Overview
In 1984, vertebroplasty was first successfully performed in France for the treatment of a cervical vertebral hemangioma (see image below). [1]
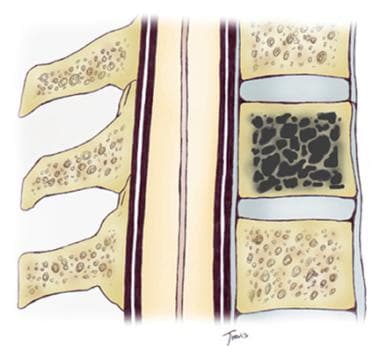 In a vertebral hemangioma, the fine trabeculae are replaced by venous channels, which predispose the patient to painful microfractures.
In a vertebral hemangioma, the fine trabeculae are replaced by venous channels, which predispose the patient to painful microfractures.
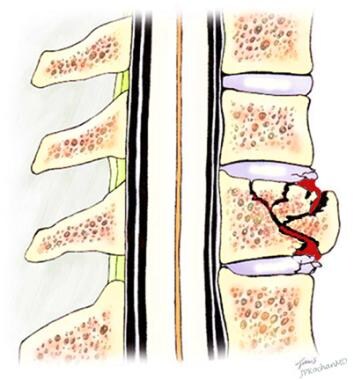
Since then, the application of vertebroplasty and kyphoplasty has expanded to include the treatment of the intense pain caused by vertebral compression fractures (see image below) that is refractory to conventional therapies such as analgesic use, bed rest, and bracing. Vertebroplasty may also be applied prophylactically to an at-risk vertebra between 2 other abnormal vertebra.
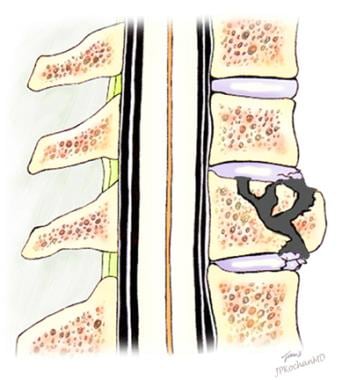
Vertebroplasty and kyphoplasty involve the injection of an acrylic cement under local anesthesia and either fluoroscopic guidance or, less commonly, CT guidance to control the pain of vertebral fractures associated with osteoporosis, tumors, and trauma (see image below). Typically, vertebroplasty is performed in an outpatient setting, while kyphoplasty typically requires hospital admission. Pain reduction or elimination is immediate, and the risk of complications is low. Neither vertebroplasty nor kyphoplasty is intended for the treatment of intervertebral disc disease or arthritis. [2]
Vertebroplasty is a treatment for pain. Theoretically, 2 mechanisms may account for the pain reduction associated with the injection of methylmethacrylate. The first mechanism may be as a result of acrylic fusion of the fragments into a single block, preventing the painful motion of the individual fracture fragments against each other. The second mechanism of pain reduction may be related to the heat produced by the polymerization process as the acrylic hardens. An added benefit is that deposition of acrylic within the vertebra significantly strengthens osteoporotic bone, reducing the likelihood of repeat fracture.
Vertebroplasty does not restore the height of the compressed vertebral body. A related procedure, kyphoplasty, is intended to restore lost height by inflating a balloon tamp within and between the fracture fragments prior to the infusion of methylmethacrylate. The procedures result in similar relief of pain due to vertebral compression fractures.
Fractures and osteoporosis
The fractures may be as a result of bone weakened by osteoporosis, trauma, or tumors such as metastases, multiple myeloma, and hemangioma. Osteoporosis, however, accounts for most fractures. The disease accounts for an estimated annual incidence of 700,000 fractures per year; of these, approximately 260,000 are vertebral compression fractures. Once a vertebral compression fracture occurs, the risk of additional fractures in adjacent vertebrae increases 5-fold.
Fractures are identified in 26% of women aged 50 years or older and are radiographically present at a rate of 500 cases per 100,000 persons in patients aged 50-54 years and 2,960 cases per 100,000 persons in patients older than 85 years. [3] Vertebral compression fractures are twice as common in females, [4] occurring in 153 females per 100,000 compared with 81 males per 100,000. Prevalence rates in North America for White women ≥ 50 years are 20–24%, with a White/Black ratio of 1.6. [5] For reasons not clearly understood, only one third of spinal compression fractures are painful; most of these are refractory to medical management. The remaining patients report a history of significant spinal pain in the past or do not have pain at the time of diagnosis.
