Practice Essentials
Elbow fractures and dislocations are commonly seen in the acute care setting. In adults, elbow dislocation is the second most common dislocation after that of the shoulder; in children, elbow dislocation is the most common dislocation. Elbow factures can be either extra-articular or intra-articular. Extra-articular fractures include intercondylar, supracondylar, epicondylar, and condyle, whereas intra-articular fractures include those of the trochlea, capitellum, radial head, and olecranon. [1, 2, 3, 4, 5, 6]
Preferred examination
It has been suggested that radiologic imaging studies may be unnecessary for the evaluation of elbow fractures and dislocations if the active range of motion (including extension, flexion, supination, and pronation) remains normal. [7, 8] An alternative clinical prediction rule by Arundel et al maintains that, in the adult elbow, fracture is excluded and imaging is therefore unnecessary if the patient has normal full elbow extension; absence of bruising; and lack of tenderness over the radial head, olecranon, and medial epicondyle. [9] Arundel et al suggest that clinical gestalt is sensitive for detecting fractures but that the clinical prediction rule increases specificity (identifying which adults do not need imaging), decreasing the number of negative radiographs. [9]
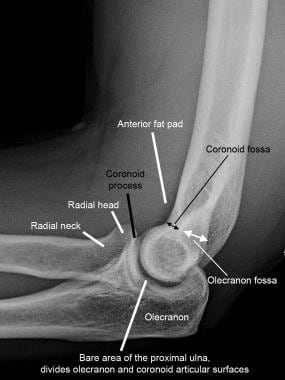
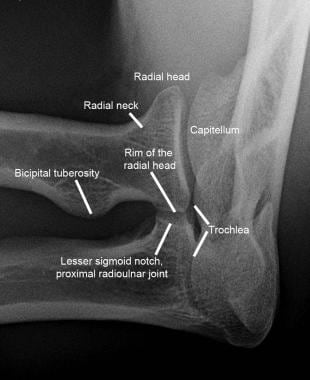
The majority of acute elbow conditions encountered in the emergency setting can be diagnosed on conventional radiographs. The minimal radiographic series includes anteroposterior (AP) and lateral images, while an oblique radial head–capitellar view can help detect subtle fractures by removing osseous overlap of the radial head and coronoid. [10] Examples of all 3 views, with anatomy labeled, are shown in the 3 images below. The radial head–capitellar view may be acquired only when a radial head fracture is suspected, or it may be performed routinely for acute elbow pain or trauma.
 Normal elbow. Normal anteroposterior (AP) radiograph of the elbow with labeling of relevant anatomy.
Normal elbow. Normal anteroposterior (AP) radiograph of the elbow with labeling of relevant anatomy.
Radiographs of the elbow and wrist can exclude malalignment of the elbow joint and distal radioulnar joint (DRUJ). Neurovascular status should be determined because the brachial artery and ulnar and median nerves may be entrapped. [1]
The technologist may be more adept at performing this view and, therefore, more likely to produce a high-quality radiograph when it is needed, if he or she performs them frequently. Optimal elbow radiographic technique requires the patient to tolerate, and cooperate with, full extension of the elbow for the frontal projection and 90° of flexion for the lateral and oblique views, positions that may be difficult in the acutely traumatized elbow. Splints and other materials included on the radiograph may also adversely affect the image quality.
On radiographs, a line drawn along the anterior cortex of the distal humerus, the anterior humeral line, is said to intersect the middle third of the capitellum. [6] This sign was originally described by Lee Rogers in 1978 in the evaluation of a pediatric elbow for subtle supracondylar fractures. [11] Similarly, the radiocapitellar line, drawn along the long axis of the radial neck, should bisect the capitellum on all projections.
(See the image below.)
 Normal elbow. Anterior humeral line and radiocapitellar line on normal lateral radiograph. The anterior humeral line is drawn along the anterior cortex of the distal humeral shaft and should bisect the middle third of the capitellum. The radiocapitellar line is parallel to the long axis of the radial neck and should bisect the capitellum. These were originally reported for evaluation of the pediatric elbow and have not been validated in adults.
