Practice Essentials
Nasopharyngeal carcinoma (NPC) is uncommon in the United States and in most other countries. Although NPC accounts for less than 1% of all cancers in the United States, it is common among Southeast Asians, especially in Chinese persons from the southern provinces of Kwantung, Kwangsi, and Fukien. Close to 130,000 new cases of NPC were reported in 2018. [1, 2, 3]
Native populations in Canada, Alaska, Greenland, and Africa also have increased rates as compared to those of the rest of the world. The mean age at diagnosis is 45-55 years, and the annual rates are 23.3 cases per 100,000 men and 8.9 cases per 100,000 women. The male-to-female ratio is approximately 2-3:1. In China, the incidence varies with geography and decreases from southern to northern China, where rates are 2-3 cases per 100,000 persons per year. In the United States, the risk is increased in first-generation persons of Chinese descent. The rarity and obscure location of NPCs often lead to delayed diagnosis and the finding of an advanced-stage tumor at diagnosis. [1]
Epidemiologic and experimental data suggest at least 3 major etiologic factors: viral, environmental, and genetic.
A close association has been identified between the Epstein-Barr virus (EBV) and NPC. IgA antibodies against EBV proteins have been identified as serologic markers for NPC. Simon et al determined that both IgA and IgG antibodies against multiple EBV proteins are highly sensitive and specific for EBV-positive NPC. [4, 5, 6]
Imaging modalities
Preferred examinations include clinical examination of the neck, fiberoptic examination, CT scanning of the nasopharynx and neck, and MRI of the nasopharynx and neck. [7, 8] Narrow band imaging promises a high level of diagnostic accuracy. [9, 10]
The role of CT is well established. CT remains the most common modality for tumor mapping and nodal staging, particularly in the regions of the globe in which nasopharyngeal carcinoma (NPC) occurs with high frequency, because access to MRI remains limited.
MRI is superior to CT in demonstrating the extent of soft tissue tumors. This is particularly relevant in tumors with extensive submucosal involvement. Generally, CT is accepted as being superior to MRI in the detection of skull base involvement; however, contrary to common belief, changes in the skull base are better identified on MRI than on CT. Although cortical erosion often is diagnosed more confidently by using CT, marrow infiltration is better determined with MRI. MRI is also more sensitive than CT in detecting perineural invasion; the obliteration of fat just external to the foramen rotundum or foramen ovale is as a good sign of early perineural infiltration.
According to some studies by King et al and other researchers, 11% of all NPCs in symptomatic patients could be detected only by MRI, with this number increasing to 17-35% in asymptomatic patients. MRI has also been found to be able to detect NPCs as early as 3 years before being detectable on endoscopy. [11, 12, 13, 14, 15]
Pathologic diagnosis is achieved by examining biopsy specimens from the nasopharyngeal mass. Workup includes assessment of the tumor by means of flexible or rigid endoscopic examination; documentation of the extent of the tumor and the location of neck nodes; assessment of cranial nerve (CN) function, vision, and hearing; CT or MRI of the head and neck regions; chest radiography; and blood work, including complete blood counts and serum chemistry panels, particularly renal function tests.
Cervical lymphadenopathy is depicted better by using CT scans than MRIs, especially in terms of nodal necrosis and extracapsular spread. Although large amounts of data exist regarding the superiority of CT over MRI in the assessment of nodal metastasis, both modalities are adequate in routine clinical practice. Compared with MRI, CT rarely provides additional information that results in a change in treatment options.
MRI is recommended for use in staging tumor recurrences. Although MRI has limitations in separating postirradiation fibrosis from tumor recurrence, it is superior to CT in identifying submucosal infiltration, replacement of marrow in the skull base, and intracranial spread.
In a study by Piao et al of 18FDG PET/MR scans of 60 patients with clinically diagnosed recurrent or metastatic NPC, the overall accuracy of 18FDG PET/MR imaging for staging of recurrent or metastatic NPC was determined to be 88.3%. [4]
In many tumors that are staged with CT, their classification may be changed on MRI, especially in patients with involvement of the skull base or early CN infiltration and intracranial extension. This disparity of staging results between CT and MRI can potentially affect treatment recommendations, which may in turn pose problems in comparing treatment outcomes.
