Overview
The widely used acronym ABCDE (asymmetry, irregular borders, multiple colors, diameter >6 mm, enlarging lesion) contains the primary clinical criteria for diagnosing suspected cutaneous malignant melanoma. The early phase of malignant melanoma is difficult to identify because cutaneous malignant melanoma can share many clinical features with an atypical nevus. Several studies have described diagnostic accuracy rates ranging from 50-75%, indicating a need for additional diagnostic tools. The introduction of dermoscopy, also termed epiluminescence microscopy (ELM), has opened a new dimension in the examination of pigmented skin lesions and, especially, in the identification of the early phase of cutaneous malignant melanoma.
Dermoscopy is a noninvasive method that allows the in vivo evaluation of colors and microstructures of the epidermis, the dermoepidermal junction, and the papillary dermis not visible to the naked eye. These structures are specifically correlated to histologic features. The identification of specific diagnostic patterns related to the distribution of colors and dermoscopy structures can better suggest a malignant or benign pigmented skin lesion. The use of this technique provides a valuable aid in diagnosing pigmented skin lesions. Because of the complexity involved, this methodology is reserved for experienced clinicians.
Vestergaard et al have reported dermoscopy assessment is more accurate than clinical evaluation by naked eye for the diagnosis of cutaneous melanoma (odds ratio = 15.6, P = .016). In this study, the mean sensitivity in the diagnosis of melanoma was 74% for the examination by naked eye and 90% for dermoscopy.
The equipment; technologic methods; diagnostic features; and primary aspects of melanoma, common nevi, atypical nevi, and other nonmelanocytic pigmented skin lesions are discussed in this article. The technique is also commonly used to assist in the evaluation of nail fold capillaries and features of alopecia. [1, 2]
Technical Procedures and Equipment
Dermoscopy involves an evaluation of the skin surface. During a dermoscopy assessment, the pigmented skin lesion is typically covered with a liquid (usually oil or alcohol) and examined under a specific optical system. Applying oil reduces the reflectivity of the skin and enhances the transparency of the stratum corneum. This allows visualization of specific structures related to the epidermis, the dermoepidermal junction, and the papillary dermis, and it also suggests the location and distribution of melanin. Some newer instruments use techniques such as polarization to reduce the need for a liquid interface. [3]
Dermatoscope
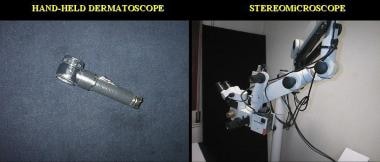
The dermatoscope, shown in the image below, is the simplest and best-recognized piece of equipment used to perform a dermoscopy examination. It is similar to an otoscope, is user friendly, and is inexpensive. This optical system's features include monocular observation, magnification X10, and the use of an illumination system (3.5-V halogen lamp).
Stereomicroscope
Another optical instrument, the stereomicroscope, shown in the image above, allows an accurate binocular observation with different magnifications (X6-80). The illumination system includes a halogen lamp (12 V/50 W). The stereomicroscope is expensive, is large and bulky, and is only available in a few centers.
From an empiric point of view, visualization is better than with the dermatoscope, but formal studies of the differences in diagnostic features and accuracy of the 2 instruments have never been published.
Videodermatoscope
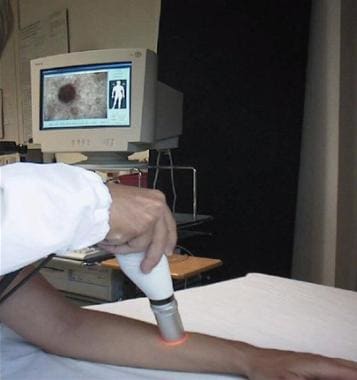
Features of another optical system, the videodermatoscope (shown below), include a polarized or nonpolarized video probe that transmits images of the skin lesion to a color monitor.
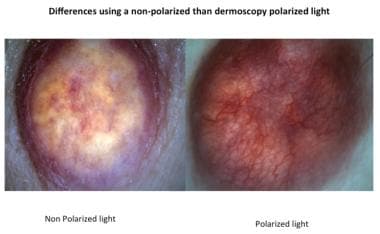
More subtle differences are visible on dermoscopy structures and colors using a dermoscopy with nonpolarized than polarized light. The polarized system allows a better visualization of vessels and red areas. Nonpolarized dermoscopy requires the application of a liquid or a gel in the interface between the instrument and the skin surface. Furthermore, the study of vascular pattern may be compromised by excessive pressure of the instrument resulting in compression of vessels. Thus, vascular patterns cannot properly be examined in their real shape. On the other hand, structures such as pseudocysts, multiple gray-blue dots and blue-white veil are more accurately evaluated by not polarized dermoscopy.
The addition of a digital system to the stereomicroscope, also termed the digital epiluminescence microscope (see the image below), and/or to the videodermatoscope has opened a new area of development with the advantages of computerized technology. However, the technologic features (which are cost dependent) of the camera (single-chip video charge-coupled device, 3-chip charge-coupled device, or still digital; see the image below), optical system, monitor, digitized board, and software can influence the resolution and quality of the images. These features can strongly influence the evaluation of a pigmented skin lesion; a low-resolution instrument may prevent accurate diagnosis.
 Digital epiluminescence microscopy equipment, Skin Cancer Unit, Centro Prevenzione Oncologica, Ravenna, Italy.
Digital epiluminescence microscopy equipment, Skin Cancer Unit, Centro Prevenzione Oncologica, Ravenna, Italy.
Dynamic optical coherence tomography (D-OCT)
D-OCT is a noninvasive imaging modality that can cellular structure motion with nanometer sensitivity and micrometer resolution. Studies have demonstrated the usefulness of D-OCT in distinguishing benign nevi and malignant melanoma based on the lesions' microvascular features. [4]
Color
Accurate evaluations of the color of a pigmented skin lesion, the degree of pigmentation, and the distribution of the colors within the lesion are the most important elements of a dermoscopy examination. The epidermis usually appears white, but acanthosis results in a grayish-brown or brownish-yellow color. Melanin is the most important pigment in determining different structural and chromatic patterns. The pigmented skin lesion can have a different degree and distribution of pigmentation depending on the location of melanin in different layers of the skin.
Melanin location and lesion color
See the list below:
-
Upper epidermis (stratum corneum, stratum spinosum) - Black
-
Dermoepidermal junction - Light-to-dark brown
-
Papillary dermis - Slate blue
-
Reticular dermis - Steel blue
Other possible colors include various shades of white and red. White shades are related to regression and may be seen with melanomas, benign melanocytic nevi (halo nevus), and nonmelanocytic lesions (lichenoid keratosis, scars). Red shades are related to increased vascularization in tumors, an increased number of capillary vessels, and bleeding within the lesion. If bleeding persists and crust develops, the color ranges from red-black to blue-black. A good evaluation of colors and their relative distribution is essential for achieving the correct clinical diagnosis of a pigmented skin lesion.
On multispectral dermoscopy, a study showed that deep pigmentation in cutaneous melanomas was associated with significantly greater Breslow thickness. [5]
Guide Criteria
ELM features can be divided into primary and secondary guide criteria, which show numerous different manifestations related to chromatic and geometric variables (eg, distribution, width, caliber); these are discussed in detail in the description of each ELM feature.
Primary criteria
Pigment network
The most important ELM feature of melanocytic lesions is the pigment network (PN), which consists of pigmented network lines and hypopigmented holes. This feature is correlated histologically to the length of the rete ridges and to the distribution of melanin within the keratinocytes of the epidermal rete ridges. The network of hypopigmented holes corresponds to the suprapapillary plate, which is relatively thin and contains less melanin. The network lines correspond to the rete ridges, which are thicker and have a greater quantity of melanin.
