Practice Essentials
Mammary Paget disease (PD) occurs almost exclusively in women; involvement of the male breast is rarely reported and may be more aggressive. [1, 2] Patients with PD frequently present with a chronic, eczematous rash on the nipple and adjacent areolar skin. Proper recognition of this disorder is required to initiate an appropriate workup (eg, skin biopsy) for differentiating it from other benign inflammatory dermatoses and for detecting an underlying breast carcinoma.
A similar disease involving the skin of female and male external genitalia (ie, vulva, glans penis) is known as extramammary Paget disease. [3] The histologic features of mammary PD and extramammary PD are similar; however, the histogenesis and the pathogenesis are different.
Signs and symptoms
Patients with mammary Paget disease (PD) present with a relatively long history of an eczematous skin lesion or persistent dermatitis in the nipple and adjacent areas. [4] Eczematous skin lesions are associated with several symptoms, including the following [5] :
-
Erythema
-
Scaling
-
Itching
-
Burning sensation
-
Ulceration
-
Oozing with serosanguineous discharge
-
Bleeding
-
Some combination of the above symptoms
Early symptoms and signs of mammary PD include the following:
-
Excoriation from itching
-
Resolution and recurrence of small vesicles within the skin lesion
Symptoms of pain, itching, and a burning sensation prompt patients to seek medical attention.
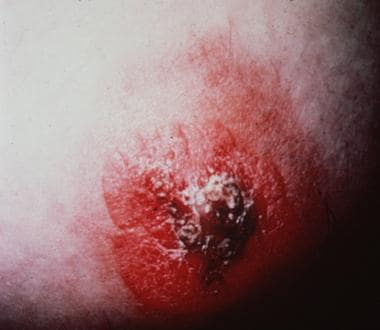
Scaly, erythematous, crusty, and thickened plaques on the nipple, spreading to the surrounding areolar areas, are typical (see the images below). Axillary PD can arise from underlying axillary accessory breast tissue. [6]
 Biopsy-proven Paget disease involving nipple of 56-year-old woman. Patient noted erythematous, swollen, enlarged nipple with focal ulceration and oozing; occasional serosanguineous discharge and bleeding were present. Patient was later found to have palpable breast mass and mammography results positive for subareolar microcalcification; no auxiliary lymphadenopathy was found. Patient was treated by simple mastectomy. At 5-year follow-up, she was alive, without recurrent or metastatic tumor.
Biopsy-proven Paget disease involving nipple of 56-year-old woman. Patient noted erythematous, swollen, enlarged nipple with focal ulceration and oozing; occasional serosanguineous discharge and bleeding were present. Patient was later found to have palpable breast mass and mammography results positive for subareolar microcalcification; no auxiliary lymphadenopathy was found. Patient was treated by simple mastectomy. At 5-year follow-up, she was alive, without recurrent or metastatic tumor.
 Mammary Paget disease (PD) affecting 48-year-old woman. Patient had experienced prolonged history of chronic eczematous dermatitis of nipple and areolar area for several years. Lesion did not respond to topical treatment, and it progressively distorted nipple with expansion into surrounding skin. Note markedly scaly, crusted, and deformed nipple with thickened, irregularly outlined adjacent nipple-areola complex. Excisional biopsy confirmed diagnosis of mammary PD. Patient developed infiltrating ductal carcinoma of underlying breast tissue with axillary lymph metastasis. She was treated by mastectomy and radiation. No metastatic tumor was noted in axillary lymph node. Patient was alive and well 3 years after treatment.
Mammary Paget disease (PD) affecting 48-year-old woman. Patient had experienced prolonged history of chronic eczematous dermatitis of nipple and areolar area for several years. Lesion did not respond to topical treatment, and it progressively distorted nipple with expansion into surrounding skin. Note markedly scaly, crusted, and deformed nipple with thickened, irregularly outlined adjacent nipple-areola complex. Excisional biopsy confirmed diagnosis of mammary PD. Patient developed infiltrating ductal carcinoma of underlying breast tissue with axillary lymph metastasis. She was treated by mastectomy and radiation. No metastatic tumor was noted in axillary lymph node. Patient was alive and well 3 years after treatment.
An erythematous patch in mammary PD is usually sharply demarcated and infiltrated (unlike eczematous dermatitis). Retraction of the nipple or the presence of palpable nodules indicates an underlying breast cancer. Serosanguineous discharge from the nipple may be present. Lesion size ranges from 3 mm to 15 cm in diameter; the mean size is 2.8 cm in diameter. Nipple invagination is sometimes seen (see the image below).