Before the era of CT, plain radiography was used to determine the extent of skull-base involvement by nasopharyngeal carcinoma. The classic 5 views of NPC that Ho described consist of lateral, submentovertical, occipitosubmental, 25° occipitomental, and occipitomaxillary views. [16] CT and MRI have replaced plain radiography for the purpose of staging. Plain skeletal radiography still has a role in the initial evaluation of suspected bone metastases.
Creatinine clearance is determined by using 24-hour urine specimens. Any clinical or laboratory findings suggestive of distant metastases warrant further investigation. Baseline endocrine function is established. Dental and oral hygiene evaluation is necessary before radiation therapy is started. MRI is often more helpful than CT in depicting abnormalities and in defining the extent of tumors.
Evaluation of mucosal lesions is best achieved endoscopically. Imaging findings often lead to incorrect estimates of the extent and frequency of mucosal involvement. Conversely, clinical evaluation is inadequate in tumors located entirely or almost entirely beneath the mucosa. Hence, the full staging process should include endoscopy, clinical examination of the neck, and imaging.
(Images of nasopharyngeal carcinoma are shown below.)
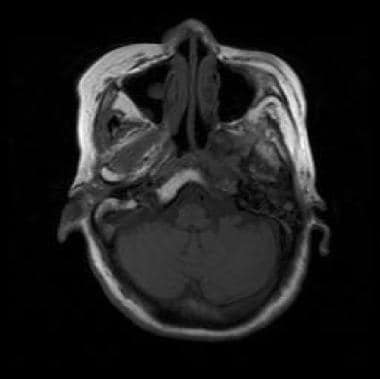 Nonenhanced T1-weighted MRI shows nasopharyngeal cancer invading the left side of the clivus. Signal intensity of the marrow fat is lost on the left side of the clivus compared with the right side.
Nonenhanced T1-weighted MRI shows nasopharyngeal cancer invading the left side of the clivus. Signal intensity of the marrow fat is lost on the left side of the clivus compared with the right side.
Staging for Nasopharyngeal Carcinoma
The Union Internationale Contre le Cancer (UICC) and the American Joint Committee on Cancer (AJCC) have maintained a primary tumor, regional lymph nodes, and distant metastasis (TNM) classification for NPC. [17]
In 1993, the UICC and AJCC collaborated to form a task force at the international level to initiate a process of consultation with the objective of developing a relevant staging classification. The fifth edition of the TNM classification published by the UICC and AJCC in 1997 featured a complete revision of staging classification for NPC. The eighth edition, published in 2017, included modification of T and N categories. [18]
The UICC/AJCC classification system is as follows [17, 19] :
Primary tumor (T):
-
TX - Primary tumor not assessable
-
T0 - No evidence of primary tumor. EBV-positive cervical node involvement
-
Tis - Carcinoma in situ
-
T1 - Tumor confined to the nasopharynx, or tumor extends to oropharynx and/or nasal cavity without parapharyngeal extension
-
T2 - Tumor with parapharyngeal extension and/or extension to adjacent soft tissue (pterygoid and prevertebral muscles)
-
T3 - Tumor involves bony structures of skull base, cervical vertebra, pterygoid and/or paranasal sinuses
-
T4 - Tumor with intracranial extension, involvement of cranial nerves, hypopharynx, orbit, parotoid gland, and/or extensive soft tissue infiltration of the pterygoid muscles
Regional lymph nodes (N):
-
NX - Regional lymph nodes not assessable
-
N0 - No regional lymph node metastasis
-
N1 - Unilateral metastasis in lymph node(s) and/or unilateral or bilateral metastasis in retropharyngeal lymph nodes, 6 cm or less in greatest dimension, above the claudal border of cricoid cartilage
-
N2 - Bilateral metastasis in cervical lymph node(s), 6 cm or less in greatest dimension, above the claudal border of cricoid cartilage
-
N3 - Unilateral or bilateral metastasis in cervical lymph node(s), greater than 6 cm in dimension and/or extension below the claudal border of cricoid cartilage
Distant metastasis (M):
-
MX - Distant metastasis not assessable
-
M0 - No distant metastasis
-
M1 - Distant metastasis
AJCC/UICC stages are as follows:
-
Stage 0: Tis, N0, M0
-
Stage I: T1, N0, M0
-
Stage II: T0, N1, M0; T1, N1, M0; T2, N0, M0; T2, N1, M0
-
Stage III: T0, N2, M0; T1, N2, M0; T2, N2, M0; T3, N0, M0; T3, N1, M0; T3, N2, M0
-
Stage IVA: T4, N0, M0; T4, N1, M0; T4, N2, M0; Any T, N3, M0
-
Stage IVB - Any T, any N, M1
Survival is consistently correlated with the stage of disease. Patients with disease in early stages fare markedly better than others, with overall survival rates of 80% for stage I and 65% for stage II. Survival rates for patients with more advanced disease are 45% in stage III and 30% in stage IV. The extension of the tumor behind the styloid process or into the masticator space is common and is associated with poor survival, with 5-year relapse-free survival rates of 46% and 43%, respectively.