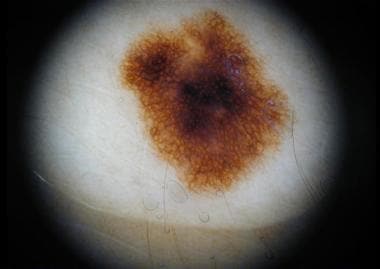
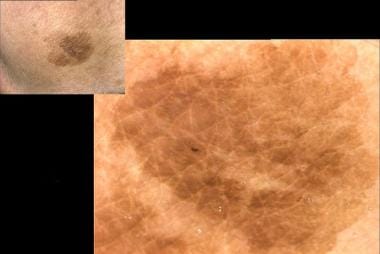
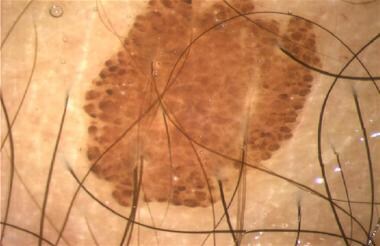
In melanocytic nevi, the PN is slightly pigmented. Light-brown network lines are thin and fade gradually at the periphery. Holes are regular and narrow (see the images below).
The distribution is symmetric and sometimes accentuated in the center of the lesion (see the images below).
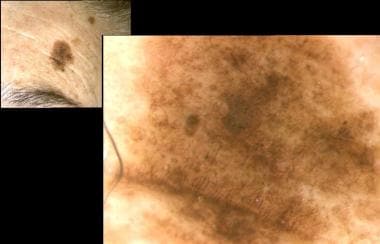
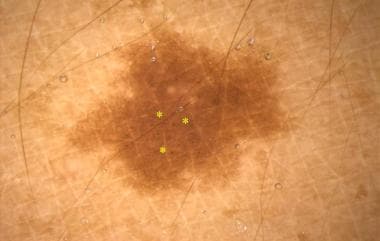
In melanoma, the PN usually ends abruptly at the periphery and has irregular holes, thickened and darkened network lines, and treelike branching at the periphery (see the image below).
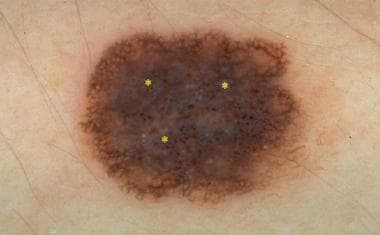
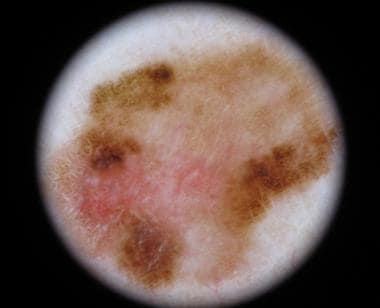
 In situ melanoma with asymmetric color distribution, irregular pigment network, and a whitish veil (*).
In situ melanoma with asymmetric color distribution, irregular pigment network, and a whitish veil (*).
In cutaneous malignant melanoma, the PN features change between bordering regions. Some areas of malignant lesions manifest as a broad and prominent PN, while others have a discrete irregular PN. The PN also may be absent in some areas (see the image below).
 In situ melanoma with asymmetric color distribution, irregular pigment network, and pigment dots with varied size (*).
In situ melanoma with asymmetric color distribution, irregular pigment network, and pigment dots with varied size (*).
Atypical nevi (dysplastic nevi) are difficult to diagnose at times because they may show areas of irregular and discrete PN distributed asymmetrically (see the image below).
Pseudopigmented network
ELM features of homogeneous pigmentation of the face (interrupted by hypopigmented hair follicles and hypopigmented sweat gland openings) create a pseudopigmented network. In benign lesions, this pseudonetwork tends to be uniform and symmetric in color and pattern. In contrast, in lentigo maligna and lentigo maligna melanoma, the pseudonetwork becomes nonuniform and asymmetric in color and pattern because of the increased number of atypical melanocytes extending down hair follicles and adnexal structures. The meshes become broader, and the holes are larger. Note the images below.
Radial streaming and pseudopods
Radial streaming and pseudopods are different morphologic expressions of malignant melanoma, specifically melanoma in the radial growth phase. Radial streaming (see the image below) is a linear extension of pigment at the periphery of a lesion, often appearing in groups of nearly parallel, radially arranged linear structures.
Depth determines the colors, which are brown, dark brown, blue-gray, and black. Pseudopods (see the image below) are curved fingerlike projections that are predominantly dark brown or black and are located at the periphery of a lesion. They occasionally have small knobs at their tips. Radial streaming and pseudopods histologically correspond to confluent junctional nests of atypical melanocytes.
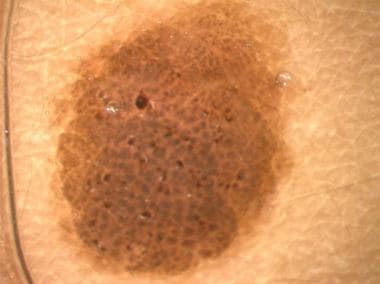
Pigmented globules
Pigmented globules are round or oval, dark brown or black, and larger than 1 mm in diameter. They are uniform in pigmented skin lesions but vary in size, color, and shape in atypical nevi and melanoma. When abundant, aggregated globules have a cobblestone pattern, which is typical of benign melanocytic lesions. See the images below.
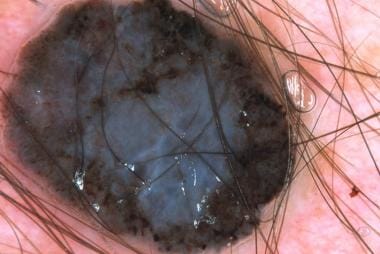
In cutaneous malignant melanoma, globules are dark or slate blue and are distributed irregularly (see the image below). Occasionally, isolated dark globules are seen at the margins of an achromic lesion; in this case, a diagnosis of melanoma is suggested.
Pigmented globules correspond histologically to nests of pigmented melanocytes (nevus or melanoma) at the junction in the papillary dermis or, because of melanin storage, in melanophage clusters in the papillary dermis. Milky-red globules can be seen in cutaneous malignant melanoma, representing melanoma cell nests with increased vascularization.
Secondary criteria
Pigmented dots
Pigmented dots are small, round or irregularly shaped pinpoint structures that are black or dark brown. They correspond to focal accumulations of free melanin or an increased number of highly pigmented melanocytes in the cornified layers of the epidermis.
The presence of melanophages and/or atypical melanocytes in the dermis correlates with blue-gray or slate blue dots and is typically found in pigmented melanocytic and nonmelanocytic lesions undergoing regression. Vertical capillaries found on apical dermal papillae appear as red dots on the palms and soles; sweat gland openings appear as white dots. In benign melanocytic lesions, dots in the center of the lesion are homogeneous in color and are regular in size, shape, and distribution. In cutaneous malignant melanoma or in atypical lesions, dots may occur at the periphery of the lesion and are irregular in size, shape, and distribution. See the images below.
