescence microscopy performed on epithelial biopsy specimen obtained from a patient with pemphigus vulgaris detects immunoglobulin G deposits at the epithelial cell surfaces.
-
Biopsy shows moderate epithelial hyperplasia with a suprabasal cleft that shows suprabasal acantholysis. The rest of the epithelium shows spongiosis with neutrophils. The submucosa has a moderately dense mixed perivascular infiltrate of lymphocytes and neutrophils. At places, the epithelium is missing, and the surface is covered by fibrin and necrotic inflammatory cells. Photo courtesy of Dr. Uday Khopkar.
-
Biopsy shows upper epidermal acantholytic blistering dermatitis involving the granular and upper spinous layer. The blister contains plasma, RBCs, and few acute inflammatory cells. The epidermis at the periphery of the blister shows mild spongiosis with neutrophils. In the roof of the blister, a few elongated acantholytic cells can be seen. Underlying dermis shows superficial and mid perivascular mixed infiltrate of neutrophils and lymphocytes. Photo courtesy of Dr. Uday Khopkar.
-
Biopsy shows upper epidermal acantholytic blistering dermatitis involving the granular and upper spinous layer with absence of roof of blister. The epidermis shows mild spongiosis with neutrophils. Underlying dermis shows superficial and mid perivascular mixed infiltrate of neutrophils and lymphocytes. Photo courtesy of Dr. Uday Khopkar.
-
Biopsy shows sparse superficial and deep perivascular infiltrate of lymphocytes. The papillary dermis is edematous and there is extravasation of RBCs. Basal layer shows vacuolization and interface infiltration by lymphocytes. Reticular dermis shows small amount of mucin. Photo courtesy of Dr. Uday Khopkar.