Normal elbow. Anterior humeral line and radiocapitellar line on normal lateral radiograph. The anterior humeral line is drawn along the anterior cortex of the distal humeral shaft and should bisect the middle third of the capitellum. The radiocapitellar line is parallel to the long axis of the radial neck and should bisect the capitellum. These were originally reported for evaluation of the pediatric elbow and have not been validated in adults.
In distinction, elevation of the anterior and posterior fat pads is a reliable indicator of elbow effusion, which, in the setting of acute elbow trauma, should be considered evidence of an acute intra-articular fracture. The radiographic anterior fat pad represents the superimposed radial and coronoid fat pads lying side by side along the anterior surface of the distal humerus within their respectively named shallow humeral fossae. [12] In their normal positions, the superimposed anterior fat pads are seen as a triangular or convex fat density along the anterior distal humerus. When a joint effusion distends the joint capsule, the fat pads are lifted superiorly with convex deep contour, the “spinnaker sail sign," as shown in the image below. [13]
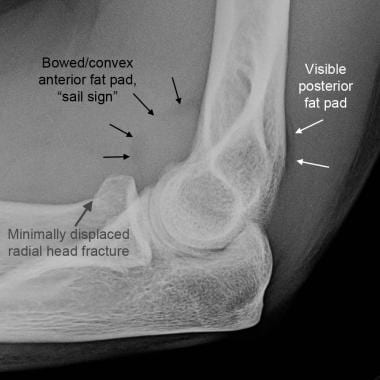 Elbow, fractures and dislocations. Elbow effusion with associated fat-pad elevation in the setting of radial head fracture. The anterior fat pad is elevated, and its undersurface is convex, giving the "spinnaker sail sign." The posterior fat pad is elevated out of the deep olecranon fossa and is visible just above the cortex of the distal humerus.
Elbow, fractures and dislocations. Elbow effusion with associated fat-pad elevation in the setting of radial head fracture. The anterior fat pad is elevated, and its undersurface is convex, giving the "spinnaker sail sign." The posterior fat pad is elevated out of the deep olecranon fossa and is visible just above the cortex of the distal humerus.
The posterior fat pad normally resides within the much deeper olecranon fossa along the extensor surface of the distal humerus, compressed by the triceps and anconeus muscles during elbow flexion, and it is therefore not seen on a normal lateral elbow radiograph. [12, 14, 15] When elbow effusion elevates the fat pad out of the fossa, it becomes visible posterior to the humerus. Alternatively, the fat pad may be displaced out of the fossa by the olecranon in the otherwise normal, but extended, elbow. Care should be exercised when interpreting fat-pad elevation on a poorly positioned lateral elbow radiograph.
A posttraumatic elbow effusion is most often assumed to be a sign of lipohemarthrosis from acute fracture; however, depending on the clinical setting, effusion could instead be due to hemarthrosis, inflammatory/crystalline arthropathy, or infection. [14] If necessary, advanced imaging or fluid analysis may confirm the diagnosis.
CT scanning is helpful in some patients to further characterize fractures and alignment before surgery, and it can be performed after reduction and splinting.
MRI is widely used in cases of chronic elbow pain but has limited use for acute elbow trauma. In cases of continued pain despite conservative management, MRI can be invaluable for assessing collateral ligaments, common flexor and extensor tendon origins, articular cartilage, and occult bone lesions. [16, 17]
Ultrasound can be used acutely for diagnosis and preoperative localization of ruptured biceps and triceps tendons. In such cases, comparison to the normal contralateral side may be helpful. However, ultrasound examination depends on operator experience and skill to perform and interpret. [18, 15]
Conventional angiography may be considered for assessing and treating the brachial artery at the elbow. Transection, thrombosis, dissection, and intimal flaps may be found.
Pearls
Optimize radiographic technique, especially on the lateral view. Exclusion of anatomy, overlying materials, or elbow extension and/or rotation can all impair one’s ability to detect fat-pad elevation, the most sensitive indicator of intra-articular injuries.
Look for fat-pad elevation on every lateral radiograph. An elevated posterior fat pad is never normal, and a fracture or ligamentous injury must be suspected if it is detected. If radiographs are otherwise negative, conservative treatment with follow-up radiographs in 7-10 days is appropriate.
Obtain the radial head–capitellar oblique view routinely, but carefully scrutinize this view in patients with tenderness at the radial head. Fractures involving the radial head, capitellum, or coronoid process may only be visible on this view.