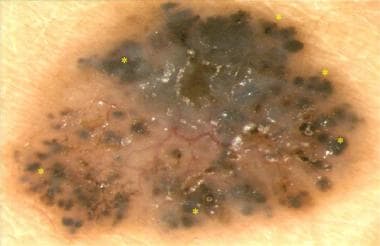
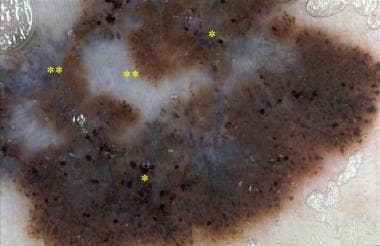 Invasive melanoma with white and gray areas (**), different expressions of pigmented dots (*), and globules (O).
Invasive melanoma with white and gray areas (**), different expressions of pigmented dots (*), and globules (O).
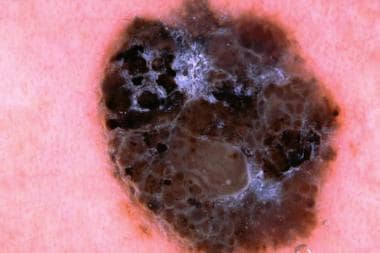
Blue-white veil
A blue-white veil is a ground-glass area of pigmentation that is blue-gray to blue-white in color. This ELM feature is present in homogeneously pigmented black or dark brown lesions and is associated with thickening of the epidermis (see images below). It is correlated histologically with compact orthokeratosis and hypergranulosis, with confluent nests of heavily pigmented melanocytes in the dermis. A blue-white veil is often found in melanomas and Spitz nevi. See images below.
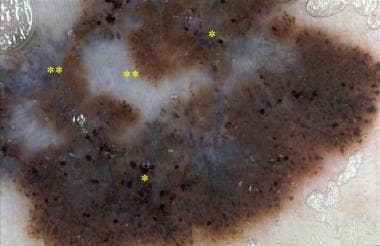 Invasive melanoma with white and gray areas (**), different expressions of pigmented dots (*), and globules (O).
Invasive melanoma with white and gray areas (**), different expressions of pigmented dots (*), and globules (O).
Blue-gray areas
Blue-gray areas are ELM features with coloration varying from gray-blue to deep gray. Blue-gray or bluish areas may be either isolated disseminated granules or peppering and ill-defined spots with bizarre margins (see image below). They may be associated with melanoma regression. They are correlated histologically with the presence of melanin and/or hemosiderin within melanocytes and melanophages, and blue-gray areas may be free in the papillary and middle dermis.
Steel blue areas
Steel blue areas are structureless, gray-blue, and homogeneously diffuse. They are found in blue nevi (see image below) and occasionally are associated with globules, dots, or both. A central steel blue area may be found in some combined blue nevi.
Depigmentation
Depigmentation depends on a lack or reduction of pigment in the pigmented skin lesion. With depigmentation, differentiation can occur in hypopigmented regions that correspond to pigmented areas lighter than other areas within the nevus. Differentiation also can occur in white areas that correspond to well-defined white or milky red-white areas. In contrast to hypopigmented areas, depigmented areas completely lack pigment. Histologically, they correspond to fibroplasia, telangiectasias, and loss of melanin. See images below.
Negative pigment network
Negative pigment network is seen as a negative of the pigmented network with relatively lighter serpiginous lines making up the "cords" of the network and darker areas, filling the holes, resembling elongated tubular or curved globularlike structures. This feature is highly specific for melanoma but it is also correlated with Spitz nevi and can also be seen in dysplastic nevi and in growing melanocytic nevi. Negative pigment network in melanoma, differently from benign lesions, is often focal and asymmetrically distributed histopathologically, the negative pigment network has been suggested to correspond to thin elongated hypopigmented rete ridges accompanied by the presence of large nests of heavily pigmented melanocytic cells located at the dermal papillae.
 A focal and asymmetrically located negative pigment network in the lower periphery of this melanoma (0.85 mm thick).
A focal and asymmetrically located negative pigment network in the lower periphery of this melanoma (0.85 mm thick).
Shiny white streaks, metaphorically called "chrysalis structures," were defined as thick, short, bright, whitish linear structures, often orthogonally oriented. These structures can only be seen with polarized dermoscopy and can be found in melanoma, Spitz nevus, dermatofibroma and basal cell carcinoma. Histopathologically, shiny white streaks probably correspond to changes in the composition and orientation of the collagen.
Nonspecific Guide Criteria
Milialike cysts
Milialike cysts are small, circular, whitish-yellow areas with sizes ranging from 0.1-1 mm (see image below). They are important for the diagnosis of seborrheic keratosis but can also be found in papillary melanocytic nevi and melanoma, although in seborrheic keratosis, they are larger. Histologically, milialike cysts correspond to keratin-filled cysts.
Comedolike openings
Comedolike openings are another typical diagnostic feature of seborrheic keratosis. They are keratin-filled porelike openings that communicate with the surface of the lesion. They appear yellow-brown, with a circular or oval shape and a light round halo (see images below). They are correlated histologically with keratin within the invaginations of the epidermis.
Red-black lagoons
Red-black lagoons are the pathognomonic diagnostic criteria of hemangioma and angiokeratomas. They are small, well-defined, oval or round areas that range from blue-red to blue-black. Histologically, they correspond to large lagoons and thrombi within the vascular spaces of papillary dermis. Subungual hemorrhages can have blue-red and/or red-black homogeneous pigmentation without vascular lagoons. See images below.
Maple leaf–like pigmentations
Maple leaf–like pigmentation, an important diagnostic criterion for basal cell carcinoma, is gray-brown to gray-black with a shape similar to that of a maple leaf or to the fingers of a hand (see image below). Histologically, they correspond to heavily pigmented basaloid cells within the nest of basal cell carcinoma.
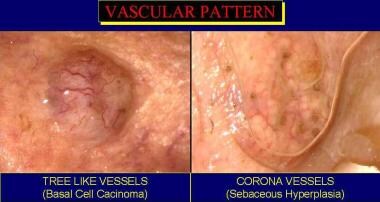
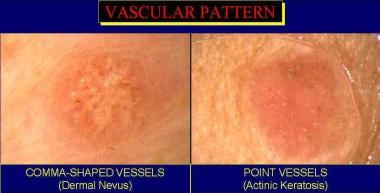
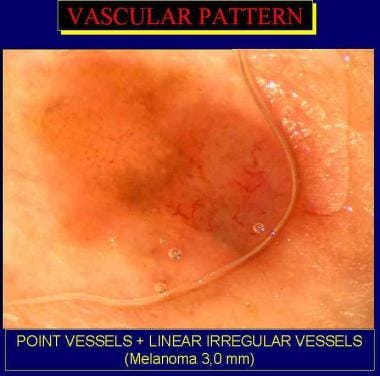
Vascular Patterns
Vascular patterns are important markers for melanocytic and nonmelanocytic lesions. The vascular pattern can be evaluated more accurately using magnification of higher than 10X.
Kreusch and Koch described the main vascular patterns as follows:
-
Treelike vessels are described as thick, arborizing vessels; they are compatible with pigmented basal cell carcinoma of any type. See image below.
-
Corona vessels are thinner and less curved than treelike vessels. Generally, they surround a sebaceous gland hyperplasia. See image below.
-
Comma-shaped vessels are parallel to the skin surface and appear as short, strong, curved vascular structures often visible in the dermal nevi. See image below.
-
Point vessels are short capillary loops visible as pinpoint dots. They are commonly seen in all types of melanocytic tumors and superficial epithelial tumors (ie, actinic keratosis, Bowen disease). See image below.
-
Hairpin vessels are long capillary loops of thicker tumors and are related to angiogenesis of thick melanomas (at the border) but also squamous cell carcinoma, keratoacanthoma, and seborrheic keratosis.
