Practice Essentials
Multicystic dysplastic kidney (MCDK) is a congenital maldevelopment in which the renal cortex is malformed and characterized by numerous cysts of multiple sizes. [1, 2, 3, 4] A dysplastic parenchyma anchors the cysts, the arrangement of which resembles a bunch of grapes. The calyceal drainage system is absent. Typically, MCDK is a unilateral disorder; the bilateral condition is incompatible with life. [5] Furthermore, MCDK with contralateral renal agenesis does not support life. [6] Multicystic dysplastic kidney is the most common cause of an abdominal mass in the newborn and is the most common cystic malformation of the kidney in infants. [7] Genetic aberrations have been detected in some cases. [8]
Several forms of MCDK have been described. The classic type and the less common hydronephrotic type have cysts of various sizes connected by loose, insubstantial fibrous tissue. No functional renal tissue can be identified. The classic type has a random configuration of cysts, whereas the hydronephrotic type presents with a discernible, dilated renal pelvis surrounded by cysts. Some sources identify a third type, known as solid cystic dysplasia. Solid cystic dysplasia is composed of smaller cysts with a greater amount of nonfunctional parenchyma. [9]
MCDK should not be confused with polycystic kidney disease (PCKD) or other renal cystic diseases. [10] Spence recognized MCDK as a distinct entity in 1955. [11] The Urology Section of the American Academy of Pediatrics established the National Multicystic Kidney Registry, which is a large, multicenter, longitudinal database that has helped clarify the appropriate management of MCDK.
MCDK can be associated with ipsilateral ureterocele, which is believed to cause renal malformation due to early obstruction during nephrogenesis. [12] It can occur in a segment of a duplicated kidney or in renal fusion anomalies. [13]
(See the image below.)
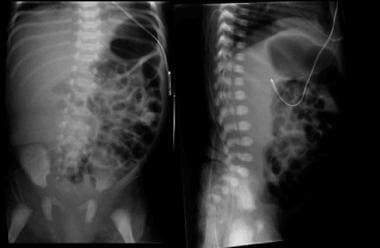 Kidney, ureter, and bladder (KUB) images of an infant with a right multicystic dysplastic kidney demonstrate displacement of bowel loops away from the right abdomen.
Kidney, ureter, and bladder (KUB) images of an infant with a right multicystic dysplastic kidney demonstrate displacement of bowel loops away from the right abdomen.
Imaging modalities
Ultrasonography is the preferred initial examination. [14] Prenatal ultrasound has been shown to have a diagnostic accuracy of over 90%. [15, 16, 17] Antenatally, MCDK is one of the most common renal anomalies detected during ultrasound examination, with an incidence of between 1 in 1000 and 1 in 4300 live births. The diagnosis of MCDK is often made antenatally, with multiple small cysts becoming evident as early as the 15th week of gestation. [18] In patients with a prenatal presentation, postnatal studies are required to differentiate MCDK from hydronephrosis. A sonogram should be obtained before a neonate is discharged from the nursery when MCDK is suspected. Reduced renal function and relative dehydration of the neonate should have no bearing on the detection of MCDK; therefore, there is no need to delay the initial sonogram. [19, 20, 21]
In a patient with a symptomatic presentation, such as a palpable abdominal mass, abdominal pain, incontinence, and recurrent urinary tract infections, ultrasonography should be the initial study. [22] The ultrasound information provides clues of other urinary tract anomalies, as well as intra-abdominal or retroperitoneal malignancies.
MCDK can be detected on other forms of imaging, but ultrasonography is fast and accurate, and it does not require sedation, radiation, or other interventions. Radionuclide imaging can be used to further differentiate the hydronephrotic form of MCDK from an obstruction in a functioning, severely hydronephrotic kidney. Radionuclide imaging provides information about the function of the involved renal unit and is superior to intravenous pyelography (IVP) in children.
The hydronephrotic form of MCDK can mimic ureteropelvic junction obstruction (UPJO), and radionuclide scanning is necessary following ultrasonography to confirm the diagnosis. Technetium-99m (99mTc) mercaptoacetyltriglycine (MAG-3) and 99mTc dimercaptosuccinic acid (DMSA) studies can demonstrate lack of function in the affected kidney, but MAG-3 studies can also provide information regarding drainage in an obstructed hydronephrotic kidney. Renal function is relatively poor in the first month of life, and radionuclide imaging should be postponed until 1 month of age to avoid false-positive results.