When a fracture is detected, double-check alignment. Fractures are not infrequently associated with dislocations (eg, Monteggia fracture-dislocation) or instability from ligamentous injuries. These complex injuries are more surgically challenging.
Check for fractures after reduction of the elbow dislocation. Missed coronoid process fractures can lead to chronic instability.
Image the forearm/wrist if a fracture or dislocation is detected at the elbow. This helps detect any concomitant injuries to the osseous ring of the forearm.
Radiography
Elbow dislocations
Dislocations of the elbow are second in frequency only to dislocations of the shoulder in adults and are the most common dislocations in children. [2] Most elbow dislocations result from falling on an outstretched hand (FOOSH) with extended elbow and are therefore posterior. Anterior, medial, lateral, and divergent types also occur. Dislocations are almost always accompanied by disruption of most or all of the components of the capsuloligamentous complex. An elbow occasionally dislocates without fracture (simple dislocation), as shown in the image below.
 Elbow, fractures and dislocations. Posterior dislocation of the elbow without fractures. Note malalignment of the radiocapitellar line and ulnotrochlear joints.
Elbow, fractures and dislocations. Posterior dislocation of the elbow without fractures. Note malalignment of the radiocapitellar line and ulnotrochlear joints.
Complex elbow dislocations have associated fractures that further compromise joint stability. The most common associated fractures are those of the radial head and coronoid process, which, in the setting of posterior elbow dislocation, has been termed the “terrible triad of the elbow,” as shown in the image below. [19] On plain radiographs, the oblique view provides visualization of the radial head and coronoid process, and the anteroposterior view may demonstrate an avulsion fracture of the lateral epicondyle, suggesting lateral ulnar collateral ligament injury. [1]
 Elbow, fractures and dislocations. "Terrible triad of the elbow." Lateral elbow radiograph shows posterior fat-pad elevation (white arrowhead), widening of ulnotrochlear joint (short white lines), and fractures of the radial head (black arrow) and coronoid process (white arrows). Subtle posterior subluxation of the proximal radius relative to the capitellum also can be seen.
Elbow, fractures and dislocations. "Terrible triad of the elbow." Lateral elbow radiograph shows posterior fat-pad elevation (white arrowhead), widening of ulnotrochlear joint (short white lines), and fractures of the radial head (black arrow) and coronoid process (white arrows). Subtle posterior subluxation of the proximal radius relative to the capitellum also can be seen.
Monteggia fracture-dislocations, as shown in the image below, are another common form of complex fracture-dislocation. These include a combination of proximal ulnar shaft fracture and radial head dislocation (without or with fracture).
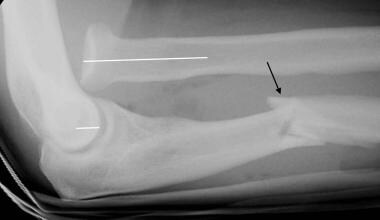 Elbow, fractures and dislocations. Monteggia fracture-dislocation of the elbow. Lateral elbow radiograph shows anterior radial head dislocation (with discontinuity of radiocapitellar line, white line) and an apex-anterior proximal ulnar shaft fracture (black arrow). This would be classified as Bado type I, the most common Bado subtype of Monteggia injuries.
Elbow, fractures and dislocations. Monteggia fracture-dislocation of the elbow. Lateral elbow radiograph shows anterior radial head dislocation (with discontinuity of radiocapitellar line, white line) and an apex-anterior proximal ulnar shaft fracture (black arrow). This would be classified as Bado type I, the most common Bado subtype of Monteggia injuries.
They are classified by the Bado classification according to the direction of displacement and location of the ulnar fracture. The Table below summarizes the Bado classification system for Monteggia fracture-dislocations.
Table. Bado Classification of Monteggia Fracture-Dislocation [20] (Open Table in a new window)
Type |
Description |
Frequency, % |
I |
Ulnar fracture - Middle or proximal third Radial head - Anterior dislocation |
65 |
II |
Ulnar fracture - Middle or proximal third Radial head - Posterior dislocation |
18 |
III |
Ulnar fracture - Distal to coronoid process Radial head - Lateral dislocation |
16 |
IV |
Ulnar fracture - Middle or proximal third Radial head - Anterior dislocation plus fracture of proximal third of radius |
1 |
Additional upper extremity injuries resulting from the FOOSH-type mechanism can be seen at the wrist and shoulder in 10-15% of cases, [3] and these joints should therefore be imaged in the setting of all elbow fractures and dislocations. The Essex-Lopresti injury is an important, highly unstable variant in which a comminuted radial head fracture (without or with dislocation) is accompanied by tearing of the interosseous membrane and disruption of the distal radioulnar joint, as shown in the images below.