-
A combined evaluation of linear and other types of vascular features is called linear irregular vessels and is often seen in melanoma. See image below.
Bañuls et al reported that, in cutaneous melanoma, vascular morphology on dermoscopy was associated with lesion Breslow index, thickness, ulceration, and regression. Specifically, vessel presence on dermoscopic images of melanoma was associated with thicker melanomas, and linear, irregular vessels were associated with ulceration. Dotted blood vessels were associated with dermoscopic regression. [6]
Additionally, Giuffrida et al found that vascular diameter on dermoscopy could be a useful factor in the differentiation of heavily-pigmented and amelanotic skin lesions. [7]
Overview of Different Dermoscopic Diagnostic Procedures
The different technical instruments and the guidelines for dermoscopy diagnosis for Pigmented skin lesions are described in Guide Criteria and Technical Procedures and Equipment, respectively. This section describes the different methods of classification and diagnosis using dermoscopy that have been developed in the last several years.
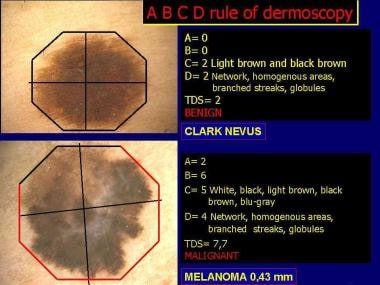
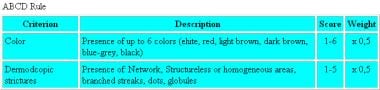
In the world of dermatology, ELM recognition of suggestive melanomas is based on the observation of numerous parameters; not just one of these factors is specific for melanoma. The literature shows that many different methods of classification are used for dermoscopy. The most widely used ELM procedures are pattern analysis, the ABCD dermoscopy rule, the Menzies methods, the 7-point checklist, and the stratification of risk level.
Pattern analysis
Described by Pehamberger et al [8] and more recently redefined by the Consensus Net Meeting on Dermoscopy (CNMD), pattern analysis is the procedure most used by dermatologists. Its efficiency is correlated to the experience of the observer. Pattern analysis uses a process of diagnostic framing that keeps control of the known analytic data of all the dermatoscopic parameters of pigmented skin lesions and of the prevalence of single variables. That is, it helps determine if the PN is present or absent, and, if the PN is present, if it is regular or irregular and delicate or prominent, among other variables discussed earlier.
The various types of pigmented skin lesions, and specifically differentiation between benign and malignant melanocytic lesions, can be determined through pattern analysis of specific dermatoscopic features. The 2 steps in the new process of pattern analysis are (1) deciding whether the lesion is melanocytic or nonmelanocytic and (2) identifying the melanocytic lesion, making a diagnosis, and planning relative management.
Pattern analysis has been deemed superior to the other algorithms (ie, ABCD dermoscopy rule, Menzies method, 7-point checklist) for diagnostic efficiency by experts all over the world in the 2000 CNMD.
Pattern analysis - Step 1
The first step to identifying a melanocytic lesion is to look for the presence of aggregated globules, PN, or branched streaks (ie, fragmented irregular PN).
If the above patterns are absent, other characteristics should be sought (substeps). First, note that a typical marker for blue nevus is the presence of homogeneous steel blue areas. Second, the lesion should be evaluated for the presence of moth-eaten borders, fingerprinting, comedolike openings, and milialike cysts. In this case, the lesion is suggestive of either a solar lentigo or a seborrheic keratosis. Third, if red or red-blue to black lagoons are present, the lesion should be considered a hemangioma or an angiokeratoma.
Finally, the lesion should be evaluated for maple leaf–like structures, arborizing telangiectasias, spoke-wheel–like areas, and gray-blue ovoid nests. This lesion is compatible with a basal cell carcinoma.
All lesions should be reevaluated to determine if they have a melanocytic structure, even if they do not have the structures described above.
Pattern analysis - Step 2
The main goal for step 2 is to make an accurate differential diagnosis between benign melanocytic lesions and melanomas. The important features in distinguishing these 2 groups are the overall general appearance of color, architectural order, symmetry of pattern, and homogeneity, known by the acronym CASH.
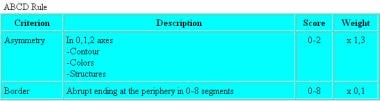
Melanocytic nevi have few colors, a regular design, and symmetrical patterns. In contrast, malignant melanoma often has several colors, architectural disorder, asymmetrical patterns, and heterogeneity. For the asymmetry evaluation, the lesions are bisected by two 90° axes positioned to produce the lowest possible asymmetry score. See the image below.
Importantly, also incorporate color and structural asymmetry into this ELM parameter because most equivocal lesions have a symmetrical contour. Thus, asymmetry must be calculated according to the distribution of colors and structures on either side of each axis, and not solely based on contour, as in the clinical ABCD rule (ie, by naked eye).
-
Borders (B): The emphasis is borders that brusquely interrupt at the periphery. The lesion is visually divided into 8 pie-shaped segments, or eighths, and then the number of segments is counted in which an abrupt cut off is present at the margins of the pigment pattern. The score can range from 0-8 (see image below).
-
Colors (C): The emphasis is the different colors in the lesion (see image below). They include red, white, light and dark brown, blue-gray, and black. White should be counted only if it is lighter than the surrounding skin (white areas) and should not be confused with the hypopigmentation commonly seen in all types of melanocytic lesions. Each color is assigned 1 point, and the total score ranges from 1-6.
-
Different structural components (D): The emphasis is different structural components. These components include the PN, branched streaks (thickened and branched PN anywhere in the lesion, not only at the borders), structureless or homogeneous areas (color, but no structures such as PN, branched streaks, dots, or globules), dots, and globules. In order to be counted, structureless or homogeneous areas must be larger than 10% of the lesion.
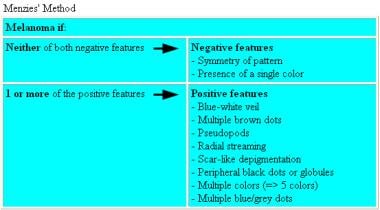
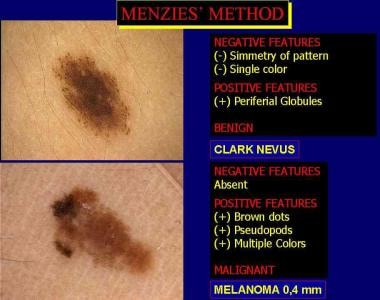
Menzies scoring method
Menzies scoring method is another effort to simplify the pattern analysis ELM system. This classification identifies 2 negative aspects and 9 positive aspects commonly used in the semeiotics of dermoscopy. To make a diagnosis of melanoma, 2 negative aspects (negative features) must be absent from the lesion and 1 or 2 positive aspects (from 1 of the 9 positive features) must be present.
-
Negative features (see images below)
The symmetry of the pattern is related to the symmetry of the melanocytic lesion.
A symmetry of color (a single color) is observed.
-
Positive features (see images below)
A blue-white veil appears as irregular, confluent, structureless, blue pigmentation with an overlying ground-glass or hazy appearance.
Multiple brown dots appear as focal collections of multiple, dark brown dots, not to be confused with the dark brown globules that are larger and are commonly found in benign nevi.
Peripheral black dots and globules appear as black dots and/or globules found at or near the periphery of a lesion.
Radial streaming is observed.
Pseudopods can be considered variations of the fourth criterion. They are radially oriented or bulbous, fingerlike extensions of the PN at the periphery of a lesion. They should not be scored if they are seen regularly or symmetrically around the lesion.