 Nipple invagination, deformed nipple-areola complex, marked erythema, and alternating hyperpigmentation and hypopigmentation noted in adjacent skin of breast in 65-year-old woman with biopsy-proven Paget disease. Note focal scaling of previous biopsy site. Nipple changes were associated with intraductal carcinoma of breast. Patient was treated by conservative excision of lesion and lumpectomy for in situ carcinoma. No recurrence or metastatic disease was noted at 6-year follow-up.
Nipple invagination, deformed nipple-areola complex, marked erythema, and alternating hyperpigmentation and hypopigmentation noted in adjacent skin of breast in 65-year-old woman with biopsy-proven Paget disease. Note focal scaling of previous biopsy site. Nipple changes were associated with intraductal carcinoma of breast. Patient was treated by conservative excision of lesion and lumpectomy for in situ carcinoma. No recurrence or metastatic disease was noted at 6-year follow-up.
Nipple changes are associated with an underlying carcinoma of the breast (ie, in situ, infiltrating ductal carcinoma) in more than 98% of patients; as many as two thirds of patients have a palpable breast tumor.
Unilateral involvement is the rule; however, bilateral mammary PD has occasionally been reported. [7] Rare cases of female patients with PD of supernumerary nipples have been reported. [8]
Pigmented mammary PD and pigmented extramammary PD are rare clinical entities in both males and females. These diseases may mimic malignant melanoma both clinically and histopathologically. [9] They may also mimic melanoma on dermatoscopic examination. [10] In pigmented lesions of PD, increased numbers of benign melanocytes are present, which may interfere with the correct diagnosis of PD, resulting in misinterpretation of this condition as malignant melanoma. [11]
Diagnostics
Sonographic abnormalities in the nipple-areolar complex may be evident. [12]
As this neoplasm may be multifocal and multicentric, MRI has been recommended to evaluate the true extent of disease. [13]
Mammography
Radiographic changes seen in mammary Paget disease (PD) include the following:
-
Subareolar microcalcifications (helpful in evaluating and locating clinically occult, nonpalpable underlying breast carcinoma)
-
Architectural distortion
-
Thickening of the nipple and the areola (reflecting edema)
-
Nipple changes (in a minority of patients)
About 50-70% of patients with biopsy-proven mammary PD show positive findings on mammography; image-guided biopsy is assisted by positive results on mammography.
Ninety-four percent of patients with biopsy-proven PD as the only physical finding had an underlying carcinoma, and nearly 60% had unifocal disease. However, negative preoperative mammography findings did not reliably exclude an underlying carcinoma. Statistical evidence suggests that in the setting of negative mammography findings, magnetic resonance imaging (MRI) of the involved breast can detect otherwise occult PD and thus facilitate treatment planning for patients with PD. [14]
Please see Workup for information on tissue analysis, histology, and staging.
Management
Also see Medication.
Mastectomy (radical or modified) and lymph node clearance are appropriate therapies for patients with mammary Paget disease (PD) with a palpable mass and underlying invasive breast carcinoma. [13, 15] As many as two thirds of patients are reported to have axillary lymph nodes positive for metastasis. Noninvasive breast carcinoma (in situ carcinoma) is found in about 65% of patients with mammary PD without a palpable mass.
Conservative management includes a combination of local excision of the nipple, wedge resection of the underlying breast, and radiation therapy. The number of patients treated by one or more conservative measures (eg, nipple excision and wedge excision of the underlying breast, cone excision, radiation therapy) is small. Breast conservation therapy with lumpectomy and radiation is an effective option, compared with mastectomy, for patients with Paget disease–ductal carcinoma in situ and Paget disease–invading ductal carcinoma. [16]
Patients who underwent cone excision and elective tamoxifen therapy had recurrences after an average follow-up of 4.6 years; some developed metastases. Therefore, cone excision is not sufficient therapy for patients with disease limited to the nipple.
Wide local excision with axillary node sampling is recommended for patients with or without a clinical mass.
Radiation therapy alone does not always control occult breast cancer; however, it may be used for patients who refuse mastectomy or those who are medically unfit for surgery.
Background
Sir James Paget first described Paget disease (PD) of the breast in 1874. He reported a chronic eczematous disease on the skin of the nipple and the areola in 15 women, with an associated intraductal carcinoma of the underlying mammary gland. In 1881, Thin illustrated the first histologic description of PD.
Pathophysiology and Etiology
The pathogenesis of mammary PD and the origin of Paget cells were once controversial. It is now widely accepted that mammary PD is always associated with an underlying carcinoma of the breast. By thorough histologic examination, Muir documented intraepidermal extension of malignant ductal epithelial cells through the lactiferous ducts and ductules into the epidermis (epidermotropism). [17] The findings are the basis of the epidermotropic theory of mammary PD.
