Background
Melanocytic nevi are benign neoplasms or hamartomas composed of melanocytes, [1] the pigment-producing cells that constitutively colonize the epidermis. Melanocytes are derived from the neural crest and migrate during embryogenesis to selected ectodermal sites (primarily the skin and the CNS), but also to the eyes and the ears. Ectopic melanocytes have been identified at autopsy in the gastrointestinal and genitourinary tracts. Congenital melanocytic nevi are thought to represent an anomaly in embryogenesis and, as such, could be considered, at least in a sense, malformations or hamartomas. [2] In contrast, most acquired melanocytic nevi are considered benign neoplasms. Compare the images below. Melanocytic nevi occur in all mammalian species and are especially common in humans, dogs, and horses.
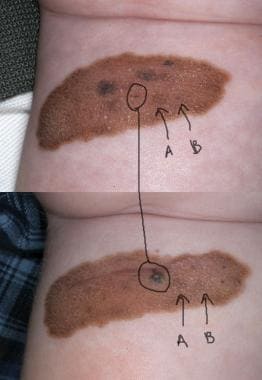 This large congenital nevus developed papular areas of pigmentation within it. Microscopic examination proved that the "new" areas represented small nodular collections of benign melanocytes, with no evidence of evolving melanoma.
This large congenital nevus developed papular areas of pigmentation within it. Microscopic examination proved that the "new" areas represented small nodular collections of benign melanocytes, with no evidence of evolving melanoma.
See Can You Recognize Benign Skin Lesions From Cancerous Ones?, a Critical Images slideshow, to help correctly identify various lesions.
The malignant analogue of a melanocytic nevus is melanoma, a topic discussed independently in Malignant Melanoma. Additionally, the Medscape Skin Cancer Resource Center may be helpful.
Pathophysiology
Melanocytes are present in the basal layer of the epidermis and exhibit a certain degree of territoriality. Non-neoplastic melanocytes typically exhibit contact inhibition to each other, and thus pigment cells are usually not found as contiguous cells. With certain forms of stimulation, such as the exogenous administration of ultraviolet irradiation, the density of melanocytes in normal epithelium may increase. Normal melanocytes may also involve adnexal epithelium, most notably the bulbs of follicular papillae.
Melanocytic nevi represent proliferations of melanocytes that are in contact with each other, forming small collections of cells known as nests. Melanocytic nevi commonly form during early childhood. Their onset is believed by some authorities to be, at least in part, a response to sun (ultraviolet) exposure. However, genetic factors are also clearly involved in the development of some types of melanocytic nevi. Some kinships express an autosomal dominant condition (the so-called dysplastic nevus syndrome or the familial atypical multiple mole and melanoma syndrome), in which members have a large number of large nevi, sometimes hundreds, scattered over the integument.
Melanocytic nevi have also been observed to develop or spread rapidly after blistering events, such as second-degree thermal burns, severe sunburns, or toxic epidermal necrolysis or in persons with genetic blistering diseases such as epidermolysis bullosa. In such instances, the development of so-called eruptive melanocytic nevi appears to be propagated by a traumatic stimulus, with scattering of melanocytic nevus cells over a large area within a zone of blistering and with the subsequent development of multiple independent melanocytic nevi within the injured area. Growth factors, such as basic fibroblast growth factor, have been suggested to be released by proliferating keratinocytes and could contribute to stimulation of melanocyte proliferation in this context. In summary, the exact etiology behind the development of melanocytic nevi is complex and multifactorial and is incompletely understood.
Acquired melanocytic nevi are considered benign neoplasms. In contrast, congenital melanocytic nevi are perhaps best interpreted as congenital malformations. Melanocytes are of neural crest origin, and congenital nevi probably represent an error in the development and migration of these neuroectodermal elements. Evidence of errant embryological migration can be seen histopathologically within giant congenital melanocytic nevi. In this context, melanocytes may be found distributed throughout the dermis, around and within the walls of blood vessels, around adnexal structures such as hair follicles, within the subcutis, and sometimes within skeletal muscle, smooth muscle bundles, nerves, or sebaceous glands.
Errant embryological migration is also believed to be the source of melanocytic nevus cell "rests," which can be observed in the capsules of lymph nodes. Occasionally, rests of melanocytes can also be found in the subcapsular space or within lymph node trabecula. The importance of melanocytic nevus rests is that they can sometimes be mistaken for metastatic deposits because of their extracutaneous location.
These rests are not uncommonly associated with agminated blue or cellular blue nevi or with large congenital melanocytic nevi. However, with the advent of sentinel node evaluation, nodal rests of melanocytic nevi clearly are not uncommon and can be found in association with a variety of melanocytic and nonmelanocytic lesions. These rests of cells are sometimes referred to as benign metastases because these cell clusters may represent the end result of an intralymphatic migration of benign melanocytes. Note, however, that benign nodal melanocytic nevi are almost invariably within the capsule, while melanoma metastases are commonly subcapsular.
