Practice Essentials
Spondylolysis, or lumbar pars interarticularis, is a common clinical condition that can result in low back pain. Patients with spondylolysis have a defect in the pars interarticularis of the neural arch, which is the portion of the neural arch that connects the superior and inferior articular facets. On oblique radiographs, the posterior elements form the appearance of a Scottie dog. A break in the pars interarticularis can have the appearance of a collar around the neck (see the images below). Spondylolysis is believed to be caused by repeated microtrauma, resulting in stress fracture of the pars interarticularis. Heredity also is believed to be a factor. [1, 2, 3, 4, 5, 6, 7, 8]
Excessive loading during repetitive hyperextension is a significant risk factor and occurs most commonly at L5, followed by L4. Spondylolysis is bilateral in 80% of symptomatic cases. [1] Approximately 95% of cases of spondylolysis occur at the L5 level. Lyses can occur much less commonly at other lumbar or the thoracic levels. Involvement of multiple levels is rare. Patients with bilateral pars defects can progress to spondylolisthesis. The degree of slippage of adjacent vertebral bodies varies and can progress over time. Patients with spina bifida occulta have an increased risk for spondylolysis. [3, 4, 5, 6, 7, 8]
Imaging modalities
Patients with suspected spondylolysis should be evaluated initially with plain radiography, consisting of anteroposterior, lateral, and oblique views of the lumbar spine. The lateral views are most sensitive for detection of pars fractures, and the oblique views are most specific. Radiography of the lumbar spine is limited by its inability to detect stress reactions in the pars interarticularis that have not progressed to complete fracture. Early spondolytic defects may be seen in approximately 30-38% of the cases. If plain radiographs are negative or inconclusive, further imaging may be warranted. Magnetic resonance imaging (MRI), computed tomography (CT) scanning, and single-photon emission computed tomography (SPECT) bone scintigraphy are used to further evaluate patients with suspected spondylolysis. [9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28]
Some investigators and practicing radiologists believe that after normal radiographs have been obtained, MRI of the lumbar spine should be next. However, the MRI examination must be performed with thin-section images (3 mm) and at relatively high resolution (256 x 192 matrix). Imaging should be obtained in 2 planes: sagittal and axial. Obtain T1-weighted (short recovery time [TR]/echo time [TE]) and T2-weighted (long TR/TE) with fat-suppression images. Usually, this type of MRI examination requires a high-field magnet (minimum of 1 T). [15, 21, 29, 30]
CT scanning of the lumbar spine can be performed after obtaining radiographs or after an equivocal MRI. Perform the examination with stacked thin (2 mm) axial sections through the portion of the spine in question. Perform sagittal reconstructions. However, even without reconstructions, pars fractures can be identified on CT because of the absence of a complete ring of bony structures at a given vertebral level. [9, 12, 21, 22]
CT of the lumbar spine is not sensitive for detecting early acute stress reactions in the pars interarticularis where there is only marrow edema and microtrabecular fracture. [15, 31] These findings, although not visible on CT, are observed easily on MRI; thus, MRI of the lumbar spine can easily identify acute stress reactions in the pars interarticularis. However, direct identification of pars defects may be slightly more difficult with MRI than with CT. The presence of facet osteophytes, combined with volume averaging, occasionally can obscure the presence of the pars defect in the sagittal plane. [32]
SPECT bone scintigraphy also can be obtained after plain radiographs and easily identifies acute stress reaction in the pars interarticularis; however, anatomic details such as the pars defect cannot be identified directly with bone scan. This means that old lyses usually are not seen. [33] SPECT can provide images in the axial, coronal, and sagittal planes. SPECT is superior to planar bone scan and plain radiographs but limited by high rates of false-positive and false-negative results and by high radiation dose. [23, 24] The spatial resolution of SPECT bone scintigraphy is less than that of CT scanning or MRI. [25]
In a prospective study, by Nakashima et al, of 76 adolescent patients with acute and subacute low back pain (46 with lumbar spondylolysis and 30 with low back pain without spondylolysis), MRI and/or CT revealed very early- and early-stage lumbar spondylolysis, but a positive Doppler effect on ultrasonography was also found to be effective in detecting early spondylolysis. [34]
In a study, by West et al, of the accuracy of MRI and CT in 22 young athletes (14.7 ± 1.5 years) diagnosed with spondylosis, the sensitivity and false-negative rate of MRI were, respectively, 59.1% and 40.9%, and the sensitivity and false-negative rate of CT scans were 77.3% and 22.7%, respectively. [35]
In a retrospective study by Morimoto et al to identify how accurately fracture lines can be detected on plain radiographs in patients with lumbar spondylolysis, the fracture line detection rate in early spondylolysis was 11.4% using 2 views, 20.5% using 4 views and 4-D views, and 22.7% using 6 views. In progressive spondylolysis, the fracture line detection rate was 54.2% using 2 views, 70.8% using 4-D views, 75.0% using 4 views, and 79.2% using 6 views. The respective detection rates for terminal spondylolysis were 85.0%, 100%, 100%, and 100%. [36]
(A lateral radiograph of spondylolysis and a defect in the pars interarticularis are presented in the images below.)