Malignant epithelial (Paget) cells infiltrate and proliferate in the epidermis, causing thickening of the nipple and the areolar skin. These tumorous epithelial cells are derived from luminal lactiferous ductal epithelium of the breast tissue (see the image below).
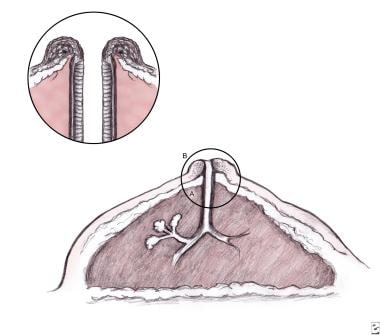 Schematic diagram of female breast depicting widely accepted concept of pathogenesis of mammary Paget disease. Malignant Paget cells are derived from luminal lactiferous ductal epithelium (A) of breast tissue with retrograde extension of cancerous Paget cells into epidermis of overlying nipple (B). Enlarged circle shows details that reveal thickening both of lining epithelium of breast duct and of nipple skin.
Schematic diagram of female breast depicting widely accepted concept of pathogenesis of mammary Paget disease. Malignant Paget cells are derived from luminal lactiferous ductal epithelium (A) of breast tissue with retrograde extension of cancerous Paget cells into epidermis of overlying nipple (B). Enlarged circle shows details that reveal thickening both of lining epithelium of breast duct and of nipple skin.
The cells possess microscopic features of glandular cells. Paget cells and underlying ductal carcinoma cells have been shown to be positive for the oncogene HER2/neu, suggesting common genetic alterations for both the epidermal and breast tumor cells.
It has been speculated that Paget cells may derive from glandular stem cells or epidermal Toker cells (clear cells of the nipple epithelium). [18, 19] Toker cells have been found in about 10% of normal nipples and rarely in supernumerary nipples on the mild line and apocrine bearing areas. [20] Like Paget cells of both mammary and extramammary sites, Toker cells contain prominent clear (vacuolated) cytoplasm, and they are considered benign counterparts of Paget cells.
Mammary Paget cells are malignant epithelial cells derived from underlying ductal adenocarcinoma of the breast that invade into the skin of nipple and areolar areas. Toker cells are benign and may sometimes proliferate, resulting in a condition known as clear cell papulosis. [20]
Kuan et al [21] reported on the immunohistochemical expression of apomucin MUC1, MUC2, and MUC5AC in PD and concluded that both epidermal Paget cells and underlying ductal carcinoma exhibit the same phenotypic apomucins that are also expressed by the Toker cells.
Morandi et al [22] reported that the chromosomal alterations seen in Paget cells (eg, loss of heterozygosity and mitochondrial DNA displacement loop sequence analysis) are different from those seen in underlying breast carcinoma cells. They suggested that the epidermal Paget cells are genetically different from those of breast carcinoma.
A concept of a “collision” between the neoplastic lesion of mammary PD and the underlying carcinoma is therefore presented. However, this concept is based on only a few cases. Further studies are necessary to arrive at a more definitive conclusion concerning collision lesions.
Paget cells often express cell markers that mimic those of the underlying breast carcinoma, including glandular epithelial cell markers (eg, low-molecular-weight cytokeratins or cellular adhesion molecule [CAM] 5.2).
They also express tumor markers, including carcinoembryonic antigen (CEA); Ca 15-3 (milk fat globule protein); oncogenes (TP53,c-erb B-2; about 85% of cases tested for c-erb B-2 are positive); and other cell markers, such as epithelial membrane antigen (EMA; all cases tested are EMA positive) and gross cystic disease fluid protein (GCDFP-15) found in tumor cells of ductal carcinoma of the breast.
Paget cells also share similar immunohistochemical characteristics with eccrine and apocrine sweat gland epithelium. Paget cells are periodic acid-Schiff (PAS) positive and diastase resistant; and they are Alcian blue positive at pH 2.5 in 32% and 18%, respectively.
Advances in immunohistochemistry further define the histogenesis of Paget cells. Cytokeratin 7 (CK7) has been proposed as a specific and nearly 100% sensitive marker for mammary PD; whereas cytokeratin 20 (CK20) is negative in mammary Paget cells, about 33% of cases of extramammary PD express this marker. However, there is a rare CK7-negative variant of Paget disease. [23] If in doubt, staining positive for GATA3 might be diagnostically beneficial.