Adverse prognostic features include CN palsies, involvement of the paranasopharyngeal space, advanced age, male sex, and involvement of the lymph nodes. The prognosis is worse with distal lymph node involvement proceeding from the upper cervical chain to the middle and lower cervical chain; patients with bilateral involvement have a 5-year overall survival rate of less than 10%.
Medical/legal pitfalls
Because nasopharyngeal carcinoma (NPC) is a relatively rare condition in Western countries (except for those with cities with a large population of Chinese or Asian individuals), missing an early diagnosis is always a risk. A high index of suspicion is important for a correct diagnosis. The prognosis depends on the stage of the disease; therefore, missing an early disease could be detrimental. Although CT or MRI demonstrates advanced disease well, early disease is frequently not evident on the images. Endoscopic examination with biopsy (if necessary) should always supplement scanning if the patient has symptoms and signs suggestive of NPC.
The accurate delineation of the extent of the disease is crucial, as NPC has a propensity to invade the fissures of the skull base. Because the mainstay of treatment for NPC is radiotherapy, a geographic miss can result from inaccurate delineation of the target volume, especially in this modern era of radiation therapy in which 3D conformal and IMRT (image-guided irradiation) is frequently used to minimize toxicity. If only CT is available, a bone window should always be used. A coronal view is also useful. The skull base should be examined carefully for any invasion, especially in patients with headaches and CN deficits.
Posttreatment follow-up with CT or MRI should always be supplemented with endoscopic examination and biopsy if necessary. CT or MRI may not be sensitive enough to detect a recurrence of small volume.
Imaging guidelines
The National Comprehensive Cancer Network (NCCN) guidelines for head and neck cancers include the following recommendations for imaging of NPC [20] :
-
Initial imaging: MRI with contrast is preferred over CT; imaging should include the skull base to the clavicle.
-
Inconclusive initial imaging: PET/CT should be performed to identify primary sites before intervention.
-
Distant metastases: FDG PET/CT and/or chest CT with contrast.
In 2021, the European Society for Medical Oncology and EURACAN released joint guidelines for the diagnosis, treatment, and follow-up of nasopharyngeal carcinoma. The recommendations concur with the NCCN guidelines. The European guidelines also include the following imaging recommendations for staging NPC [21] :
-
Local and nodal tumor staging: MRI is preferred; FDG-PET may be used to add further accuracy in nodal staging.
-
Locally advanced disease or distant metastases staging: FDG-PET
Computed Tomography
Primary tumor
Imaging of nasopharyngeal carcinoma (NPC) includes thin-section contrast-enhanced neck CT performed in the helical mode from the base of the skull to the thoracic inlet (see the images below). This scanning helps in the easy reconstruction of 3-dimensional data and volumetric measurements. [22]
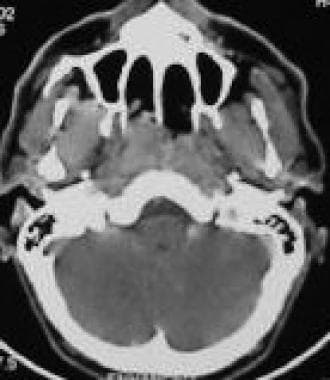
 Contrast-enhanced CT scan shows nasopharyngeal carcinoma with right parapharyngeal extension and retropharyngeal adenopathy.
Contrast-enhanced CT scan shows nasopharyngeal carcinoma with right parapharyngeal extension and retropharyngeal adenopathy.
