Practice Essentials
Optic nerve glioma (also known as optic pathway glioma) is the most common primary neoplasm of the optic nerve. Optic pathway gliomas are benign tumors that are classified as pilocytic astrocytomas. They constitute 50% of primary optic nerve tumors and 1.5-4% of all orbital tumors. [1, 2] Along with reducing visual acuity in the affected eye, the tumor sometimes produces additional symptoms as it grows. A low-grade form of this neoplasm, benign optic glioma, occurs most often in pediatric patients. Another form, aggressive glioma, is most common in adults; it is frequently fatal, even with treatment. [3, 4, 5] Many children with optic nerve glioma are also known to have neurofibromatosis type 1 (NF-1) or, in some cases, hybrid phakomatosis. [6, 7, 8]
(See the images below.)
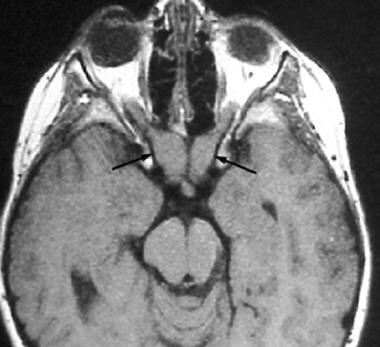
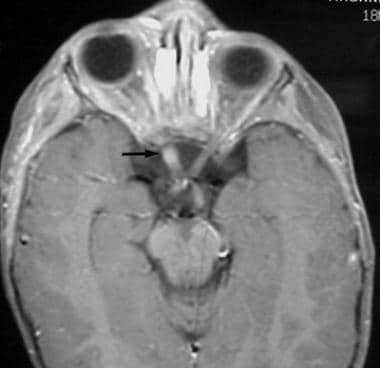
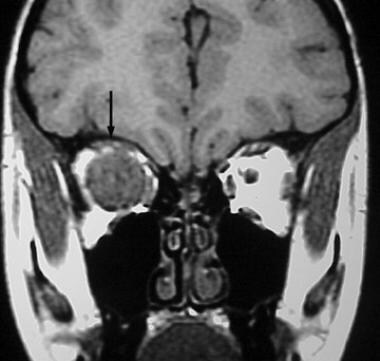 Coronal noncontrast T1-weighted MRI reveals a large intraorbital mass (arrow) centered on the optic nerve.
Coronal noncontrast T1-weighted MRI reveals a large intraorbital mass (arrow) centered on the optic nerve.
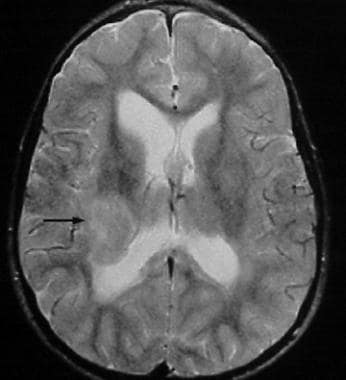 Axial T2-weighted MRI in a 46-year-old man demonstrates a mass in the lateral geniculate nucleus of the thalamus resulting from contiguous extension of the patient's known optic nerve glioma.
Axial T2-weighted MRI in a 46-year-old man demonstrates a mass in the lateral geniculate nucleus of the thalamus resulting from contiguous extension of the patient's known optic nerve glioma.
Preferred examination
Contrasted computed tomography (CT) scanning can be used to characterize local involvement of optic nerve glioma within the orbit. However, magnetic resonance imaging (MRI) better demonstrates the extent of the lesion's intracranial growth. [9, 10] Although MRI may reveal even subtle lesions of the optic nerve, CT scanning can detect a subtle erosion or expansion of the optic canal. In addition, fine calcification, which may help to identify a lesion as a meningioma rather than a glioma, is visualized best through CT scanning.