Etiology
The etiology of melanocytic nevi remains unknown. No established genetic or environmental influences are known to contribute to the development of congenital nevi. However, after studying 144 children in Naples, researchers concluded that development of melanocytic nevi early in life is the result of complicated relationships among nevus evolution, anatomic location, and environmental and constitutional factors. [3] The specific genetic factors that contribute to the development of acquired melanocytic nevi also remain unknown. However, data suggest that the propensity for developing large numbers of nevi, such as multiple dysplastic nevi, might be inherited as an autosomal dominant trait.
Patients with the familial atypical multiple mole and melanoma syndrome (also known as the dysplastic nevus syndrome) develop dozens to hundreds of melanocytic nevi and have an elevated lifetime risk for the development of melanoma. As the name implies, this disorder is believed to have an inherited basis.
As noted previously, population-based evidence suggests that ultraviolet irradiation may trigger the development of acquired melanocytic nevi. The number of melanocytic nevi in childhood is inversely related to the degree of skin pigmentation and is high in children with poor sun tolerance. The mechanism of this induction has not been adequately investigated, but such induction could represent an example of tumor promotion by ultraviolet light.
Epidemiology
Frequency
United States
Acquired melanocytic nevi are so common that some authorities believe they cannot be considered a defect or an abnormality. However, despite the high prevalence, melanocytic nevi are nonetheless pathologic in the sense that they represent an aberrant or neoplastic proliferation of cells. Most persons with light skin have at least a few melanocytic nevi. [4] Melanocytic nevi also occur in dark-skinned individuals, albeit with low prevalence. Interestingly, there are distribution differences in melanocytic nevi between light-skinned and dark-skinned individuals. In light-skinned individuals, most melanocytic nevi occur on the trunk. In dark-skinned individuals, acral melanocytic nevi are relatively more common. [5]
International
The international prevalence of melanocytic nevi is believed to be similar to that observed in the United States. The prevalence in ethnic groups with dark skin is lower than that observed in individuals with fair skin. If ultraviolet exposure represents an inducing agent for the development of melanocytic nevi, than this is unsurprising. Some individuals of northern European extraction, especially those from northern Germany, Holland, Belgium, and the United Kingdom, not uncommonly have large nevi (≥ 1 cm in largest diameter), often of large number (>50, up to several hundred), with a red-brown color. These nevi have been called atypical moles or dysplastic nevi.
Race
Melanocytic nevi are common lesions in patients with light or fair skin and are less common lesions in dark-skinned individuals. This difference in prevalence is in part attributable to the fact that identifying moles in dark-skinned patients is often difficult, especially if the lesions are macular (flat).
Some authorities have suggested that melanocytic nevi are in part stimulated by exposure to sunlight. [6, 7] If so, then individuals with dark skin might have fewer nevi because of the protective properties of melanin.
Evidence indicates that broad-spectrum sunscreens attenuate the development/evolution of melanocytic nevi when used in children [8] ; therefore, dark-skinned individuals probably have inherent protection against the development of moles because of their cutaneous melanization.
Sex
No clear sex predilection is reported for the development of melanocytic nevi. However, melanocytes have been postulated to exhibit some degree of sex hormone responsiveness. The findings associated with melanocytic nevi during pregnancy support this conclusion. Melanocytic nevi commonly darken and/or enlarge during pregnancy. Melanocytes have been shown to have cytosolic receptors for estrogens and androgens, and melanogenesis is responsive to these steroid hormones. Some melanomas seem to respond to hormones, an observation that might be explained by these cytosolic receptors.
Subtle differences may exist in the prevalence of melanocytic nevi between women and men. Judging the incidence and prevalence based on available biopsy data is difficult because women may be more likely to seek medical attention. If sex-specific variations in incidence do exist, the differences may be site specific. For example, specific histopathological features are commonly observed in melanocytic nevi that occur within genital skin. These features are noted almost exclusively within biopsy specimens from women, although similar alterations can occasionally be observed in melanocytic nevi from males.
From the author's database (at the University of California, San Francisco), data clearly show that biopsies of genital melanocytic nevi are much more commonly performed in women than in men. These data do not unequivocally confirm that the prevalence of genital melanocytic nevi is truly increased in women, although this seems likely.
Age
By definition, congenital melanocytic nevi are present at birth or soon thereafter, although some small congenital nevi are clearly tardive in their clinical presentation. Current opinion holds that some elements of such nevi are present at birth but remain inconspicuous until some later date.
By definition, acquired melanocytic nevi are not present at birth, and the incidence of melanocytic nevi increases throughout the first 3 decades of life.