 Lateral radiograph of the lumbar spine shows spondylolysis at L5, with spondylolisthesis at L5 through S1. On this single view, it is not possible to determine if these pars defects are unilateral or bilateral. Oblique views may help to resolve this issue.
Lateral radiograph of the lumbar spine shows spondylolysis at L5, with spondylolisthesis at L5 through S1. On this single view, it is not possible to determine if these pars defects are unilateral or bilateral. Oblique views may help to resolve this issue.
 Sagittally reconstructed CT of the lumbar spine shows a defect of the pars interarticularis on the left at L5.
Sagittally reconstructed CT of the lumbar spine shows a defect of the pars interarticularis on the left at L5.
Radiography
On lateral radiographs, which is the most sensitive projection, spondylolysis appears as a linear lucency in the pars interarticularis (see the images below). This lucency also can be seen on oblique radiographs, which is the most specific projection. If spondylolysis is bilateral, the defect should be visible on the right and left obliques. At times, however, the fracture is obscured. The lucency seen in the pars interarticularis on oblique radiographs has been termed the collar on the neck of the Scottie dog. [31, 32, 37, 38]
 Lateral radiograph of the lumbar spine shows spondylolysis at L5, with spondylolisthesis at L5 through S1. On this single view, it is not possible to determine if these pars defects are unilateral or bilateral. Oblique views may help to resolve this issue.
Lateral radiograph of the lumbar spine shows spondylolysis at L5, with spondylolisthesis at L5 through S1. On this single view, it is not possible to determine if these pars defects are unilateral or bilateral. Oblique views may help to resolve this issue.
 Lateral lumbar spine radiograph shows postoperative changes, including posterior spinal fusion at L4-5 and interbody fusion at L4-5.
Lateral lumbar spine radiograph shows postoperative changes, including posterior spinal fusion at L4-5 and interbody fusion at L4-5.
Secondary radiographic signs are occasionally seen in association with spondylolysis, including sclerosis of the contralateral pedicle and the presence of spina bifida occulta at the level of the lysis. [37]
When a pars defect is identified on lumbar spine radiographs, further imaging usually is not needed. False-positive diagnoses of spondylolysis on radiographs of the lumbar spine are uncommon. One possible cause of a false-positive result is bowel gas superimposed over the region of the pars interarticularis that simulates the lucency of the pars defect. False-negative results occur when the lucent defect in the pars interarticularis is not seen or when there is a radiographically occult stress reaction without lysis. Nonvisualization of the pars defect occurs if the plane of the defect lies near the sagittal plane. [37]
A retrospective radiologic analysis, by Alvarez et al, of 111 patients found that lateral flexion-extension views can be useful in the diagnosis of degenerative cervical spondylolisthesis. They also found that MRI missed 38% of cases identified by radiography. [39]
Advances in deep transfer learning have been used to diagnose spondylolisthesis and scoliosis from radiographic images without the need for any measurements, which can help physicians make an early diagnosis with less effort and fewer errors and reduce the need for surgical interventions. [40]
Computed Tomography
Spondylolysis on CT of the lumbar spine is seen as a linear lucency or defect extending through the pars interarticularis. In some patients, fragmentation of the pars interarticularis may be seen. These findings are identified most easily on sagittal reconstructions of the axial images (an example of which appears below). On axial images, a pars defect can be identified easily by virtue of the absence of a complete bony ring at any given vertebral level. [12, 18, 21, 26]
 Sagittally reconstructed CT of the lumbar spine shows a defect of the pars interarticularis on the left at L5.