Voiding cystourethrography (VCUG) may be indicated in patients with MCDK to evaluate the urinary tract for vesicoureteral reflux (VUR) and other anomalies. Historically, there was greater emphasis on universal screening for VUR in all cases in order to prevent contralateral renal injury. [23] However, recent trends have seen an ebb in the call for VCUG, particularly in children with a normal contralateral kidney, as high grade VUR is rarely found. [24]
Radiography
Incidental findings on kidney, ureter, and bladder (KUB) images include displacement of the bowels when the affected kidney is enlarged (see the image below). Also, ringlike calcifications of the cyst walls may be seen on plain images. Retrograde pyelography may demonstrate an atretic or absent ureter.
 Kidney, ureter, and bladder (KUB) images of an infant with a right multicystic dysplastic kidney demonstrate displacement of bowel loops away from the right abdomen.
Kidney, ureter, and bladder (KUB) images of an infant with a right multicystic dysplastic kidney demonstrate displacement of bowel loops away from the right abdomen.
Voiding cystourethrography (VCUG) may be indicated in patients with MCDK to evaluate the urinary tract for vesicoureteral reflux (VUR) and other anomalies, including an ipsilateral ureterocele, which is found in some cases. [23, 24]
Magnetic Resonance Imaging
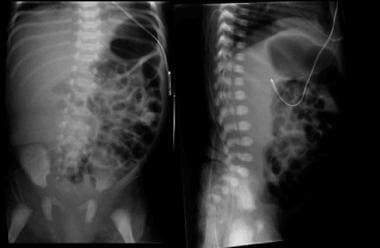
MCDK can be an incidental finding on magnetic resonance imaging (MRI) scans, but MRI is not part of the diagnostic investigation. MRIs show the typical multicystic appearance of MCDK with little or no parenchyma. [25, 26]
(See the images below.)
 A T2-weighted MRI scan demonstrates multiple cysts without normal renal parenchyma. A normal left kidney can be seen on the other side of the spine.
A T2-weighted MRI scan demonstrates multiple cysts without normal renal parenchyma. A normal left kidney can be seen on the other side of the spine.
 A T2-weighted MRI scan of the same patient as in the previous image demonstrates multiple cysts without normal renal parenchyma.
A T2-weighted MRI scan of the same patient as in the previous image demonstrates multiple cysts without normal renal parenchyma.
In a study by Jii et al, fetal MRI was found to add additional diagnostic information to prenatal US in the assessment of MCDK. MRI correctly changed the ultrasound diagnosis in 12 of 55 cases. All 55 cases were performed at 1.5 T magnetic resonance unit. MRI sequences, including steady-state free precession (SSFP), single-shot fast spin echo (SSFSE), T1-weighted imaging (T1WI), and diffusion weighted imaging (DWI) sequences. [26]
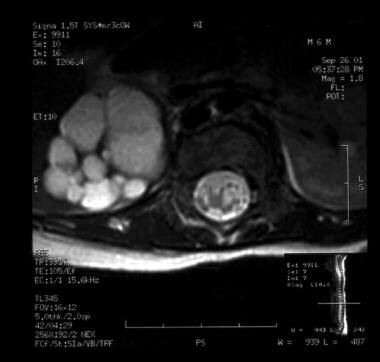
Ultrasonography
Prenatal imaging findings (see the images below) include hypoechoic cysts of variable sizes and shapes, interfaces between cysts, a nonmedial location of large cysts, the absence of an identifiable renal sinus, a lack of communication between cysts on sonograms, and minimal surrounding parenchyma. [27] Only 20% of MCDKs have an identifiable reniform shape (compared with 90% of hydronephrotic kidneys). Bilateral MCDK may occur with oligohydramnios as a result of poor urine production. The cysts of MCDK may become enlarged, may shrink, or may involute during fetal life. [19, 20, 21, 17]
Antenatally, MCDK is one of the most common renal anomalies detected during ultrasound examination, with an incidence of between 1 in 1000 and 1 in 4300 live births. The diagnosis of MCDK is often made antenatally, with multiple small cysts becoming evident as early as the 15th week of gestation. [18]
 A coronal prenatal sonogram of the retroperitoneum shows both kidneys. The cystic hypoechoic area is the right multicystic kidney. The normal kidney looks slightly hypoechoic and lobulated.