Scarlike depigmentation (white scarlike area) appears white or milky-white and represents true scarring.
Multiple (5-6) colors are observed, including black, gray, blue, red, dark brown, and tan. White is not counted as a color.
Multiple blue or gray dots appear as foci of multiple "pepperlike" small, blue or gray dots. They are irregular in size and shape (not globules) in the regression areas.
A broadened network shows a localized, thickened, and irregular PN.
The 7-point checklist
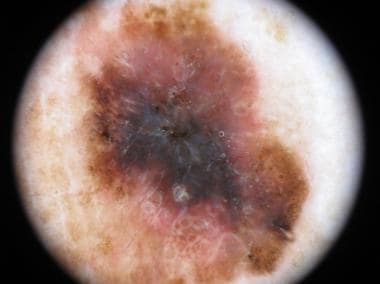
Developed by Argenziano et al [9] in 1998, the 7-point checklist is another variation of the qualitative pattern analysis system, but with a point system. This method uses 7 criteria specific for melanoma. It includes 3 major criteria, to each of which is attributed 2 points, and 4 minor criteria, to each of which is attributed 1 point (see images below). This method has fewer criteria to identify and analyze compared with the pattern analysis method. A score of 3 or greater has a high sensitivity of being melanoma.
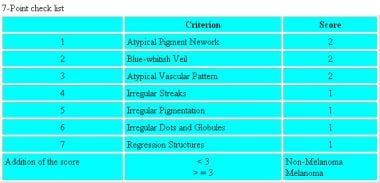 Seven-point checklist uses 7 melanoma-specific criteria: 3 major criteria (score 2 points each) and 4 minor criteria (score 1 point each).
Seven-point checklist uses 7 melanoma-specific criteria: 3 major criteria (score 2 points each) and 4 minor criteria (score 1 point each).
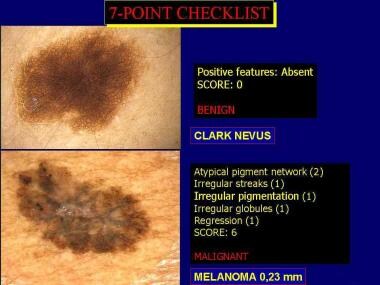 A typical benign melanocytic lesion and a malignant melanoma classified using the 7-point checklist parameters and the relative score.
A typical benign melanocytic lesion and a malignant melanoma classified using the 7-point checklist parameters and the relative score.
See the list below:
-
Major criteria
Atypical PN: Black, brown, or gray thickened and irregular line segments are observed anywhere in a lesion.
Blue-whitish veil: Irregular, confluent, gray-blue to whitish-blue diffuse pigmentation is observed that can be associated with PN alterations, dots/globules, or streaks. This differs from the Menzies definition, in which the blue color should be featureless.
Atypical vascular pattern: Linear-irregular and/or dotted red vessels are not seen in regression areas.
-
Minor criteria
Irregular streaks: Pseudopods or radial streaming are irregularly arranged at the periphery of the lesion.
Irregular pigmentation: Black, brown, or gray featureless areas with an irregular shape and/or distribution are observed.
Irregular dots/globules: Black, brown, or gray; round to oval; variously sized structures are irregularly distributed in the lesion.
Regression structures: White scarlike areas and/or blue pepperlike areas are observed.
Stratification of risk level
Described by Kenet and Fitzpatrick [10] in 1994 and more recently revised by the Melanoma Cooperative Group, this methodology seems to provide very simple and standardized management of both the diagnosis and therapy of early melanomas and suggestive melanocytic lesions.
The stratification of risk level is the basis for the management of melanocytic pigmented lesions. This classification system is based on a wide database of 61,000 examined cutaneous lesions, with 478 diagnosed as cutaneous melanomas (62% stage I, per the American Joint Committee on Cancer). It has 5 risk levels essentially correlated to the history (as described by the patient) and clinical course of the lesion, the presence or absence of a PN, the different variables of the PN associated with the lesion, and other ELM structures (see images below).
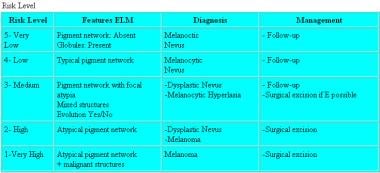 Stratification of risk levels correlated to the different spectra of melanocytic lesions and relative management.
Stratification of risk levels correlated to the different spectra of melanocytic lesions and relative management.
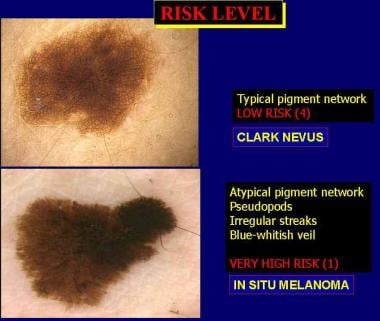 A low-risk melanocytic lesion with a typical pigment network (Clark nevus) and a very high-risk melanocytic lesion (melanoma) classified using the level of risk stratification method.
A low-risk melanocytic lesion with a typical pigment network (Clark nevus) and a very high-risk melanocytic lesion (melanoma) classified using the level of risk stratification method.
The stratification risk level includes the following 3 integrated steps:
-
History and clinical evaluation: Genetic factors, including melanoma susceptibility, and a suggestive clinical history (ie, lesion recently changed shape or dimension) should alert the clinician. After a full body evaluation of the skin, pigmented skin lesions are first classified by the clinical ABCDE rules (ie, asymmetry, irregular border, different colors, diameter >6 mm, evolution) as visible by the naked eye. After this first step, all pigmented skin lesions showing at least 2 ABCDE criteria and a suggestive family or clinical history should be evaluated using dermoscopy.
-
Dermoscopy evaluation, first analysis: A preliminary ELM evaluation should be performed to classify pigmented skin lesions as either nonmelanocytic lesions or melanocytic lesions, using the same criteria according to previous guidelines. Melanocytic lesions must be further subclassified in order to plan the best diagnostic strategy.
-
ELM evaluation, second level evaluation for risk-related classification of melanocytic lesions: Melanocytic lesions are classified as very-low, low, medium, high, and very-high risk lesions on the basis of accurate assessment of structural and morphological parameters. The characteristics and classification of individual lesions is based on the presence or absence of dermoscopy melanocytic features.
Type 1 is considered very high risk. These lesions are suspected of being melanoma because they demonstrate dermoscopy features typical for melanoma.
Type 2 is considered high risk. These are atypical nevi or borderline lesions that manifest an irregular network and other features, such as pseudopods or radial streaming, which, in most cases, indicate the presence of atypia.
Type 3 is considered medium risk. These are lesions with a PN showing the subtle perturbations that may be present in atypical nevi and lesions with melanocytic hyperplasia. The detection of slight alterations can make diagnosis more difficult, lead to overestimation of the seriousness of a lesion, and result in unnecessary surgery. Clinical history and evaluation findings are important aids to avoiding such overdiagnosis.
Type 4 is considered low risk. These are pigmented skin lesions with benign-appearing networks.
Type 5 is considered very low risk. These include lesions with a benign-appearing network and with a globular or other benign ELM pattern.
The Melanoma Cooperative Group emphasizes that anamnesis, clinical observation, and other additional parameters be integrated into dermoscopy evaluations for the stratification of risk level in order to standardize the management of melanocytic lesions.
Practical approach to the management of a pigmented skin lesion
The different dermoscopy classifications have their own worthy internal coherence; however, the use of the different diagnostic scores can be affected by interobserver and intraobserver variability when only a single guideline is used for evaluation (ie, limited qualitative and quantitative agreement). Furthermore, all of these classifications can prove to be very sensitive but not very specific; thus, they do not allow 100% accuracy.