Sagittally reconstructed CT of the lumbar spine shows a defect of the pars interarticularis on the left at L5.
Bone absorption is seen in the early stage, and it is usually demonstrated as an incomplete fracture. In later stages, spondylolysis progresses to complete fracture and pseudoarthrosis. [41] When spondylolysis is seen on CT scans of the lumbar spine, further imaging is not needed. Decreased-dose CT is the optimal examination to confirm a high suspicion of spondylolysis in children and adolescents, with dose essentially equivalent to radiographs. In a study of 42 pediatric patients at a single institution, decreased-dose CT provided a greater level of agreement than 2D MRI and 2D + 3D MRI. [27] False-negative results can occur on CT scans of the lumbar spine when an acute stress reaction in the pars interarticularis is seen that has not progressed to fracture or fragment.
In a study of 717 CT scans in 532 children, 25 cases of spondylolysis were identified in 14 of 273 boys and 11 of 259 girls, with 12 being associated with grade 1 spondylolisthesis. Prevalence was 1% in children younger than 3 years; 3.7% in children younger than 6 years; and 4.7% for all 532 patients. [28]
Magnetic Resonance Imaging
Spondylolysis on MRI of the lumbar spine has a variable appearance that depends on the timing of the examination. Patients with an acute stress reaction have increased signal on long TR (T2-weighted) images in the pars interarticularis. This represents marrow edema. On short TR (T1-weighted) images, decreased signal is seen in the pars interarticularis. [15, 19, 20, 29, 30, 42, 43, 44]
(See the images below.)
 Long TR (T2-weighted), fat-suppressed, sagittal image shows increased signal in the pars interarticularis on the left at L5. This is an acute stress reaction.
Long TR (T2-weighted), fat-suppressed, sagittal image shows increased signal in the pars interarticularis on the left at L5. This is an acute stress reaction.
 Short TR (T1-weighted), sagittal image shows decreased signal in the pars interarticularis on the left at L5 (same patient as in the previous image).
Short TR (T1-weighted), sagittal image shows decreased signal in the pars interarticularis on the left at L5 (same patient as in the previous image).
Patients with an actual fracture of the pars interarticularis have a discontinuity or fragmentation of the pars interarticularis that is seen best on sagittal short TR images. On long TR images, signal may be decreased in the pars if the process is chronic, indicating reactive sclerosis. If a pars defect is found with increased signal on long TR images, this indicates a subacute process. [29, 30] When spondylolysis is seen on MRI, no further imaging is required. This applies to stress reaction in the pars, as well as to fractures. [29, 30] A false-positive MRI of the lumbar spine rarely occurs when active facet joint arthropathy with reactive marrow edema is seen in the pars interarticularis. [29, 30] Typically, this should have a different appearance than an acute stress reaction in the pars. With arthropathy, edema extends beyond the pars and, possibly, at more than 1 level. A false-negative MRI of the lumbar spine may occur in the setting of facet joint arthropathy with facet osteophytes that obscure the pars defect.