 Elbow, fractures and dislocations. Essex-Lopresti injury of the forearm. Anteroposterior (AP) elbow radiograph showing fracture of the radial neck (black arrows) and discontinuity of the radiocapitellar line (white lines) due to dislocation of the fractured radial head.
Elbow, fractures and dislocations. Essex-Lopresti injury of the forearm. Anteroposterior (AP) elbow radiograph showing fracture of the radial neck (black arrows) and discontinuity of the radiocapitellar line (white lines) due to dislocation of the fractured radial head.
 Elbow, fractures and dislocations. Anteroposterior (AP) wrist radiograph shows dislocation of the distal radioulnar joint (black arrowheads), and complete disruption of the interosseous ligament is therefore inferred. Incidentally, this patient also has perilunate fracture-dislocation with rotation of the lunate (L) and fracture through the scaphoid waist.
Elbow, fractures and dislocations. Anteroposterior (AP) wrist radiograph shows dislocation of the distal radioulnar joint (black arrowheads), and complete disruption of the interosseous ligament is therefore inferred. Incidentally, this patient also has perilunate fracture-dislocation with rotation of the lunate (L) and fracture through the scaphoid waist.
Diagnosis of elbow dislocation is usually made easily on radiographs, for which anteroposterior (AP) and lateral views are the most helpful. Associated fractures may be easier to see or localize on postreduction radiographs without splint material. The findings most typical of dislocation include malalignment of the radiocapitellar line and incongruity/widening of the ulnotrochlear joint.
Elbow fractures
Any of the 3 bones involved in the elbow joint can be fractured—the distal humerus, proximal ulna, and proximal radius—with several subcategories of each.
Fractures of the distal humerus
Fractures of the distal humerus are not uncommon in elderly osteoporotic patients. In younger adults, these fractures occur in the setting of high-energy trauma. Operative repair is usually preferred and, if possible, is best performed within 24 hours of injury. [21] Fractures of the distal humerus are broadly classified as extra-articular, intra-articular-unicondylar, and intra-articular-bicondylar.
Extra-articular distal humerus fractures: The supracondylar humerus is frequently fractured in children, but this is covered separately in Imaging in Pediatric Elbow Trauma. In contrast, extra-articular distal humeral fractures are unusual in adults. They can result from hyperextension (FOOSH), hyperflexion (direct impact to flexed elbow), or adduction or abduction mechanisms. Most traverse the supracondylar segment of the distal humerus that is thinned by the radial, coronoid, and olecranon fossae. As this portion is intracapsular (though extra-articular), a joint effusion is common, and displaced free intra-articular fragments can be detected. Some fractures are even more distal, extending across the condyles proximal to the articular surface, which complicates placement of surgical hardware. A traction view, as shown below, is helpful to exclude subtle transcondylar extension in adults. Displaced fractures should be referred to an orthopedist.
 Elbow, fractures and dislocations. Comminuted extraarticular fracture of the distal humerus (white arrowheads), intersecting within the distal humeral fossae (*). This traction view was performed to exclude subtle intraarticular extension.
Elbow, fractures and dislocations. Comminuted extraarticular fracture of the distal humerus (white arrowheads), intersecting within the distal humeral fossae (*). This traction view was performed to exclude subtle intraarticular extension.
Intra-articular-unicondylar distal humerus fractures: These are oblique fractures that extend from the medial or lateral humeral shaft cortex across the distal articular surface, usually through the trochlear sulcus or the trochlear groove. This isolates either the trochlea or capitellum from the distal humerus. [22] The other humeral condyle, though, remains attached to the shaft. When the trochlea remains attached to the humerus and ulnotrochlear joint alignment is maintained, the capsuloligamentous complex is often intact and conservative treatment can be considered. Displacement of the radius and ulna with the fractured condyle, however, represents a fracture-dislocation of the elbow and requires surgical fixation because it is unstable. [22]
(See the image below.)