The peak incidence of melanocytic nevi is in the fourth to fifth decades of life, and the incidence with each successive decade decreases, with a low incidence in elderly persons.
Acquired melanocytic nevi have been stated to be absent at birth and at death. Although not entirely true, this concept reflects the fact that acquired nevi develop in increasing numbers throughout childhood and early adulthood and then slowly involute; therefore, melanocytic nevi are inconspicuous during the advanced elder years.
Nevus subtype incidence may also vary with ages. According to a study by Zalaudek et al, melanocytic nevi of mixed pattern with a peripheral rim of dark globules are sufficiently rare in persons older than 50 years that they should be considered suspicious. [9]
Prognosis
The prognosis associated with any single melanocytic nevus is favorable because these lesions are benign neoplasms with no potential for malignant behavior, unless evolution of melanoma occurs. Patients with multiple melanocytic nevi or sizable melanocytic nevi appear to have an increased lifetime risk of melanoma, with the risk increasing in rough proportion to the size and/or number of lesions.
Melanocytic nevi, if diagnosed properly, are biologically stable, completely benign lesions. However, melanocytic nevi can be found in association with melanoma. [10] The true frequency of transformation of a melanocytic nevus into melanoma is not known, and the estimated prevalence varies widely in published series, with some data suggesting that up to 40% of melanomas are associated with a precursor melanocytic nevus.
Both acquired and congenital melanocytic nevi hold some risk for the development of melanoma. Congenital melanocytic nevi hold the greater risk, and this is especially true of giant congenital melanocytic nevi. This is believed to be a consequence of the fact that the number of lesional melanocytes within large lesions is greater, and thus the chances of a transformative event are proportionately greater. Large and giant congenital melanocytic nevi often have both biological and cosmetic implications. Large congenital nevi have a low but real risk for secondary malignant transformation and the development of melanoma. Some data suggest that melanoma can develop within a giant congenital melanocytic nevus in up to 5% of cases.
Patient Education
Patients should be educated regarding self-examination of melanocytic nevi. Teach patients to use an ABCDE approach, in which the patient assesses the asymmetry, border irregularity, color, diameter (size), and evolution of any given lesion. Some authorities add an F for "funny looking," suggesting that "ugly duckling" lesions that differ from the patient's other nevi should be evaluated. An explanation of any changes and observations for changes are important. Nevi can change in diameter, outline, and/or color, and they can acquire an itch or begin to bleed. These changes require evaluation by a trained observer to determine the malignant potential of a lesion.
Patient handouts that illustrate these changes and their significance are available from the American Academy of Dermatology. The greater the degree of asymmetry, the greater the irregularity in the border, the greater the variation in color, and the greater the diameter of the lesion, the more cause for concern.
The need for adequate sun protection and should be emphasized to adults and children. [11]
For patient education resources, see the patient education article Mole Removal.
-
A Clark (dysplastic) nevus with modest variation in pigmentation and irregular borders. Biopsy of the lesion proved no evidence of melanoma.
-
A compound Clark (dysplastic) nevus with fried egg–like clinical morphology, with a central dark papule flanked by an eccentric more lightly pigmented macular zone.
-
A conventional (papular) melanocytic nevus occurring within acral skin. Note slight border irregularity, a feature common in association with acral nevi.
-
A heavily pigmented junctional Spitz nevus, also known as pigmented spindle cell nevus. Note that many Spitz nevi are nonpigmented and may have an angiomalike clinical appearance.
-
A melanocytic nevus occurring within conjunctival epithelium.
-
A conventional compound melanocytic nevus. Note the presence of melanocytes with small nuclei in nests along the dermoepidermal junction and the presence of similar melanocytes in nests and syncytia in the subjacent dermis.
-
This Spitz nevus shows large melanocytes with spindled and epithelioid cytomorphology arrayed along the junctional zone of an acanthotic and hyperkeratotic epithelium.
-
At higher magnification, this Spitz nevus also demonstrates large, dull-pink globules along the junctional zone. These structures are known as Kamino bodies. Kamino bodies are most commonly observed in association with Spitz nevi but are occasionally observed in melanocytic nevi of other types. Well-formed Kamino bodies are almost never (if ever) found in association with melanoma.
-
This blue nevus is composed of small dendritic melanocytes. This type of cytomorphology can be seen in so-called common blue nevi and in topographically restricted lesions such as nevus of Ito or nevus of Ota.
-
This large congenital nevus developed papular areas of pigmentation within it. Microscopic examination proved that the "new" areas represented small nodular collections of benign melanocytes, with no evidence of evolving melanoma.
-
Histopathologically, a congenital nevus differs from an acquired melanocytic nevus in that melanocytes are often distributed deeply within the reticular dermis, within the adventitial dermis around adnexal elements, and sometimes within the subcutis. This congenital nevus shows a folliculocentric array of melanocytes.