Although very useful to detect intraepidermal lesions, dermoscopy is limited in regard to nodular lesions or clearly dermal lesions, lesions without pigmentation, very dark lesions in which the amount of pigment does not allow the observation of ELM signs, and faintly pigmented seborrhoic warts.
The efficiency of dermoscopy is closely related to an integrated diagnostic synopsis for trained clinicians. The user must think in global diagnostic terms when considering the accuracy of dermoscopy findings, independent of the methods used; a broader aim is to include case histories and clinical assessment.
In fact, the first steps to be integrated by dermatoscopic evaluation are as follows:
-
Anamnesis (personal and family background)
-
Photo-type
-
Previous sunburn history
-
Complete analysis of the entire skin surface (with the intent of finding the so-called "ugly duckling sign")
-
Careful evaluation of the timing of first appearance (and eventual widening) of the lesion being examined and/or modifications of previously existing lesions: A magnifying glass is to be used to carefully observe and evaluate the shape, color, and dimensions of the lesion.
Such a combination of the traditional clinical diagnostic procedures and dermoscopy allows better classification of suggestive melanocytic lesions and a significant reduction in the percentage of unneeded biopsies, but only in pigmented skin lesion centers.
Hot Topics in Dermoscopy
Amelanotic melanoma
Amelanotic malignant melanoma is a subtype of cutaneous melanoma with little or no pigment at visual inspection. A review of the literature indicates that amelanotic melanomas represent 2-8% of all malignant melanomas; the precise incidence is difficult to calculate because the term amelanotic is often used to indicate melanomas only partially devoid of pigment. Truly amelanotic melanomas are rare; often some pigmentation is present at the periphery of the lesion, and they may mimic benign and malignant variants of both melanocytic and non-melanocytic lesions.
According to the extent of the hypopigmentation, amelanotic melanoma can be classified as follows (1) truly amelanotic melanoma, lacking any trace of melanin even if viewed under dermoscopy; (2) partially pigmented melanoma, with larger or smaller pigmented sections covering up to 30% of its total surface; (3) hypomelanotic melanoma, showing a faint brownish tan with little variation of its intensity, which can occupy more than 30% of its total surface and may cover the entire area.
Amelanotic malignant melanoma tends to occur in sun-exposed skin, especially in elderly persons with photodamage, and may appear as erythematous, sometimes scaly, macules or plaques with irregular borders, simulating benign inflammatory plaques, superficial basal cell carcinoma, actinic keratosis, Paget disease, or Bowen disease.
It may also manifest as translucent papules, thereby resembling basal cell carcinoma, or it may clinically resemble keratoacanthoma or Merkel cell carcinoma. Alternatively, it may manifest as an exophytic nodule, often eroded, simulating a pyogenic granuloma or hemangioma, or as a skin-colored dermal plaque/nodule known as desmoplastic malignant melanoma.
From a dermoscopic point of view, amelanotic melanoma lacks most of the dermoscopic criteria reflecting pigmentation, and the vascular structures are frequently the only clue for its diagnosis. The vascular patterns associated to amelanotic melanoma include milky-red globules/areas of dotted or linear irregular or polymorphous vessels (ie, a combination of dotted and linear irregular vessels). In addition, irregular hairpinlike or glomerular vessels can also be found in amelanotic melanoma, albeit less frequently.
Because dermoscopy uses criteria reflecting pigmentation and vascular patterns, it is a useful technique for pigmented melanoma and for amelanotic melanoma. However, the vascular patterns can suggest a diagnosis of melanoma when associated with other criteria found in melanocytic lesions, such as pigment network, irregular pigmentation, streaks, irregular dots/globules, regression structures, and a blue-whitish veil. In truly amelanotic melanoma, vascular patterns alone may not be sufficient to diagnose melanoma because hairpin vessels, dotted areas, and even milky-red areas have also been found in seborrheic keratosis and common nevi, respectively, and in melanomas.
A combined approach of dermoscopic evaluation and clinical examination including clinical information such as age, sex, history of melanoma and/or of excessive sun exposure, number and sites of lesions, time of onset, and descriptions of any changes of the lesion over time must play an important role in the diagnosis of truly amelanotic melanoma and for the so-called "featureless" melanomas that lack specific surface microscopic features.
Difficult melanomas
The primary goal of melanoma detection is early tumor recognition and subsequent surgical treatment. The ABCD method for detecting cutaneous melanoma has been a useful tool in distinguishing benign lesions from melanoma. However, the clinical diagnosis of cutaneous melanoma may be difficult because some melanomas lack all or most of the features of the “ABCD” rule. In fact, some authors have identified a subset of melanomas of unusual appearance, clinically indistinguishable from other pigmented and nonpigmented cutaneous lesions, that escape clinical recognition. The most common clinical diagnoses of these histopathologically confirmed melanomas were nevus, basal cell carcinoma, seborrheic keratosis, and lentigo, while the less common diagnoses included Bowen disease, verruca vulgaris, dermatofibroma, pyogenic granuloma, and hemangioma.
Dermoscopic diagnosis for melanoma also may be difficult because some cases lack specific features for melanoma. Some authors have demonstrated the limitations of dermoscopy in the detection of early melanomas that present with an uncharacteristic dermoscopic appearance. Some melanomas, the so-called "featureless melanomas," may lack specific dermoscopic features for melanoma diagnosis and dermoscopically may even appear as benign melanocytic lesions (nevuslike melanomas) or as atypical nevi, so that the diagnosis is impossible to make on dermoscopic grounds alone. [11, 12]
In fact, difficult melanomas present dermoscopic patterns indistinguishable from those of atypical nevi and common nevi. According some authors, melanomas that failed dermoscopic detection belong to the 3 following categories: melanomas showing criteria of melanocytic nevi, melanomas exhibiting criteria of nonmelanocytic lesions, and melanomas lacking specific criteria of a melanocytic or nonmelanocytic lesion (hypomelanotic/amelanotic melanoma). [13]
In addition, dermatoscopy does not solve the dilemma of discriminating early, featureless melanoma from dysplastic nevi.
Only a meticulous comparative and interactive process based on an assessment of all the individual’s other nevi (ugly duckling sign) and a knowledge about recent changes can lead to the recognition of melanomas that are difficult to diagnose.
Recurrent nevus versus recurrent melanoma
The most important feature suggesting recurrent melanoma is extension of pigment beyond the confines of the scar. Additional features more common in recurrent melanoma include circles, eccentric hyperpigmentation at the periphery, and a noncontinuous growth pattern. In contast, symmetry, radial lines, and a centrifugal growth pattern were more common in recurrent nevi. [14]
Mole mapping
Digital dermoscopy has opened a new perspective in the management of patients at risk of melanoma and in the monitoring of melanocytic lesions.
In particular, the storage of computerized clinical data and dermoscopic images of individual moles in computer-based information systems allows a detailed follow-up of individual melanocytic lesions over time, monitoring changes in their geometry, color, and structure.
Digital monitoring, more commonly referred to as mole mapping, is used to monitor atypical melanocytic lesions without evidence of melanoma-specific criteria, with reevaluation and comparison of changes in the short term (3-6 mo) for the identification of potential or incipient featureless melanomas.
 In situ melanoma, malignant lentigo type, detected using digital dermoscopy. Hyperpigmentation around follicular opening, increasing in size and brown pigmentation suggested atypical melanocytic proliferation after 6 months from baseline.