A coronal prenatal sonogram of the retroperitoneum shows both kidneys. The cystic hypoechoic area is the right multicystic kidney. The normal kidney looks slightly hypoechoic and lobulated.
 A prenatal sonogram shows the right multicystic dysplastic kidney in a longitudinal view. The spine underlies the affected kidney.
A prenatal sonogram shows the right multicystic dysplastic kidney in a longitudinal view. The spine underlies the affected kidney.
If MCDK is indicated on prenatal sonograms, postnatal ultrasonography (shown in the images below) should be completed before the patient is discharged home from the hospital. The diagnostic criteria for postnatal ultrasonography are the same as those for prenatal ultrasonography. Associated urologic anomalies such as ispilateral ureterocele and fusion anomalies may also be detected.
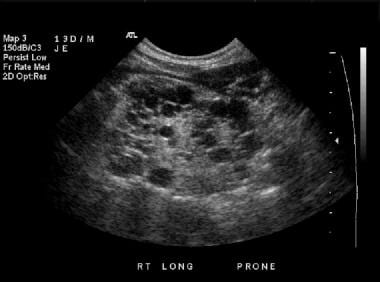 A longitudinal sonogram of the right kidney shows multiple diffuse hypoechoic renal cysts, without any significant normal renal parenchyma.
A longitudinal sonogram of the right kidney shows multiple diffuse hypoechoic renal cysts, without any significant normal renal parenchyma.
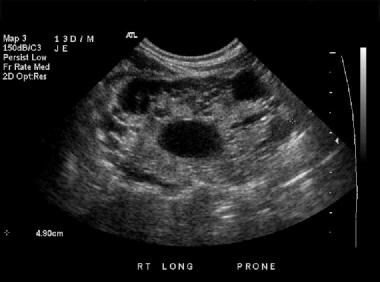 A Longitudinal sonogram of the right kidney shows multiple diffuse, hypoechoic renal cysts, without any significant normal renal parenchyma.
A Longitudinal sonogram of the right kidney shows multiple diffuse, hypoechoic renal cysts, without any significant normal renal parenchyma.
Degree of confidence
Ultrasonography is an excellent diagnostic test for MCDK, with a high degree of confidence. An obstructive uropathy with little renal parenchyma can mimic MCDK, but radionuclide studies can provide confirmation of the diagnosis. Autosomal recessive PCKD is not usually mistaken for MCDK, as the cysts in PCKD are too small to be visualized on ultrasonograms, and the parenchyma is generally homogeneously hyperechoic. Other renal cystic diseases typically appear with some functional parenchyma. Hepatic cysts are not seen in association with MCDK.
The greatest source of false-positive errors occurs in the setting of hydronephrosis or UPJO. A reniform shape and/or a large cystic structure in the medial portion of the kidney are more indicative of hydronephrosis than MCDK. Unlike in hydronephrosis, where there is communication with the central renal pelvis, the cysts of the classic form of MCDK do not communicate.
Regarding false-negative results, renal agenesis with nonrenal cystic structures in the retroperitoneum (eg, an adrenal cystic mass) could potentially be mistaken for MCDK.
Nuclear Imaging
Nuclear renograms are used to evaluate the perfusion, function, and drainage of the kidneys, as there is uptake of the radiotracer into a functioning kidney and excretion into the renal pelvis, ureter, and bladder. In the area of the MCDK, a photopenic region is present that represents displaced tissue with background activity only. [19]
(See the images below.)
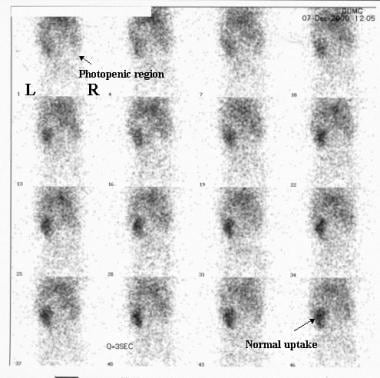 Initial perfusion images from a nuclear renal scan. Note the normal uptake and concentration of the radiotracer in the left kidney. No uptake or concentration of radiotracer is seen in the right MCDK, leaving a photopenic area in the right renal fossa.