 Elbow, fractures and dislocations. Unstable unicondylar distal humeral fracture. Anteroposterior (AP) elbow radiograph shows comminuted fracture of the capitellum (black arrowheads). Disruption of the ulnotrochlear joint alignment (white arrows) indicates concomitant ligamentous injury that necessitates surgical repair. The injury is also open in this case.
Elbow, fractures and dislocations. Unstable unicondylar distal humeral fracture. Anteroposterior (AP) elbow radiograph shows comminuted fracture of the capitellum (black arrowheads). Disruption of the ulnotrochlear joint alignment (white arrows) indicates concomitant ligamentous injury that necessitates surgical repair. The injury is also open in this case.
Intra-articular-bicondylar or intercondylar distal humerus fractures: These are comminuted, often T-, Y-, or H-shaped, fractures of the distal humerus that result in separation of both the medial and lateral humeral condyles from each other and from the shaft. These fractures nearly always require surgery. The difficulty of repair depends on the complexity of fractures through the articular surface and through the metaphyseal cortices, as well as the vertical height of the metaphyseal fracture above the articular surface. Fractures that are more distal have a smaller zone for surgical plate placement. Free fragments of the trochlea (as shown below) are at risk for avascular necrosis. [22] The fractures usually intersect in the humeral fossae and are comminuted, resulting in small free intra-articular loose bodies. CT scanning may be helpful for preoperative planning.
 Elbow, fractures and dislocations. Comminuted bicondylar distal humeral fracture. Anteroposterior (AP) elbow radiograph shows fracture lines extending through the medial and lateral cortices of the distal humeral shaft, between the trochlea and capitellum, and between the trochlea and medial epicondyle (black arrows). Marked comminution is noted at the distal humeral fossae. The presence of the free trochlear fragment (outlined with white arrowheads) both increases difficulty of operative repair and increases risk of avascular necrosis.
Elbow, fractures and dislocations. Comminuted bicondylar distal humeral fracture. Anteroposterior (AP) elbow radiograph shows fracture lines extending through the medial and lateral cortices of the distal humeral shaft, between the trochlea and capitellum, and between the trochlea and medial epicondyle (black arrows). Marked comminution is noted at the distal humeral fossae. The presence of the free trochlear fragment (outlined with white arrowheads) both increases difficulty of operative repair and increases risk of avascular necrosis.
Fractures of the proximal ulna
Fractures of the proximal ulna can involve the olecranon, coronoid process, or proximal ulnar shaft, such as in Monteggia fracture-dislocation.
Olecranon process fractures: Fractures of the olecranon are not uncommon, representing 10% of all fractures in the upper extremity. Nondisplaced and minimally displaced fractures can be treated conservatively. If, however, displacement exceeds 3 mm or increases with elbow flexion, surgical repair is considered and becomes increasingly complex with the addition of comminution of the olecranon or collateral ligament instability, [23] as shown in the image below. These fractures are encountered with greater frequency in osteoporotic elderly patients and are often the result of a fall directly onto the elbow. The fracture and joint capsule may be open. [24, 25]
 Elbow, fractures and dislocations. Olecranon fracture. Lateral elbow radiograph demonstrates comminuted (*) fracture of the olecranon with more than 3 mm of distraction of the proximal fracture fragment (double-ended white arrow) by the triceps tendon. This usually requires surgical repair. The radiocapitellar joint appears widened (black arrow), raising concern for concomitant ligamentous injury, which could be confirmed intraoperatively.
Elbow, fractures and dislocations. Olecranon fracture. Lateral elbow radiograph demonstrates comminuted (*) fracture of the olecranon with more than 3 mm of distraction of the proximal fracture fragment (double-ended white arrow) by the triceps tendon. This usually requires surgical repair. The radiocapitellar joint appears widened (black arrow), raising concern for concomitant ligamentous injury, which could be confirmed intraoperatively.
Coronoid process fractures: Less than 1-2% of elbow fractures involve the coronoid process, and when present, these injuries are rarely isolated; they are more often associated with elbow dislocation, radial head fracture, or both (the terrible triad). [13] The coronoid process is essential for elbow stability. It acts as a bony constraint against posterior elbow dislocation. It also serves as the attachment site for the anterior joint capsule and fibers of the medial and lateral collateral ligaments and brachialis. Fractures involving more than 50% of the coronoid are particularly unstable. [26]
(See the images below.)