In situ melanoma, malignant lentigo type, detected using digital dermoscopy. Hyperpigmentation around follicular opening, increasing in size and brown pigmentation suggested atypical melanocytic proliferation after 6 months from baseline.
Another form of digital management is linked to long-term monitoring (>6 mo) in the case of multiple atypical nevi in patients at high risk of melanoma.
In the context of practical applications, although no homogeneous criteria exist for the recognition of the dermoscopic features that define a lesion for digital mapping, some melanocytic nevi may hide a potential melanoma. Features would include the following:
-
Nevus with eccentric hyperpigmentation
-
Nevus with eccentric hypopigmentation
-
Melanocytic nevus with a homogeneous black pattern (no corneal lamella)
-
Nevus with multifocal hypopigmentation/hyperpigmentation
According to the guidelines of the International Dermoscopy Society (IDS), in the presence of multiple atypical melanocytic lesions, dermoscopic monitoring can be planned at 3- to 6 month intervals, where any change suggests surgical excision.
The IDS guidelines suggest that mole mapping at close intervals can be used in the following conditions [15] :
-
Pigmented lesion in a high-risk patient with reported or documented history of change in its clinical and/or dermoscopic appearance
-
Melanocytic lesions with a symmetrical peripheral rim of globules and with an asymmetry of structures within the lesion
-
Atypical blue nevi
-
Isolated pigmented or atypical seborrheic keratosis (seborrheic keratosis–like melanoma)
-
Acral melanocytic lesions in adults, with atypical clinical and/or nontypical dermoscopic pattern
-
Dermatofibromas showing an atypical dermoscopic pattern
-
Lesions with uncertain diagnosis under clinical and/or dermoscopic examination
Surgical excision is, however, strongly recommended in the presence of a single atypical lesion (clinical dermoscopic ugly duckling) for the simultaneous presence of reticular, globular, and homogeneous structures; for the presence of eccentric hyperpigmentation; or for a clear history of recent changes.
During long-term monitoring, symmetrical enlargement is typical of melanocytic nevi. On the contrary, changes in shape and color may be related to malignancy or dysplasia. These substantive modifications include focal enlargement, regression, and change in shape and color (appearance of new colors and/or asymmetrical pigmentation). Furthermore, suspicious structural changes, black dots at periphery, appearance of streaks and/or white veil, and an atypical network can be observed.
Mole mapping should never be performed in atypical nodular lesions, given that diagnosis of nodular melanoma cannot be excluded with certainty. The patients who are typically submitted to periodic inspections have many nevi with a predominant type of atypical nevus. In these individuals, the presence of a lesion not belonging to the predominant type of atypical nevi requires special attention.
The diagnostic and therapeutic challenge in these cases could be related to the number of atypical nevi and the variant of atypical nevus analyzed.
From a practical point of view, the use of mole mapping should be limited to selected patients in whom the clinician has adequately compared the potential benefit (avoiding unnecessary excisional biopsy) with the risk (a possible melanoma being left in place). Even the possibility that the patient does not present at the next scheduled inspection should be taken into proper account, especially during long-term monitoring. In melanocytic lesions with characteristics of incipient or featureless melanoma, short-term digital monitoring is beneficial, providing patient compliance is good. [16]
These atypical melanocytic proliferations detected using sequential digital dermoscopy are likely related to a subgroup of melanoma characterized by slow growing changing in size, disorganized structures, loss of network, appearance of structureless areas, negative network, and new colors.
The "DEPIMELA project" prospectively evaluated the efficiency of dermatologists using dermoscopy alone with others who also performed dermoscopy but with possible access to sequential digital dermoscopy in an everyday clinical setting. This Belgium project showed a reduction in unneeded biopsies when using digital dermoscopy compared to dermoscopy alone with a high number of early melanoma diagnosed by mole mapping.
An abundant amount of literature is available on mole mapping, but interpretation of the data is hampered by extreme variance in the inclusion criteria of the lesions monitored digitally, as well as the risk levels of the patients, the number of nevi, and the ratio of benign to malignant melanomas detected after monitoring.
Digital mole mapping technology obviously allows us to characterize the clinical and dermoscopic life of melanocytic lesions. Up to now, however, it has proved highly difficult to establish standardized criteria that can be applied uniformly across the board and thus be transferred and shared in routine clinical practice. Therefore, the diagnostic accuracy of this technique cannot be assessed at this time.
Integration of digital dermoscopy to others methods
Total body photography
Among patients with multiple nevi (>50), the storage of images of the entire skin surface may represent an important step for the follow-up and to reduce the risk of leaving in place a potential melanoma. In patients at high risk of melanoma, the follow-up digital in 2 steps, including both total body photography and digital dermoscopy, could be a useful method to increase early detection of melanoma, with an increase of the diagnosis of featureless lesions and, at the same time, to reduce the number of unneeded excisions .
Reflectance confocal microscopy
Reflectance confocal microscopy (RCM) has been integrated to dermoscopy with promising impact for research and early diagnosis, especially in diagnostic steps of melanocytic proliferations.
RCM is an emerging technique that allows physicians to obtain noninvasive images of the epidermis and the upper dermis at a resolution comparable to that of histology. Briefly, RCM uses a low-power 830-nm laser beam that generates horizontal sections of the skin of 1 micron lateral resolution up to approximally 200 micron in depth. Several horizontal digital layers (max 8 x 8 mm) can be obtained showing in vivo and real-time tissue morphology and cellular details from epidermis to upper dermis.
The contrast of the images RCM is mainly related to the difference in reflectance of tissue components and cytoplasmic melanin. Thus, melanocytic lesions represent the most appropriate substrate for the RCM examination. RCM has allowed correlating in vivo cellular and architecture parameters of dermoscopic features of melanocytic lesions.
RCM analysis of melanocytic lesion also called virtual optical biopsy is routinely conducted by the evaluation of mosaics and/or a series of high-resolution images. RCM features are generally analyzed at 3 different tissue levels: superficial epidermal layer, dermal-epidermal junction, and superficial dermis. A consensus conference has suggested architectural, cellular, and tissue parameters for RCM evaluation, and diagnostic algorithms have been developed for the diagnosis of melanoma.
Specifically, melanocytic nevi architecture is respected in the various layers; in the surface layer has a honey-combed pattern (stratum granulosum) with cells that appear with black cytoplasm surrounded by a reflecting contour; in the spinous layer a cobblestone pattern can be observed for the typical cobblestone appearance of cells with reflective cytoplasm surrounded by a black halo. At the dermal-epidermal junction, dermal papillae appear as rings of uniform size and reflectance where cells surrounding dermal papillae are the melanin-containing melanocytes that make up the papilla like a string of pearls.
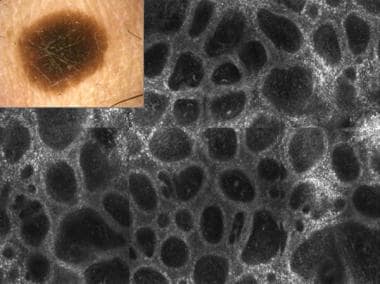 Melanocytic nevus with regular pigment network and central hyperpigmentation. Confocal laser microscopy correlation shows regular architecture. Dermoepidermal junction appears as rings of uniform size and reflectance whereas cells surrounding dermal papillae are the melanin-containing melanocytes that make up the papilla like a string of pearls.
Melanocytic nevus with regular pigment network and central hyperpigmentation. Confocal laser microscopy correlation shows regular architecture. Dermoepidermal junction appears as rings of uniform size and reflectance whereas cells surrounding dermal papillae are the melanin-containing melanocytes that make up the papilla like a string of pearls.