When the diagnosis is in question, the presence of an intraconal mass can often be detected through CT scanning. MRI, however, is the preferred method for definitive evaluation of optic nerve glioma. Both the intraorbital lesion and its intracranial extent can be effectively characterized through MRI. When evaluating the orbit, gadolinium-enhanced T1-weighted images with fat saturation can define the extent of aggressive glioma. Intracranially, MRI allows better evaluation of the optic nerve, chiasm, tracts, geniculate body, and optic radiations than does CT. [4, 5, 11, 12, 13, 14, 15, 16, 17]
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see Use of Gadolinium in MRI and MRA Linked to NSF/NFD in Patients With Renal Failure.
Computed Tomography
In children, unenhanced CT scans typically reveal a marked, diffuse enlargement of the optic nerve, with characteristic kinking or bending. The enlargement may be tubular, fusiform, or excrescent. [18] Areas of lucency may result from mucinous or cystic changes. Approximately 50% of the lesions demonstrate enhancement; this characteristic is more common with intracranial (especially retrochiasmatic) extension. Calcifications are rare.
The diagnosis may be made with a high degree of confidence when the lesion involves the optic chiasm and retrochiasmatic optic pathway. When confined exclusively to the orbit, the lesion may mimic optic neuritis or optic nerve meningioma; in this setting and in most instances, MRI is a better diagnostic tool than is CT scanning. CT scanning is the better modality for identifying uncommon meningioma with flecks of calcification, which are rare in optic nerve glioma.
False-positive results can occur because of unilateral optic nerve enhancement or other unilateral disorders, such as optic meningioma, vascular lesions, neuritis, pseudotumor, and sarcoidosis. In addition, subtle nerve enhancement occasionally may develop in normal individuals. Improper examination techniques, including failure to administer contrast or obtain thin sections, can lead to a false-negative diagnosis.
Magnetic Resonance Imaging
The diagnosis may be made with a high degree of confidence on MRI when the lesion involves the optic chiasm and retrochiasmatic optic pathway. When confined exclusively to the orbit, the lesion may mimic optic neuritis, pseudotumor, lymphoma, or optic nerve meningioma. Classically, meningioma, the primary differential diagnostic consideration, is characterized by the "tram-track" sign, [19] with enhancement of the periphery of the nerve–optic sheath unit. On the other hand, enhancement in optic nerve glioma is more uniform. Isolated enlargement of the optic nerve sheath also may present diagnostic difficulty; however, this enlargement can usually be distinguished by its signal characteristics, which follow fluid signal on all MRI pulse sequences.
In most instances, including those described above, the diagnosis can be made with greater confidence using MRI than it can with CT scanning. A false-positive diagnosis can occur as a result of unilateral optic nerve enhancement or other unilateral disorders, such as optic meningioma, vascular lesions, neuritis, pseudotumor, lymphoma, and sarcoidosis. In addition, subtle nerve enhancement occasionally may develop in normal individuals. Improper examination techniques, including failure to administer contrast, use fat saturation, or obtain thin sections, can result in a false-negative diagnosis.
Usually, the lesions are hypointense to isointense relative to the optic nerve on T1-weighted images and are hyperintense to it on T2-weighted images. Enhancement is uniform and intense.
Patients without NF-1 demonstrate cystic components more commonly at T2 -weighted imaging. [20]
On T1-weighted images, optic nerve gliomas are usually isointense to the cortex and hypointense to white matter. Invariably, the lesions are hypointense to orbital fat. [5, 17]
(See the image below.)
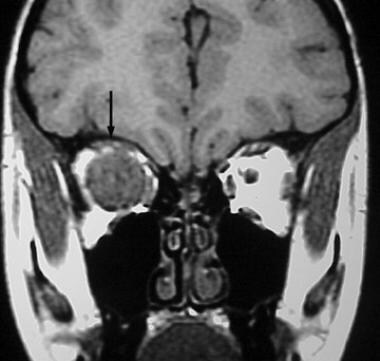 Coronal noncontrast T1-weighted MRI reveals a large intraorbital mass (arrow) centered on the optic nerve.
Coronal noncontrast T1-weighted MRI reveals a large intraorbital mass (arrow) centered on the optic nerve.
On T2-weighted images, lesions demonstrate a mixed appearance that is isointense to hyperintense relative to white matter and the cortex. Following contrast administration, intense enhancement is common. (See the images below.)