 Elbow, fractures and dislocations. Coronoid process fracture. Lateral elbow radiograph demonstrates a displaced fracture fragment (*) arising from the coronoid process (black arrowhead).
Elbow, fractures and dislocations. Coronoid process fracture. Lateral elbow radiograph demonstrates a displaced fracture fragment (*) arising from the coronoid process (black arrowhead).
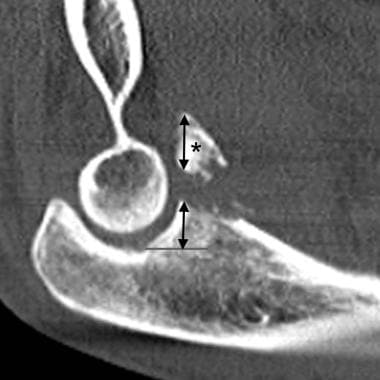 Elbow, fractures and dislocations. Coronoid process fracture. Sagittal CT image indicates that the coronoid fracture fragment (*) involves more than 50% of the coronoid height (double-ended arrows), increasing the risk of elbow instability if not repaired.
Elbow, fractures and dislocations. Coronoid process fracture. Sagittal CT image indicates that the coronoid fracture fragment (*) involves more than 50% of the coronoid height (double-ended arrows), increasing the risk of elbow instability if not repaired.
Fractures of the proximal radius
Radial head fractures are the most common fracture in the adult elbow, accounting for 30-56% of fractures. [13, 27] Most result from a FOOSH-type injury, but high-energy trauma can cause complex radial head fractures, often in combination with other elbow and upper extremity injuries. Nondisplaced and minimally displaced fractures can be treated conservatively with a sling and radiographic follow-up. [28] Since posttraumatic elbow effusion is most often due to a nondisplaced radial head fracture, these are treated the same way.
Treatment decisions
Several classification systems. The overriding principles are that nondisplaced or minimally displaced fractures are treated conservatively, while displaced fractures, comminuted fractures, fractures with block to passive range of motion, or those accompanied by other fractures and/or dislocation/instability require orthopedic referral for possible surgery.
An important consideration is the extent of involvement of the rim of the radial head, which articulates with the lesser sigmoid notch of the proximal ulna and enables the normal 180° range of motion of the forearm for supination and pronation. Fractures involving only a small portion of the lateral radial head margin (a third or less) likely spare the articulation and should not impair forearm motion. [29] Conversely, more extensive radial head and rim involvement, particularly if displaced and/or comminuted, is likely to impair forearm mobility. Surgery may entail fixation of the radial head/neck, radial head excision, or arthroplasty and depends on the severity of the fractures and integrity of the soft-tissue stabilizers of the elbow.
(See the images below.)
 Elbow, fractures and dislocations. Radial head fracture. Anteroposterior (AP) elbow radiograph shows a minimally displaced fracture of the lateral radial head, involving slightly more than half of the articular surface and radial head rim.
Elbow, fractures and dislocations. Radial head fracture. Anteroposterior (AP) elbow radiograph shows a minimally displaced fracture of the lateral radial head, involving slightly more than half of the articular surface and radial head rim.
Computed Tomography
CT scanning is helpful in select patients for further characterization of fractures and alignment prior to surgery and can be performed following reduction and splinting. If thin-section multidetector row CT (MDCT) is complemented with multiplanar reconstructions, the degree of confidence in the findings is high.
(See the image below.)
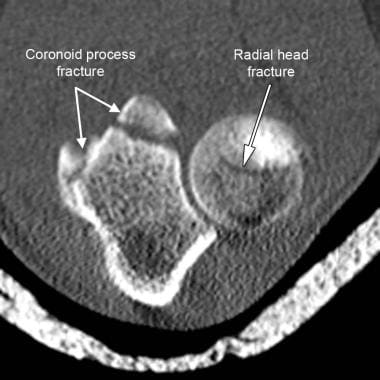 Elbow fractures and dislocations. Axial CT image was obtained post reduction and splinting for surgical planning purposes and shows acute fractures of the radial head and coronoid process.