In a study by Yamaguchi et al, spondylolysis was missed by MRI in over half of adolescents in one consecutive series (7 of 11 patients). As a result, the authors suggested that in patients with a history or physical findings suggestive of spondylolysis, such as localized pain of the lumbar spine with back extension, further radiographic evaluation should be considered if an MRI is negative. [45]
Ultrasonography
In a systematic review of 243 studies by Tanveer et al, low-intensity pulsed ultrasound was found to be effective for bone union and served as useful therapy for a quick return to playing sports for patients with lumbar spondylolysis. [46]
Tanveer et al also found that low-intensity pulsed ultrasound significantly reduced pain and functional disability in patients with early-stage lumbar spondylolysis by using the following parameters: 1.1-MHz oscillation frequency, 1-kHz pulsed frequency, 100-mW/cm2 spatial intensity, 2-ms pulse duration, 100-Hz pulse repetition rate, 20% pulse duty cycle, and 20-minute duration on alternate days. [47]
In a study, by Tsukada et al, of 80 young athletes (age range, 10-18 yr) with early-stage lumbar spondylosis, low-intensity pulsed ultrasound (LIPUS) combined with conservative treatment was associated with a shorter median time to return to sports than conservative treatment without LIPUS (61 days vs 167 days). [48]
Nuclear Imaging
Spondylolysis is seen on methylene diphosphonate technetium-99m (99mTc) bone scan with SPECT as increased activity in the pars interarticularis (as seen in the images below). This finding typically represents an acute stress reaction that radiographs of the lumbar spine will not reveal as a defect in the pars. [17, 31]
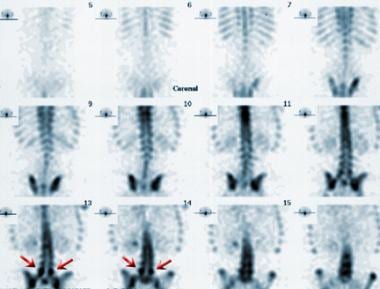 Coronal single-photon emission computed tomography bone scan shows increased activity in the region of the right and left pars interarticularis at L5.
Coronal single-photon emission computed tomography bone scan shows increased activity in the region of the right and left pars interarticularis at L5.
 Axial single-photon emission computed tomography bone scan with increased activity seen in the region of the right and left pars interarticularis at L5 (same patient as in the previous image).
Axial single-photon emission computed tomography bone scan with increased activity seen in the region of the right and left pars interarticularis at L5 (same patient as in the previous image).
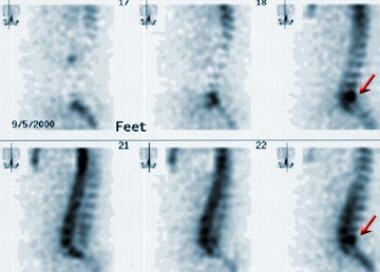 Sagittal single-photon emission computed tomography bone scan (same patient as in the previous 2 images).
Sagittal single-photon emission computed tomography bone scan (same patient as in the previous 2 images).
If increased activity is seen in the pars interarticularis, additional imaging may be needed. Correlation with lumbar spine radiographs is recommended. If radiographs are negative for spondylolysis, consider further imaging with either MRI or CT. Other causes of increased activity may exist in the region of the pars that are not related to spondylolysis. False-positive diagnoses of spondylolysis include infection and osteoid osteoma. These can cause increased activity in the region of the pars similar to that seen with spondylolysis. False-negative diagnoses can occur in the setting of chronic spondylolysis. In this situation, normal activity usually is seen in the region of the pars interarticularis. In addition, old defects of the pars interarticularis may not show increased activity.
Healing stress reactions also may show increased activity in the pars interarticularis. On planar imaging, increased activity in the pars interarticularis may be mistaken for osteoarthritis in the facet joints.
-
Lateral radiograph of the lumbar spine shows spondylolysis at L5, with spondylolisthesis at L5 through S1. On this single view, it is not possible to determine if these pars defects are unilateral or bilateral. Oblique views may help to resolve this issue.
-
Long TR (T2-weighted), fat-suppressed, sagittal image shows increased signal in the pars interarticularis on the left at L5. This is an acute stress reaction.
-
Short TR (T1-weighted), sagittal image shows decreased signal in the pars interarticularis on the left at L5 (same patient as in the previous image).
-
Sagittally reconstructed CT of the lumbar spine shows a defect of the pars interarticularis on the left at L5.
-
Lateral lumbar spine radiograph shows postoperative changes, including posterior spinal fusion at L4-5 and interbody fusion at L4-5.
-
Coronal single-photon emission computed tomography bone scan shows increased activity in the region of the right and left pars interarticularis at L5.
-
Axial single-photon emission computed tomography bone scan with increased activity seen in the region of the right and left pars interarticularis at L5 (same patient as in the previous image).
-
Sagittal single-photon emission computed tomography bone scan (same patient as in the previous 2 images).