Initial perfusion images from a nuclear renal scan. Note the normal uptake and concentration of the radiotracer in the left kidney. No uptake or concentration of radiotracer is seen in the right MCDK, leaving a photopenic area in the right renal fossa.
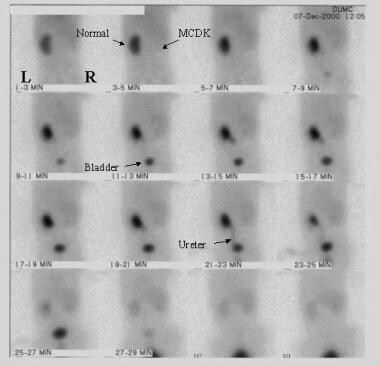 More delayed images from the same renal scanning examination as in the previous image shows a concentration of radiotracer in the normal left kidney and excretion into the left ureter and bladder. Uptake of radiotracer in the right multicystic dysplastic kidney is minimal.
More delayed images from the same renal scanning examination as in the previous image shows a concentration of radiotracer in the normal left kidney and excretion into the left ureter and bladder. Uptake of radiotracer in the right multicystic dysplastic kidney is minimal.
Degree of confidence
Nuclear medicine studies are the best imaging studies for differentiating between MCDK and hydronephrosis; however, severe hydronephrosis with poor renal function may still be difficult to distinguish from MCDK. The similarity may not be clinically relevant because reconstructive surgery is usually not indicated in the setting of poor (ie, < 10-15%) differential function.
MAG-3, diethylenetriamine-pentaacetic acid (DTPA), and dimercaptosuccinic acid (DMSA) are the preferred agents. Tests with these agents are sensitive for detecting renal function, but the anatomic resolution is relatively poor. Other forms of imaging are required to visualize the specific anatomy of the kidney.
False positives/negatives
On a nuclear renogram, anything that impairs the renal circulation, such as a renal artery stenosis or a renal vein thrombosis, appears as a nonfunctioning kidney; nevertheless, the renal parenchyma should appear relatively normal with ultrasonography. In addition, renal agenesis may mimic the nonfunctioning kidney of MCDK, but the tissue is absent on ultrasonograms.
False-negative results may arise in the setting of severe hydronephrosis. In a poorly functioning kidney, the intervention is the same as in MCDK; therefore, discriminating between these 2 disorders may not be imperative.
-
Kidney, ureter, and bladder (KUB) images of an infant with a right multicystic dysplastic kidney demonstrate displacement of bowel loops away from the right abdomen.
-
A coronal prenatal sonogram of the retroperitoneum shows both kidneys. The cystic hypoechoic area is the right multicystic kidney. The normal kidney looks slightly hypoechoic and lobulated.
-
A prenatal sonogram shows the right multicystic dysplastic kidney in a longitudinal view. The spine underlies the affected kidney.
-
A longitudinal sonogram of the right kidney shows multiple diffuse hypoechoic renal cysts, without any significant normal renal parenchyma.
-
A Longitudinal sonogram of the right kidney shows multiple diffuse, hypoechoic renal cysts, without any significant normal renal parenchyma.
-
Initial perfusion images from a nuclear renal scan. Note the normal uptake and concentration of the radiotracer in the left kidney. No uptake or concentration of radiotracer is seen in the right MCDK, leaving a photopenic area in the right renal fossa.
-
More delayed images from the same renal scanning examination as in the previous image shows a concentration of radiotracer in the normal left kidney and excretion into the left ureter and bladder. Uptake of radiotracer in the right multicystic dysplastic kidney is minimal.
-
A T2-weighted MRI scan demonstrates multiple cysts without normal renal parenchyma. A normal left kidney can be seen on the other side of the spine.
-
A T2-weighted MRI scan of the same patient as in the previous image demonstrates multiple cysts without normal renal parenchyma.