Elbow fractures and dislocations. Axial CT image was obtained post reduction and splinting for surgical planning purposes and shows acute fractures of the radial head and coronoid process.
MDCT has been found to be helpful in identifying small fractures and impaction fractures associated with elbow dislocations. [30]
Upper extremity CT angiography may be useful if there are signs of brachial artery injury related to displaced fractures or dislocations of the elbow. CT findings may include transection, thrombosis, dissection, and intimal flaps. Conventional angiography can also show these findings but is invasive.
Magnetic Resonance Imaging
MRI is used widely in the setting of chronic elbow pain but has limited use in the setting of acute elbow trauma. It is generally used as a problem-solving tool in patients with continuing pain despite conservative management. In that case, it is invaluable in the assessment of collateral ligaments, common flexor and extensor tendon origins, articular cartilage, and occult bone lesions. MR arthrography may be used for evaluation of osteochondral lesions and their stability. [16, 17]
MRI can also be used acutely for diagnosis and presurgical planning of bicipital and tricipital tendon ruptures, although ultrasonography can also be used for this purpose.
(See the image below.)
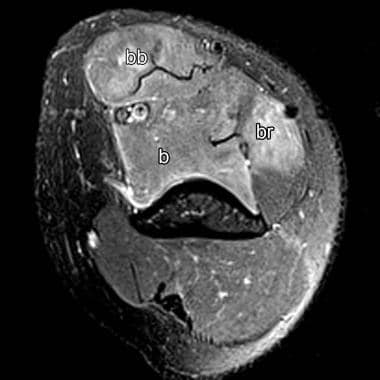 Elbow fractures and dislocations. Axial fat-suppressed T2 MRI through the distal humerus shows abnormal high T2 signal within the biceps brachii (bb), brachialis (b), and brachioradialis (br) muscle bodies, compatible with strain. Clinically, this mimicked biceps tendon rupture, but the tendon was found to be intact.
Elbow fractures and dislocations. Axial fat-suppressed T2 MRI through the distal humerus shows abnormal high T2 signal within the biceps brachii (bb), brachialis (b), and brachioradialis (br) muscle bodies, compatible with strain. Clinically, this mimicked biceps tendon rupture, but the tendon was found to be intact.
MRI has been used to identify the location and severity of ligamentous injuries after acute elbow dislocations. In one study, complete ligamentous tears were found to be more common on the medial side than on the lateral side. [16] MRI can also be used to assess the interosseous ligament when subtle Essex-Lopresti dissociation is suspected.
Ultrasonography
Ultrasound examination depends on operator experience and the skill necessary to perform and interpret. The increase in use of point-of-care US in the ED may allow more rapid diagnosis of elbow fracture, particularly in the pediatric population, in whom plain radiography may be difficult to interpret because of overlapping bones, growth plates, and maturing bones. [15]
In a study by Malahias et al, bedside ultrasound in the ED was found to to be sensitive for early (day 1) diagnosis of occult radial head fractures. According to the authors, it could be considered as an adjacent imaging modality in patients in whom radial head fracture is suspected when radiographs are negative. In this study of 23 patients with radial head fracture, US had 83.3% sensitivity, 60% specificity, 88.2% positive prognostic value, and 50% negative prognostic value (when at least one diagnostic US criterion was positive). Effusion in contact with the radial neck was the most sensitive sign. [18]
-
Normal elbow. Normal anteroposterior (AP) radiograph of the elbow with labeling of relevant anatomy.
-
Normal elbow. Normal lateral radiograph of the elbow with labeling of relevant anatomy.
-
Normal elbow. Normal oblique radiograph of the elbow with labeling of relevant anatomy.
-
Normal elbow. Anterior humeral line and radiocapitellar line on normal lateral radiograph. The anterior humeral line is drawn along the anterior cortex of the distal humeral shaft and should bisect the middle third of the capitellum. The radiocapitellar line is parallel to the long axis of the radial neck and should bisect the capitellum. These were originally reported for evaluation of the pediatric elbow and have not been validated in adults.
-
Elbow, fractures and dislocations. Elbow effusion with associated fat-pad elevation in the setting of radial head fracture. The anterior fat pad is elevated, and its undersurface is convex, giving the "spinnaker sail sign." The posterior fat pad is elevated out of the deep olecranon fossa and is visible just above the cortex of the distal humerus.