For tumors confined to the nasopharynx, the delineation of small-volume disease can be difficult by using imaging, and an evaluation of the extent of mucosal disease without knowledge of the endoscopic findings or positive biopsy findings may lead to errors in interpretation. Evaluation of the symmetry of the nasopharynx on CT scans is difficult because of inflammatory changes, secretions, and lymphoid tissue in this region. This is particularly true in the fossa of Rosenmüller, in which the presence of minor asymmetry should not be mistaken for disease. A modified Valsalva maneuver may open a collapsed lateral pharyngeal recess.
For tumors extending out of the nasopharynx, complex anatomic structures and spaces may be involved. The tumor may extend laterally to involve the extrapharyngeal portion of the levator palatini muscle, tensor palatini muscle, pterygoid plates, parapharyngeal fat space containing branches of CN V3, the medial pterygoid muscle, the lateral pterygoid muscle, temporalis and masseter muscles, mandible, and, posterolaterally, the parotid gland. Posterior extension of the tumor can involve the prevertebral muscles, clivus, anterior portion of the foramen magnum and the C1 and C2 vertebral bodies, and, posterolaterally, the carotid space containing the internal carotid artery, jugular vein, CNs IX-XII, the cervical sympathetic plexus, and retropharyngeal nodal metastasis.
Anterior extension of the tumor can involve the pterygoid process, nasal cavity, pterygomaxillary fissure, pterygopalatine fossa, maxillary sinus, and posterior ethmoid air cells. Superior extension of the tumor can involve the structures in the skull base, including petrous temporal bone; sphenoid muscle; foramina lacerum, ovale, and rotundum; carotid canal; sphenoid sinus; cavernous sinus; cranium; and orbit. Inferior extension of the tumor can involve the oropharyngeal area.
The sinus of Morgagni is an opening in the pharyngobasilar fascia through which the levator palatini and eustachian tube pass to the fascia to reach the nasopharyngeal mucosal space. This defect is located close to the lateral pharyngeal recess, which is the most common site for the development of NPC. Tumor extension to the parapharyngeal space frequently occurs at this point. On CT scans, the parapharyngeal space is the most common region in which lateral extension is revealed, with involvement occurring in 84% of the patients. Parapharyngeal extension is associated with serous otitis media due to the blockage of the eustachian tube. Opacification of the middle ear and mastoid air cells is seen frequently on CT scans.
Thin-section axial and coronal CT scans obtained with a bone window can reveal invasion of the skull base, which can occur in locally advanced NPC. Thin-section axial and coronal CT scans are sensitive for early cortical invasion; however, an increasing body of evidence suggests that MRI has several advantages over CT in the depiction of skull-based invasion in NPC.
Intracranial disease may extend to involve the cavernous sinus, middle cranial fossa, and (less commonly) the posterior cranial fossa. MRI is more sensitive than CT in delineating the extent of disease.
Invasion of the paranasal sinus may occur, involving the sphenoid sinus and posterior ethmoid air cells in 26% and 18% of patients, respectively. Extension to the maxillary sinus occurs in 9% of patients and usually is associated with sphenoid infiltration and very advanced disease.
Nodal metastases
The retropharyngeal, submandibular, submental, and lateral cervical nodes are the clinically important lymph nodes in NPC. Approximately 75% of patients with NPC have palpable cervical lymphadenopathy. Neck node involvement in NPC occurs by means of downward stepwise spread. The lower the level of spread, the worse the prognosis. This finding was used in development of the AJCC/UICC staging system for NPC. [17]
Retropharyngeal lymph nodes and the most superior internal jugular nodes are not palpable on clinical examination, and clinical examination has false-positive and false-negative rates of 25% and 10-15%, respectively, in the detection of lymph nodes. In addition, differentiating a single large lymph node from multiple matted nodes is difficult. CT scans can provide information about the patient's nodal status.
Diagnostic criteria for metastatic lymph nodes depicted on CT scans include size, shape, extracapsular invasion, nodal grouping, and central necrosis.
Regarding size, the upper limits of normal for maximal nodal diameter are 1.5 cm and 1.0 cm for jugulodigastric and submandibular nodes and for other lymph nodes, respectively. Nodes exceeding these limits have an 80% likelihood of being metastatic. The minimum axial diameter has been suggested as a more accurate criterion for evaluation. The accepted limits for digastric nodes and other cervical nodes (except retropharyngeal nodes) are 1.1 cm and 1.0 cm, respectively. For retropharyngeal nodes, 0.4 cm is the upper limit in the lateral group, and any visible node is regarded as abnormal in the medial group.