 Coronal postgadolinium T1-weighted MRI with fat saturation reveals diffuse, intense enhancement of the intraorbital mass (arrow).
Coronal postgadolinium T1-weighted MRI with fat saturation reveals diffuse, intense enhancement of the intraorbital mass (arrow).
 Axial postgadolinium T1-weighted MRI with fat saturation reveals diffuse, intense enhancement of the intraorbital mass. The lesion is confined to the orbit.
Axial postgadolinium T1-weighted MRI with fat saturation reveals diffuse, intense enhancement of the intraorbital mass. The lesion is confined to the orbit.
 Axial postgadolinium T1-weighted MRI with fat saturation in a 6-year-old girl demonstrates enhancement of the intracranial optic nerve (arrow), which is slightly expanded.
Axial postgadolinium T1-weighted MRI with fat saturation in a 6-year-old girl demonstrates enhancement of the intracranial optic nerve (arrow), which is slightly expanded.
A diagnosis of NF-1 may be supported by several findings including the following:
-
Spongiform changes (hyperintensity on T2-weighted images) in the cerebellum, brain stem, basal ganglia, thalamus, periventricular white matter, and corpus callosum
Adult lesions may involve the orbital, intracanalicular, or prechiasmal portions of the optic nerve, resulting in enlargement; they may exhibit retrochiasmatic extension as well. (See the images below.)
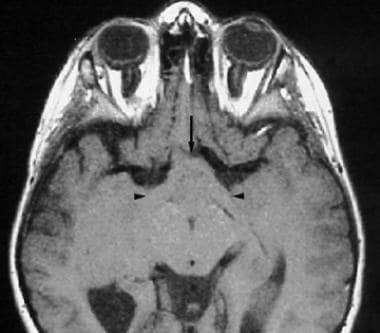 Axial noncontrast T1-weighted MRI in a 46-year-old man demonstrates enlargement of both optic tracts (arrowheads) and the optic chiasm (arrow).
Axial noncontrast T1-weighted MRI in a 46-year-old man demonstrates enlargement of both optic tracts (arrowheads) and the optic chiasm (arrow).
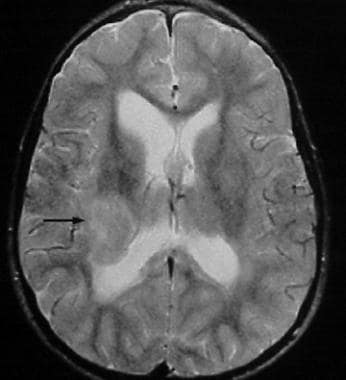 Axial T2-weighted MRI in a 46-year-old man demonstrates a mass in the lateral geniculate nucleus of the thalamus resulting from contiguous extension of the patient's known optic nerve glioma.
Axial T2-weighted MRI in a 46-year-old man demonstrates a mass in the lateral geniculate nucleus of the thalamus resulting from contiguous extension of the patient's known optic nerve glioma.
-
Coronal noncontrast T1-weighted MRI reveals a large intraorbital mass (arrow) centered on the optic nerve.
-
Coronal postgadolinium T1-weighted MRI with fat saturation reveals diffuse, intense enhancement of the intraorbital mass (arrow).
-
Axial postgadolinium T1-weighted MRI with fat saturation reveals diffuse, intense enhancement of the intraorbital mass. The lesion is confined to the orbit.
-
Axial postgadolinium T1-weighted MRI with fat saturation in a 6-year-old girl demonstrates enhancement of the intracranial optic nerve (arrow), which is slightly expanded.
-
Axial noncontrast T1-weighted MRI reveals bilateral, fusiform enlargement of the optic nerves (arrows) in a 14-year-old patient with neurofibromatosis type 1, consistent with bilateral optic nerve gliomas.
-
Axial noncontrast T1-weighted MRI in a 46-year-old man demonstrates enlargement of both optic tracts (arrowheads) and the optic chiasm (arrow).
-
Axial T2-weighted MRI in a 46-year-old man demonstrates a mass in the lateral geniculate nucleus of the thalamus resulting from contiguous extension of the patient's known optic nerve glioma.