-
Elbow, fractures and dislocations. Posterior dislocation of the elbow without fractures. Note malalignment of the radiocapitellar line and ulnotrochlear joints.
-
Elbow, fractures and dislocations. "Terrible triad of the elbow." Lateral elbow radiograph shows posterior fat-pad elevation (white arrowhead), widening of ulnotrochlear joint (short white lines), and fractures of the radial head (black arrow) and coronoid process (white arrows). Subtle posterior subluxation of the proximal radius relative to the capitellum also can be seen.
-
Elbow, fractures and dislocations. Monteggia fracture-dislocation of the elbow. Lateral elbow radiograph shows anterior radial head dislocation (with discontinuity of radiocapitellar line, white line) and an apex-anterior proximal ulnar shaft fracture (black arrow). This would be classified as Bado type I, the most common Bado subtype of Monteggia injuries.
-
Elbow, fractures and dislocations. Essex-Lopresti injury of the forearm. Anteroposterior (AP) elbow radiograph showing fracture of the radial neck (black arrows) and discontinuity of the radiocapitellar line (white lines) due to dislocation of the fractured radial head.
-
Elbow, fractures and dislocations. Anteroposterior (AP) wrist radiograph shows dislocation of the distal radioulnar joint (black arrowheads), and complete disruption of the interosseous ligament is therefore inferred. Incidentally, this patient also has perilunate fracture-dislocation with rotation of the lunate (L) and fracture through the scaphoid waist.
-
Elbow, fractures and dislocations. Comminuted extraarticular fracture of the distal humerus (white arrowheads), intersecting within the distal humeral fossae (*). This traction view was performed to exclude subtle intraarticular extension.
-
Elbow, fractures and dislocations. Unstable unicondylar distal humeral fracture. Anteroposterior (AP) elbow radiograph shows comminuted fracture of the capitellum (black arrowheads). Disruption of the ulnotrochlear joint alignment (white arrows) indicates concomitant ligamentous injury that necessitates surgical repair. The injury is also open in this case.
-
Elbow, fractures and dislocations. Comminuted bicondylar distal humeral fracture. Anteroposterior (AP) elbow radiograph shows fracture lines extending through the medial and lateral cortices of the distal humeral shaft, between the trochlea and capitellum, and between the trochlea and medial epicondyle (black arrows). Marked comminution is noted at the distal humeral fossae. The presence of the free trochlear fragment (outlined with white arrowheads) both increases difficulty of operative repair and increases risk of avascular necrosis.
-
Elbow, fractures and dislocations. Olecranon fracture. Lateral elbow radiograph demonstrates comminuted (*) fracture of the olecranon with more than 3 mm of distraction of the proximal fracture fragment (double-ended white arrow) by the triceps tendon. This usually requires surgical repair. The radiocapitellar joint appears widened (black arrow), raising concern for concomitant ligamentous injury, which could be confirmed intraoperatively.
-
Elbow, fractures and dislocations. Coronoid process fracture. Lateral elbow radiograph demonstrates a displaced fracture fragment (*) arising from the coronoid process (black arrowhead).
-
Elbow, fractures and dislocations. Coronoid process fracture. Sagittal CT image indicates that the coronoid fracture fragment (*) involves more than 50% of the coronoid height (double-ended arrows), increasing the risk of elbow instability if not repaired.
-
Elbow, fractures and dislocations. Radial head fracture. Anteroposterior (AP) elbow radiograph shows a minimally displaced fracture of the lateral radial head, involving slightly more than half of the articular surface and radial head rim.
-
Elbow, fractures and dislocations. Radial head fracture. Postoperative radiograph shows this injury was treated with radial head replacement.
-
Elbow fractures and dislocations. Axial CT image was obtained post reduction and splinting for surgical planning purposes and shows acute fractures of the radial head and coronoid process.
-
Elbow fractures and dislocations. Axial fat-suppressed T2 MRI through the distal humerus shows abnormal high T2 signal within the biceps brachii (bb), brachialis (b), and brachioradialis (br) muscle bodies, compatible with strain. Clinically, this mimicked biceps tendon rupture, but the tendon was found to be intact.