In terms of shape, metastatic nodes are usually more spherical than hyperplastic nodes.
Regarding extracapsular invasion, the nodal capsule is enhancing, and poorly defined margins are present around the node.
For the criterion of nodal grouping, 3 or more contiguous and confluent lymph nodes are present, each of which has a maximum diameter of 8-15 mm (or minimum axial diameter of 8-10 mm).
Central necrosis is the most accurate CT diagnostic criterion for a metastatic node. On nonenhanced CT scans, central necrosis appears as an area of low attenuation in the center of the node. On contrast-enhanced CT scans, the necrosis appears as a nonenhancing area in the center of the node surrounded by a thin rim of peripheral enhancement. Nodal lipid metaplasia sometimes looks like central nodal necrosis.
Degree of confidence
In tumors confined to the nasopharynx, the delineation of small-volume disease can be difficult by using imaging, and any evaluation of the extent of mucosal disease without knowledge of the endoscopic findings or positive findings in biopsy sites may lead to errors in interpretation.
Evaluation of symmetry of the nasopharynx by using CT scans is difficult because of inflammatory changes, secretions, and lymphoid tissue within the region. This limitation is particularly true in the fossa of Rosenmüller, where minor asymmetry should not be mistaken for disease. A modified Valsalva maneuver may open a collapsed lateral pharyngeal recess.
CT versus MRI
MRI has the advantage over other studies in this area because T2-weighted and contrast-enhanced T1-weighted images can be used to differentiate the high signal intensity of the mucosa from the lower signal intensity of the adjacent torus tubarius and intrapharyngeal portion of the levator palatini muscle. In the evaluation of parapharyngeal extension, CT is inferior to MRI in distinguishing compression as a large bulging tumor still confined within the mucosal space resulting from direct invasion. For the detection of skull-base invasion, thin-section axial and coronal CT scans with bone windows are inferior to MRIs.
The node of Rouviere (retropharyngeal node) is the first-echelon node for lymphatic drainage of the nasopharynx. The medial retropharyngeal nodes are usually not visible. Any CT or MRI finding of medial retropharyngeal node is abnormal.
Multidetector-row CT
With the advent of multidetector-row CT (MDCT) scanners, images with unprecedented resolution can readily be obtained. These scanners can substantially reduce scanning time and, therefore, artifact generated by patient motion. MDCTs have a row of detectors to collect the X-ray beam transmitted through the patient and thereby allow for the collection of rich volume data.
Simply, the volume data can be used to construct thin images with high spatial resolution. Thin axial images result in decreased artifact due to partial-volume averaging. Technical improvements of these scanners, such as high special resolution in longitudinal axis and voxels that are virtually isotropic, have led to improved quality of sagittal, coronal, and any other intermediate reformatted or 3-dimensional (3D) images.
One of the many advantages of MDCT scanners is the reduction, and essentially elimination, of misregistration artifact that was commonly seen on reformatted images obtained with older scanners. A high-quality CT scan can be accurate in delineating the extent of primary nasopharyngeal tumor, metastatic adenopathy, and destructive bony changes at the skull base. Fast scanning also allows for imaging when the bolus of contrast agent is mostly intra-arterial; therefore, it provides exquisite depiction of the vascular anatomy. This information can be helpful in assessment of the vasculature when the primary tumor or the adenopathy is extensive and causes vascular encasement.
False positives/negatives
Evaluation of the symmetry of the nasopharynx by using CT scans is difficult because of the inflammatory changes, secretions, and lymphoid tissue in this region, particularly the fossa of Rosenmüller, in which the presence of minor asymmetry should not be mistaken for disease. A modified Valsalva maneuver may open a collapsed lateral pharyngeal recess. Occasionally, CT scans may fail to depict an early cortical erosion of the skull base that is depicted on MRIs.
Magnetic Resonance Imaging
Primary tumor
MRI is extremely helpful because of its multiplanar capabilities and its superior depiction of soft tissue details (see the images below). Evaluation of the symmetry of the nasopharynx can be difficult by using CT scans. [23, 24, 25]
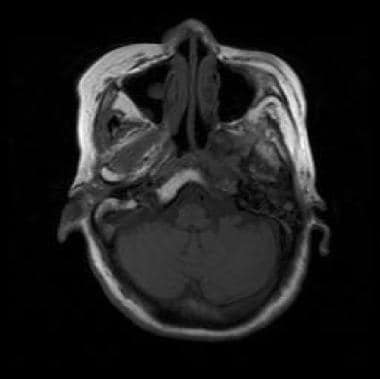 Nonenhanced T1-weighted MRI shows nasopharyngeal cancer invading the left side of the clivus. Signal intensity of the marrow fat is lost on the left side of the clivus compared with the right side.