The mechanism by which large neoplastic cells of glandular origin (ie, the Paget cells) infiltrate and spread to the overlying epidermal layers of the nipple and adjacent areola is induced by a mobility factor (heregulin-alpha) that acts through the HER2/neu receptor. [24]
Normal epidermal keratinocytes produce and release heregulin-alpha. This factor plays a significant role in the pathogenesis of PD. Paget cells express heregulin receptors HER2/neu and coreceptors HER3 and HER4. These receptor complexes on Paget cells bind heregulin-alpha, the mobility factor, resulting in the chemotaxis of breast ductal carcinoma cells. This process, in turn, causes migration and infiltration of Paget cells into the overlying epidermis of the nipple and the areolar skin.
Molecular studies have shown that abnormal plakoglobin (one of the cell-to-cell adhesion proteins) may be involved in the formation of some cases of PD of the breast and the vulva; and reduced expression of E-cadherin (another cell-cell adhesion protein) may have a role in the pathogenesis of extramammary PD. [25]
Epidemiology
In the United States, about 1-4% of female breast carcinoma cases are associated with PD of the nipple, the areola, and the surrounding skin; nearly 100% of mammary PD cases are associated with an underlying carcinoma, either in situ (intraductal, 10%) or infiltrating cancer (90%). Occasional cases of PD have been reported in ectopic breast or supernumerary nipples. [26] Worldwide, the exact frequency of mammary PD is unclear. Chinese female mammary PD patients tend to be much younger, with a lower prevalence than that in the United States. [27]
In female patients with mammary PD, ages range from 24 to 84 years, with a mean age at diagnosis of 55 years; the average age range is 53-59 years. The average patient age is 5-10 years older for patients with mammary PD than for individuals with breast carcinoma. The age of onset in male patients is generally in the fifth and sixth decades, with a range of 48-80 years. Only 1.65% of mammary PD is seen in men. [28]
Mammary PD occurs almost exclusively in females; PD of the male breast is extremely rare. The estimated occurrence of male breast carcinoma is only 1% of the rate in females. A rare case of PD in the male breast was recorded after treatment of a prostate carcinoma with estrogen. No racial predisposition is reported for mammary PD.
Prognosis
The prognosis for patients with mammary PD is related to disease stage and appears to be similar to that of women with other types of breast cancer. Patients with mammary PD first seen with underlying ductal carcinoma in situ or invasive breast carcinoma were found to have aggressive tumor characteristics and worse survival outcomes. [29] PD was identified as an independent unfavorable risk factor for breast cancer survival.
Survival is related to the presence or the absence of a palpable breast tumor. When present, the prognosis is the poorest. [30] In one study, 31 (62%) of 50 patients with mammary PD presented with a detectable breast mass.
One half (50%) of patients with PD presenting with a palpable breast mass have associated axillary lymph node metastasis. Two thirds of patients with axillary node metastasis were reported to have a palpable breast mass, whereas one third of patients with axillary metastasis did not have a palpable mass.
Even in patients with mammary PD and no underlying tumor, 30% may develop an invasive carcinoma at a later date, and 20% of patients already have an associated in situ carcinoma of the breast. However, other reports indicate that no axillary metastases were detected in patients without a palpable breast mass.
Patients with an identifiable associated underlying breast tumor have a survival rate of 38-40% at 5 years and a survival rate of 22-33% at 10 years. The death rate for metastatic breast carcinoma in patients with mammary PD and underlying cancer is 61.3%, with a 10-year cumulative survival rate of 33%.
The reported survival rate of patients with PD without a palpable breast tumor (prior to surgery) ranges from 92% to 94% at 5 years and from 82% to 91% at 10 years.
Mastectomy is the standard treatment of mammary Paget disease. Conservative treatment with preservation of the nipple-areola complex results in a higher rate of recurrence than treatment by mastectomy.
A small number of patients with mammary PD who did not have a palpable breast mass and who had a negative mammogram underwent conservative excision of the involved nipple-areola with a wedge resection of the underlying breast tissue and remained disease free at 10-year follow-up.
Rare cases of recurrent mammary PD have been reported in patients who underwent partial nipple excision; however, no patient developed breast parenchymal recurrence at a mean follow-up of 36 months.
In a study of patients with mammary PD (without clinical or mammographic evidence of breast tumor) who were treated with radiation therapy alone or excision plus radiation, 3 of 20 patients developed recurrent disease in the nipple-areola at a mean follow-up of 7.5 years. Those patients eventually underwent a mastectomy.
According to Osteen, [31] 9 (11.4%) of 79 patients treated by local excision (with or without radiation therapy) developed recurrences.
