Practice Essentials
Medial condylar fractures of the elbow, demonstrated in the images below, are rare in adults and children; prompt recognition of these sometimes elusive injuries is imperative so that complications can be averted. [1, 2]
Diagnosis
Visual inspection is often the first step in assessing a patient with a traumatically injured elbow.
Test neurologic function. Perform distal motor and sensory testing of the radial, median, and ulnar nerves.
Standard elbow radiographs, which include anteroposterior and lateral projections, are often sufficient to diagnose a fracture in the acutely injured elbow. In condylar fractures, the radiograph typically reveals widening of the intercondylar distance.
See Presentation and Workup for more detail.
Management
Nondisplaced medial condylar fractures can be splinted during the patient's initial evaluation in a long arm posterior splint; have the patient return for outpatient follow-up in 2-3 days. Displaced fractures require more urgent referral for surgical fixation.
See Treatment and Medication for more detail.
Epidemiology
United States statistics
Trauma to the elbow has a high potential for complications and residual functional disability. Luckily, fractures of the humeral condyles are uncommon in adults. Medial condylar fractures are less common than fractures of the lateral condyle. Together, these injuries account for approximately 5% of all distal humerus fractures in adults.
During adolescence, the distal humerus is the second most common site of physeal injury (second only to the distal radius). Supracondylar fractures account for approximately two thirds of distal humeral injuries in children. [3] In children with elbow fractures, isolated medial condyle fractures are uncommon and account for approximately 1-2% of all distal humerus fractures. In children, medial condyle fractures occur at a peak age of 8-12 years.
Fracture of the medial epicondyle of the elbow, as seen in the image below, is common and occurs in approximately 10% of pediatric elbow fractures. Most of these injuries occur in males aged 10-14 years.
Functional Anatomy
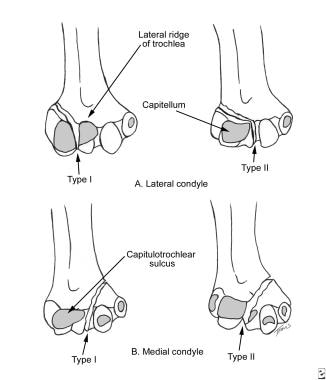
The elbow joint is composed of the bony articulation between the humerus, ulna, and radius. The distal end of the humerus can be divided into the medial and lateral condyles. The articular portion of the medial condyle is the trochlea, and the articular portion of the lateral condyle is the capitulum. The epicondyle is considered part of the nonarticular portion of the condyle. The dividing point for the distal humerus, separating the medial and lateral condyles, is the capitulotrochlear sulcus.
Distinguishing between the articular and nonarticular surface of the condyles is important in the diagnosis and management of condylar fractures. By definition, fractures that involve only the intra-articular surface have no muscular attachments and can only be repositioned by pressure of the opposing articular surface or by open reduction and internal fixation. Fractures that extend beyond the joint capsule have attached muscle and ligaments. The position of the fracture fragment is often influenced by its muscular attachment.
The stability of the elbow is enhanced by its surrounding ligamentous structures. The medial collateral ligament and the lateral collateral ligament (ie, ulnar collateral ligament, radial collateral ligament) provide further stability of the elbow. The radiocapitellar joint is supported by the radial collateral and annular ligaments.
Collectively, the forearm musculature originates from the bony epicondyle prominences. The wrist flexors originate from the medial epicondyle, and the wrist extensors originate from the lateral epicondyle. Because the forearm musculature traverses the elbow joint, some inherent stability to the joint is conferred by muscular contraction.
The structures of the upper arm and elbow are located in either the anterior or posterior compartments. The anterior compartment contains the biceps brachii, brachialis, and coracobrachialis muscles. The anterior compartment also contains the brachial artery, median nerve, musculocutaneous nerve, and ulnar nerve. The ulnar nerve passes behind the medial condyle as it enters the forearm. Because of its location and relatively tight tethering to the epicondyle, the ulnar nerve can be injured when the medial humeral condyle is fractured. The posterior compartment contains the triceps brachii muscle and the radial nerve.