Nonenhanced T1-weighted MRI shows nasopharyngeal cancer invading the left side of the clivus. Signal intensity of the marrow fat is lost on the left side of the clivus compared with the right side.
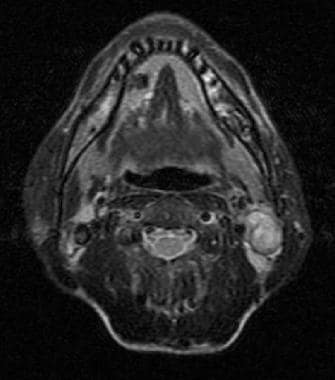
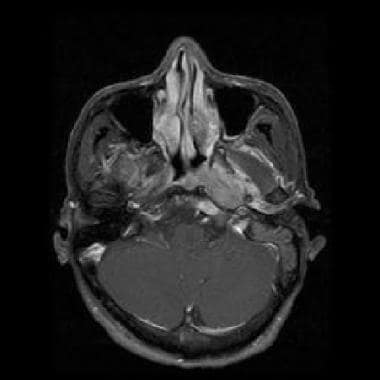 Gadolinium-enhanced axial T1-weighted MRI shows nasopharyngeal cancer with left parapharyngeal involvement.
Gadolinium-enhanced axial T1-weighted MRI shows nasopharyngeal cancer with left parapharyngeal involvement.
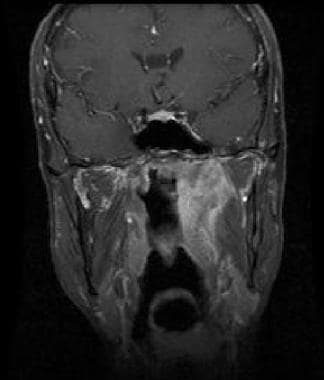 Coronal gadolinium-enhanced T1-weighted MRI shows nasopharyngeal cancer with parapharyngeal extension (same patient as in the previous image).
Coronal gadolinium-enhanced T1-weighted MRI shows nasopharyngeal cancer with parapharyngeal extension (same patient as in the previous image).
 Axial T2-weighted image shows a left-sided cervical nodal metastasis resulting from nasopharyngeal cancer.
Axial T2-weighted image shows a left-sided cervical nodal metastasis resulting from nasopharyngeal cancer.
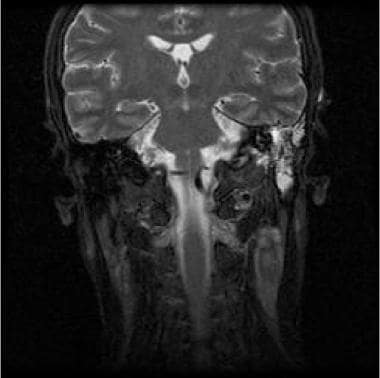 Coronal T2-weighted MRI shows a left-sided cervical nodal metastasis resulting from nasopharyngeal cancer (same patient as in the previous image).
Coronal T2-weighted MRI shows a left-sided cervical nodal metastasis resulting from nasopharyngeal cancer (same patient as in the previous image).
T2-weighted and contrast-enhanced T2-weighted MRIs can be used to differentiate the high signal intensity of the mucosa from the low signal intensity of the adjacent torus tubarius and intrapharyngeal portion of the levator palatini muscle. The tumor has a long relaxation time and is slightly hyperintense relative to muscle on T2-weighted images and isointense on T1-weighted images.
After gadolinium enhancement, the signal intensity of the tumor is greater than that of muscle but less than that of the mucosa on T1-weighted images. T2-weighted images demonstrate good contrast between the tumor and adjacent structures in the nasopharyngeal mucosal space. The pharyngobasilar fascia is usually well demonstrated on MRI but not on CT scans.