Among atypical melanocytic lesions, architecture could be less respected related to the different degree of atypia. Epidermal superficial layer may present a reflectance and irregular and asymmetrical cell distribution, with the presence of nucleated cells larger than the typical keratinocyte, defined pagetoid cells (with bizarre round or branched shapes). Dermoepidermal papillae may lose the ring structure surrounded by reflective cells, presenting disarrangement as nonedged papillae without a frame until a sheet-like structure. Superficial dermis may show nests of atypical melanocytes (cerebriform nests, scattered cells, isolated nucleated cells). The most important RCM features of malignant melanoma are mainly related to nonedge dermal papillae, atypical melanocytes, and pagetoid infiltration.
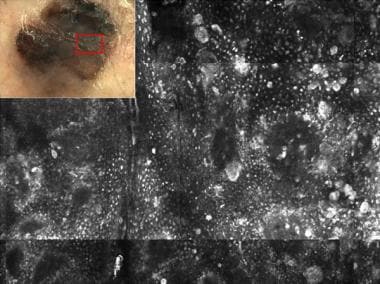 Atypical dermoscopical pattern in invasive melanoma with irregular colors and structures distribution. Reflectance confocal microscopy features are closely related to malignancy for the presence of widespread pleomorphic pagetoid cells (with bizarre, round, or branched shapes) and epidermal disarrangement.
Atypical dermoscopical pattern in invasive melanoma with irregular colors and structures distribution. Reflectance confocal microscopy features are closely related to malignancy for the presence of widespread pleomorphic pagetoid cells (with bizarre, round, or branched shapes) and epidermal disarrangement.
Dermoscopy integrated to confocal laser microscopy can help the clinician in the assessment of equivocal melanocytic lesions, especially on face lesions, keratocytes proliferations, vascular tumors simulating melanocytic lesions, presurgical evaluation of wide malignant lentigo, and to monitor dynamic skin changes during pharmacological, physical, and surgical treatments.
-
Hand-held dermatoscope and stereomicroscope.
-
Videodermatoscope. Courtesy of DS Medica, Milan, Italy.
-
Digital epiluminescence microscopy equipment, Skin Cancer Unit, Centro Prevenzione Oncologica, Ravenna, Italy.
-
Digital camera with implemented EPI30 zoom lens. Courtesy of Alpha Strumenti, Milan, Italy.
-
Brown pigment network in a melanocytic nevus.
-
Brown pigment network in a melanocytic nevus.
-
Light-brown pigment network in a melanocytic nevus.
-
Brown pigment network in a melanocytic nevus.
-
Brown pigment network in a melanocytic nevus.
-
Dark-brown pigment network in a melanocytic nevus.
-
Dark-brown pigment network in a melanocytic nevus.
-
Dark-brown pigment network in a melanocytic nevus.
-
Dark-brown pigment network in a melanocytic nevus.
-
In situ melanoma with asymmetric color distribution, irregular pigment network, and a whitish veil (*).
-
In situ melanoma with asymmetric color distribution, irregular pigment network, and pigment dots with varied size (*).
-
Dysplastic nevus with irregular pigment network and a whitish veil (*).
-
Pseudopigment network of a nevus located on the face.
-
Solar lentigo.
-
Malignant melanoma in situ on face or lentigo maligna.
-
Melanoma in situ with radial streamings at periphery and a whitish veil (*).
-
Microinvasive melanoma with pseudopods at the periphery and a whitish veil (*).
-
Melanocytic nevus with globular pattern.
-
Melanocytic nevus with globular pattern.
-
Melanocytic nevus with regular distribution of globules at periphery.
-
Melanocytic nevus with regular distribution of globules at periphery.
-
Peripheral irregular globules with varied colors in an invasive melanoma.
-
Pigmented dots (*) in a melanocytic nevus.
-
Invasive melanoma with white and gray areas (**), different expressions of pigmented dots (*), and globules (O).
-
Whitish blue veil in a pigmented Spitz nevus.
-
Whitish blue veil and gray-blue areas in invasive melanoma.
-
Homogeneous steel blue areas in a blue nevus.
-
Hypopigmented areas in a melanocytic nevus.
-
White areas in invasive melanoma.
-
Milialike cysts (*) and comedolike openings (O) in seborrheic keratosis.
-
Comedolike openings (*) in seborrheic keratosis.
-
Red vascular lagoons.
-
Subungual hemorrhage.
-
Maple leaf–like pigmentation (*), treelike vascular pattern, and gray-blue ovoid nests in a basal cell carcinoma.
-
On the left, treelike vessels in a basal cell carcinoma, and, on the right, corona vessels that are thin and curved and are surrounding a sebaceous gland hyperplasia.
-
On the left, comma-shaped vessels parallel to the skin surface in a dermal nevi. On the right, point vessels in an actinic keratosis.
-
Linear irregular vessels and pinpoint dots in a malignant melanoma.
-
Global and local patterns such as additional features in the pattern analysis classification system.
-
A typical globular pattern in a Clark nevus and the multifaceted colors and structures visible in a microinvasive malignant melanoma according to the pattern analysis classification. CNMD is Consensus Net Meeting on Dermoscopy.
-
Typical starburst pattern characterized by the presence of pseudopods (streaks) visible at the periphery of the lesion radially distributed in a Reed nevus.
-
The main patterns in acral lesions: parallel furrow pattern, latticelike pattern, fibrillar pattern, and parallel ridge pattern.
-
ABCD rule of dermoscopy. Asymmetry and border with relative weight and score.
-
ABCD rule of dermoscopy. Color and different structures with relative weight and score.
-
The scoring system developed using the ABDC rule of dermoscopy.
-
Grading of melanocytic lesions using total dermoscopy score of the ABCD rule of dermoscopy.
-
Application of ABCD rule of dermoscopy in melanocytic lesions.
-
Menzies method. Classification system used to make a diagnosis of suspected melanoma.
-
Application of Menzies method to evaluate the different spectra of melanocytic lesions.
-
Seven-point checklist uses 7 melanoma-specific criteria: 3 major criteria (score 2 points each) and 4 minor criteria (score 1 point each).
-
A typical benign melanocytic lesion and a malignant melanoma classified using the 7-point checklist parameters and the relative score.
-
Stratification of risk levels correlated to the different spectra of melanocytic lesions and relative management.
-
A low-risk melanocytic lesion with a typical pigment network (Clark nevus) and a very high-risk melanocytic lesion (melanoma) classified using the level of risk stratification method.
-
A polarized system allows for better visualization of vessels and red areas.
-
A focal and asymmetrically located negative pigment network in the lower periphery of this melanoma (0.85 mm thick).
-
Shine white streaks orthogonally oriented in the left periphery of this melanoma.
-
In situ melanoma, malignant lentigo type, detected using digital dermoscopy. Hyperpigmentation around follicular opening, increasing in size and brown pigmentation suggested atypical melanocytic proliferation after 6 months from baseline.
-
Melanocytic nevus with regular pigment network and central hyperpigmentation. Confocal laser microscopy correlation shows regular architecture. Dermoepidermal junction appears as rings of uniform size and reflectance whereas cells surrounding dermal papillae are the melanin-containing melanocytes that make up the papilla like a string of pearls.
-
Atypical dermoscopical pattern in invasive melanoma with irregular colors and structures distribution. Reflectance confocal microscopy features are closely related to malignancy for the presence of widespread pleomorphic pagetoid cells (with bizarre, round, or branched shapes) and epidermal disarrangement.