Patient Education
Patients should be informed that PD of the nipple-areola complex is a rare form of breast cancer that is clinically characterized by eczematous changes in the nipple. Clinical symptoms include erythema, itching, a burning sensation, thickening of the skin, inversion of the nipple, and sometimes a bloody nipple discharge. Usually, symptoms are present for 6 months or more before the detection of an underlying breast cancer. A biopsy should promptly be performed on all suspicious lesions of the nipple area for accurate diagnosis and treatment.
Failure to educate patients about the potential for invasive breast carcinoma associated with mammary PD is a pitfall; without this knowledge, patients may delay further diagnostic mammography examination and possibly delay detection of an underlying breast cancer.
-
Schematic diagram of female breast depicting widely accepted concept of pathogenesis of mammary Paget disease. Malignant Paget cells are derived from luminal lactiferous ductal epithelium (A) of breast tissue with retrograde extension of cancerous Paget cells into epidermis of overlying nipple (B). Enlarged circle shows details that reveal thickening both of lining epithelium of breast duct and of nipple skin.
-
Biopsy-proven Paget disease involving nipple of 56-year-old woman. Patient noted erythematous, swollen, enlarged nipple with focal ulceration and oozing; occasional serosanguineous discharge and bleeding were present. Patient was later found to have palpable breast mass and mammography results positive for subareolar microcalcification; no auxiliary lymphadenopathy was found. Patient was treated by simple mastectomy. At 5-year follow-up, she was alive, without recurrent or metastatic tumor.
-
Mammary Paget disease (PD) affecting 48-year-old woman. Patient had experienced prolonged history of chronic eczematous dermatitis of nipple and areolar area for several years. Lesion did not respond to topical treatment, and it progressively distorted nipple with expansion into surrounding skin. Note markedly scaly, crusted, and deformed nipple with thickened, irregularly outlined adjacent nipple-areola complex. Excisional biopsy confirmed diagnosis of mammary PD. Patient developed infiltrating ductal carcinoma of underlying breast tissue with axillary lymph metastasis. She was treated by mastectomy and radiation. No metastatic tumor was noted in axillary lymph node. Patient was alive and well 3 years after treatment.
-
Nipple invagination, deformed nipple-areola complex, marked erythema, and alternating hyperpigmentation and hypopigmentation noted in adjacent skin of breast in 65-year-old woman with biopsy-proven Paget disease. Note focal scaling of previous biopsy site. Nipple changes were associated with intraductal carcinoma of breast. Patient was treated by conservative excision of lesion and lumpectomy for in situ carcinoma. No recurrence or metastatic disease was noted at 6-year follow-up.
-
Photomicrograph of malignant melanoma in situ of skin displays prominent intraepidermal pagetoid spread. Note that melanoma cells are present in all layers of epidermis, mostly in single units. Cytoplasm of melanoma cells is vacuolated. Moderate upper dermal chronic inflammatory infiltrate is present (hematoxylin-eosin, original magnification ×250). S-100 protein and homatropine methylbromide immunostains are positive in melanoma cells, whereas carcinoembryonic antigen is negative. No epithelial mucin is seen in these tumor cells.
-
Photomicrograph of mammary Paget disease lesion. Note nests of malignant Paget cells predominantly involving lower layers of epidermis. Cytoplasm of tumor cells contains abundant pale-staining, granular, mucinous material. Occasional small glandular structures can be seen within malignant cell nests (hematoxylin-eosin, ×100).
-
Composite photomicrograph of mammary Paget disease depicting nests, islands, and individual tumor cells in epidermis (left; hematoxylin-eosin, ×250), along with tumor cells stained positive for carcinoembryonic antigen (CEA) (right; immunostain with anti-CEA, ×250).
-
Low-power view of transmission electron micrograph displaying malignant Paget cells in lower layer of epidermis. Note large Paget cell containing ovoid nucleus (N), scanty nuclear chromatin, large nucleolus, and abundant pale-staining cytoplasm with smooth and rough endoplasmic reticulum (arrow), scattered enlarged mitochondria, free ribosomes, and lysosomes. No desmosomal attachments are seen between Paget cells and adjacent keratinocytes. Tonofilaments are seen in keratinocytes (uranyl acetate and lead citrate, ×5,500).
-
Cytoplasm of malignant Paget cell is packed with numerous rounded, membrane-bound mucin granules with various electron densities (uranyl acetate and lead citrate, ×12,000.)
-
Photomicrograph of intraductal carcinoma of breast underneath Paget disease of nipple in 56-year-old woman. Note expansion of ductal lumen, which is filled with irregularly sized tumor cells of ductal epithelial origin. Nuclear hyperchromatism and gland-in-gland (cribriform) pattern are evident. Tumor was detected by positive mammogram result depicting focus of microcalcification beneath nipple.