T1-weighted images are also ideal for the depiction of anatomic structures, and they are less prone to artifact than other images. Generally, the primary tumor and area of metastatic adenopathy (pathology) are hyperintense and appear conspicuous on a background of predominantly isointense-to-hypointense signal on short-tau inversion recovery (STIR) images. A similar effect can be achieved by suppressing fat signal intensity on the routine T2-weighted images.
For the evaluation of parapharyngeal extension, CT is inferior to MRI in distinguishing compression as a large bulging tumor still confined within the mucosal space resulting from direct invasion. Extension of disease to the nasal cavity is well demonstrated on multiplanar MRI, especially around the superior meatus and sphenoethmoidal recess. MRI can help distinguish direct tumoral extension from retropharyngeal nodes in the evaluation of oropharyngeal involvement.
Contrary to common belief, involvement of the skull base is better identified on MRI than on CT. Although cortical erosion is often diagnosed more confidently with CT than with MRI, MRI better depicts bone marrow infiltration, which appears as moderately low signal intensity against the high signal intensity of fatty bone marrow on T1-weighted images without gadolinium enhancement. However, after the administration of contrast agent, the enhancing tumor may have signal intensity similar to that of bone marrow, rendering interpretation more difficult. Contrast-enhanced and fat-saturated T1-weighted sequences have been used to overcome this problem. In the evaluation of intracranial extension of disease, MRI is superior to CT because MRI provides better contrast between the tumor and brain tissue and because MRI is multiplanar. [26, 27, 28]
Nodal metastases
Fat surrounding the nodes decreases the conspicuity of the nodes on MRIs. Diagnostic criteria for nodal metastasis on CT also apply to MRI. The most accurate diagnostic criterion is central necrosis. Nodes with central necrosis usually have a heterogeneous appearance on both T1- and T2-weighted MRIs. Because blood products may have low, intermediate, or high signal intensity, hemorrhage into a metastatic lymph node may have a relatively homogeneous appearance. Contrast enhancement increases the sensitivity for central necrosis, but the surrounding hyperintensity of fat on T1-weighted MRI obscures the enhancing rim. Fat-suppressed contrast-enhanced sequences may be the optimal sequences for detecting nodal metastasis. The retropharyngeal nodes, which are usually affected first, are easily demonstrated on MRI.
The acquisition time for MRI is significantly longer than that of CT. Therefore, the patient must be instructed to minimize swallowing and not to move during imaging. As stated earlier, CT significantly reduces motion artifact because of its short acquisition time. It also allows for scans to be obtained during a breath hold. Dynamic maneuvers such as modified Valsalva maneuver can be done during CT scanning to expand the pharyngeal recess to evaluate lesions that are poorly demonstrated because of apposition of mucosal surfaces
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Degree of confidence
Overlap exists between nonspecific adenopathy, nodes involved by granulomatous disease, and malignant nodes when the MRI relaxation time is used to characterize lymphadenopathy. By comparing signal intensities of the lymph nodes in nonenhanced and contrast-enhanced MRIs, benign nodes have a ratio of signal intensity significantly lower than that of metastatic nodes. Sensitivity and specificity are reportedly 95% and 84%, respectively. However, this method is impractical if performed routinely, because nonenhanced and contrast-enhanced MRIs must be obtained 10-48 hours apart.
The node of Rouviere (retropharyngeal node) is the first-echelon node for lymphatic drainage of the nasopharynx. The medial retropharyngeal nodes are usually not visible. Any CT or MRI finding of medial retropharyngeal node is abnormal.
According to some studies by King et al and other researchers, 11% of all NPCs in symptomatic patients could be detected only by MRI, with this number increasing to 17-35% in asymptomatic patients. MRI has also been found to be able to detect NPCs as early as 3 years before being detectable on endoscopy. [11, 12, 13, 14, 15]
Ultrasonography
Because the size of lymph nodes is not a highly reliable criterion for malignancy as compared to their structure, fine-needle aspiration cytology under ultrasonographic (US) guidance offers additional information about enlarged lymph nodes. Because US can show malignancy in small lymph nodes not detected with other methods, it can be recommended in most patients with head and neck cancer, irrespective of the use of CT or MRI. One group from Europe demonstrated a slightly lower sensitivity with US than with other studies, but they had superior specificity with US and US-guided fine-needle aspiration biopsy compared with CT in detecting regional metastases in clinically negative necks. [29, 30, 31]
US diagnostic criteria for an abnormal node include size, shape, internal structure of the node, and nodal borders. Lymph nodes smaller than 5 mm are rarely metastatic. Nodes larger than 9 and 7 mm in transverse diameter in the jugular and in the submandibular and submental areas, respectively, are considered metastatic. Overall, these dimensions are smaller than the diagnostic limits accepted for CT or MRI.