The bony anatomy of the elbow in the pediatric population deserves special mention. Many of the challenges encountered in diagnosing elbow fractures in pediatric patients involve proper knowledge of the ossification centers of the elbow. In general, ossification of the growth centers begins at an earlier age in girls than in boys. Although variation exists, ossification of the growth centers of the elbow occurs at the following times:
-
Capitellum - 11 months
-
Medial epicondyle - 4-6 years
-
Radial head - 5-6 years
-
Olecranon - 6-8 years
-
Trochlea - 9-10 years
-
Lateral epicondyle - 10-12 years
Sport Specific Biomechanics
By definition, the elbow is a true hinge joint that is very stable to all motions except varus and valgus stress. The articulation of the trochlea of the humerus and the olecranon of the ulna defines the plane of flexion and extension at the elbow. The elbow also allows for pronation and supination at the radiocapitellar articulation. The radiocapitellar joint does provide some stability against valgus stress by acting as a buttress to prevent medial elbow opening. Stability is further enhanced by the strength of the ulnar collateral ligament, the principal stabilizing ligament of the elbow that resists valgus stress.
The radial-collateral ligament protects the joint from posterolateral rotary instability and is usually injured during elbow dislocation. The wrist extensor tendons that originate on the lateral intermuscular septum of the arm and the lateral epicondyle provide the elbow with stabilization against varus stress.
Medial condylar fractures generally occur as a result of (1) a fall onto an outstretched upper extremity or (2) a fall onto a flexed elbow. The mechanism of injury appears to be the same in both children and adults.
Prognosis
The outcome of medial condylar fractures depends on the degree of comminution of the fracture, the accuracy of the reduction, and the stability of fixation of the fracture fragment restoring congruity of the articular surface.
In general, nondisplaced fractures that are managed conservatively with a long arm cast have excellent results. In displaced fractures that require open reduction and internal fixation, a good outcome can be expected, with results paralleling the quality of reduction.
Complications
Delayed complications occur with a reasonably high frequency.
Limited flexion and extension is a complication that can occur with medial condylar fractures. Heterotopic ossification may occur and is related to trauma to the brachialis muscle. Usually, pronation or supination is not limited. Mild limitations of elbow movement are usually well tolerated from a functional standpoint.
Cubitus varus (gun stock deformity) can occur and may be the result of decreased growth of the trochlea. This complication may be more likely to occur in displaced fractures that receive no initial treatment.
Cubitus valgus deformities also can occur and appear to be due to secondary stimulation or overgrowth of the medial condyle fracture fragment.
Nonunion/pseudoarthrosis of the fracture fragment can occur as a complication of medial condylar fractures in children. This may be related to the precarious blood supply of the distal fragment and because fractures that traverse the physeal plate are inherently less stable. Kakar et al reported that the vascularized medial femoral condyle corticoperiosteal flap offers another treatment option for humeral nonunions. [4] A study by Su et al found that supracondylar osteotomy can be a safe and effective treatment option for nonunion of pediatric humeral medial condyle fractures. [5]
Yang et al reported a case of nonunion of a humeral medial condylar fracture in a child that resulted from excessive functional exercise. [6]
Posttraumatic arthritis due to chondral injury or residual joint incongruity may occur; it usually manifests several years later. Avascular necrosis may ensue because of the poor vascularity of this area and has been reported for even nondisplaced fractures.
A retrospective study reported the clinical and functional outcomes and the complications that occurred following open reduction and screw fixation of medial epicondyle fractures with intra-articular fragment incarceration. The study concluded that open reduction and screw fixation yielded excellent clinical and functional outcomes for the treatment of medial epicondyle fractures with intra-articular fragment incarceration. The authors also added that particular attention should be paid when treating these potentially serious injuries in order to minimize the risk of possible complications. [7]
-
Milch classification of condylar fractures.
-
Medial epicondylar fracture