In terms of shape, a short axis–to–long axis ratio (SALAR) greater than 0.5 indicates a spherical node, whereas a SALAR less than 0.5 signifies an oval node. Benign nodes tend to be oval, and metastatic nodes tend to be round. By using a combination of the shape and size criteria, lymph nodes larger than 10 mm in the long axis with a SALAR greater than 0.5 have a high incidence of malignancy.
Regarding the internal architecture of the node, coagulation necrosis, echogenic hilus, and cystic necrosis have been depicted on sonograms; however, distinguishing a benign node from a malignant node is often not possible on the basis of the internal architecture alone.
Lymph nodes with well-delineated borders are more likely to be malignant than lymph nodes with poorly delineated borders.
Data from Ahuga et al showed that metastatic neck nodes from NPCs are always hypoechoic relative to the surrounding tissues, and calcification is absent. [32] About 74% of the nodes are spherical, 91% have sharp borders, 84% show no echogenic hilus, 94% are homogeneous, 6% show central nodal necrosis, and 12% show distal enhancement. Most nodes are found in the upper cervical area and in the posterior triangle.
Degree of confidence
In the evaluation of cervical adenopathy, high-resolution US has a sensitivity greater than that of clinical examination and a high specificity when combined with cytologic analysis of specimens from fine-needle aspiration cytology. As such, it is a useful initial tool for distinguishing benign from malignant disease. US can also be used to monitor posttherapeutic changes and to confirm a lack of evidence of disease in the neck.
Nuclear Imaging
In some centers, bone scanning has been used to detect bone erosion; however, because of its low spatial resolution, bone scanning is limited in the modern management of nasopharyngeal carcinoma (NPC). The main role of such nuclear medicine studies is the detection of metastatic disease to the bone. [33, 34]
The use of positron emission tomography (PET) to detect distant metastases has been gaining popularity, but its role in the management of NPC is still not well defined. [35, 36, 37] One study showed that [18]F-fluoro-2-deoxy-D-glucose (FDG) PET may be better than CT in detecting neck lymph node metastases of NPC and for assessing the stage of NPCs.
Nishioka et al reported the use of imaging fusion between FDG PET MRI/CT to improve the delineation of target in planning irradiation of head-and-neck cancers in 9 patients with NPC. Gross tumor volume was determined on the basis of result of clinical examination and on FDG uptake on the fusion images. Clinical target volume was determined by following the usual pattern of lymph node spread for each disease entity and by evaluating the clinical presentation of each patient. The authors showed that fusion techniques improve delineation of the gross tumor volume and clinical target volume, as well as tissue sparing. [24]
A small study by Rudmik et al suggested that PET/CT performed before panendoscopy provides a more targeted treatment plan and will increase the diagnostic yield in the unknown head and neck primary population. In this prospective, single-blinded clinical study, the detection of the primary tumor increased from 25% to 55% with the use of PET/CT. [38]
-
Nonenhanced T1-weighted MRI shows nasopharyngeal cancer invading the left side of the clivus. Signal intensity of the marrow fat is lost on the left side of the clivus compared with the right side.
-
Gadolinium-enhanced axial T1-weighted MRI shows nasopharyngeal cancer with left parapharyngeal involvement.
-
Coronal gadolinium-enhanced T1-weighted MRI shows nasopharyngeal cancer with parapharyngeal extension (same patient as in the previous image).
-
Axial T2-weighted image shows a left-sided cervical nodal metastasis resulting from nasopharyngeal cancer.
-
Coronal T2-weighted MRI shows a left-sided cervical nodal metastasis resulting from nasopharyngeal cancer (same patient as in the previous image).
-
Contrast-enhanced CT scan shows nasopharyngeal carcinoma with right parapharyngeal extension and retropharyngeal adenopathy.
-
Contrast-enhanced CT scan shows nasal involvement resulting from nasopharyngeal carcinoma.
-
Nonenhanced CT scan (coronal view) shows thickening of the right parapharyngeal wall.