Dozens of diseases and conditions predispose individuals to osteoporosis and secondary vertebral compression fracture. Examples include the following:
-
Advanced age
-
Oophorectomy, bilateral
-
Renal disease, chronic
-
Transplants
-
Tumors, parathyroid-related peptide
In addition, certain drugs are also associated with osteoporosis, as follows: [6]
-
Glucocorticoids
-
Proton pump inhibitors
-
Antiepileptic drugs
-
Medroxyprogesterone acetate
-
Aromatase inhibitors
-
GnRH agonists
-
Serotonin selective reuptake inhibitors
-
Thiazolidinediones
-
Calcineurininhibitors
-
Heparin
-
Warfarin
Patients with compression fractures typically present with a sudden onset of intense back pain, often after a relatively benign activity. Many patients refer to intractable pain after a sneeze or a cough. The pain tends to be debilitating. Patients find it difficult to find a comfortable position, and therefore, they have difficulty sleeping. Many patients refer to sleep in a seated or semireclining position.
Indications
Vertebroplasty and kyphoplasty are radiologic procedures for the treatment of the intense pain caused by vertebral compression fractures that is refractory to conventional therapies such as analgesic use, bed rest, and bracing.
Vertebroplasty may also be applied prophylactically to an at-risk vertebra between 2 other abnormal vertebrae.
Kyphoplasty is a refinement of the vertebroplasty procedure. In addition to the reduction of fracture-related pain, some or all of the height is restored to the compressed vertebral body.
Kyphoplasty is most effective with acute compression fractures secondary to either trauma or osteoporosis (vs fractures secondary to infection, solid tumors, or vascular lesions).
Contraindications
Because the injection of acrylic under pressure is likely to pass through the fracture into the spinal canal, a posterior cortical defect is considered a relative contraindication for vertebroplasty.
Vertebroplasty also is contraindicated in cases involving a bone infection such as diskitis with osteomyelitis.
Kyphoplasty is not recommended for the treatment of fractures secondary to infection, most solid tumors, and vascular lesions.
The presence of a burst fracture with loss of integrity of the posterior vertebral cortex and retropulsion of a fracture fragment into the spinal canal is considered exclusionary.
Kyphoplasty is not indicated for the treatment of degenerative disk or joint disease.
Anesthesia
Vertebroplasty is not painful and requires only mild sedation and analgesia.
Local, deep, periosteal and endosteal anesthesia is provided at the outset.
In selected patients, a preprocedural epidural block can further reduce procedural pain.
Occasionally, patients report pain when the trocar reaches the fracture fragments and when the injection of acrylic cement is initiated. Endosteal anesthesia appears to reduce the intensity of the pain, it but does not eliminate the pain entirely.
Technique
Imaging
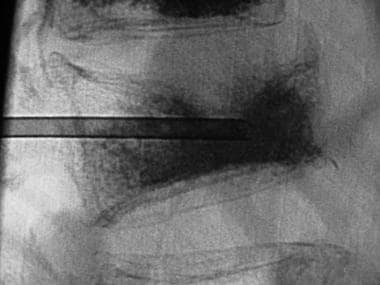
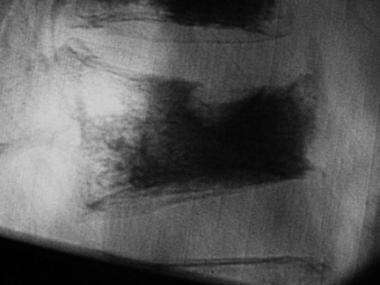
Most often, the radiographic diagnosis of compression fracture is made by using plain-film radiographs of the spine (see image below). MRI is essential in identifying cord compression as a consequence of a posteriorly displaced or retropulsed bone fragment. MRI findings are most informative in evaluating the spine at the levels where the spinal cord is present (eg, from the cervical spine through the second lumbar vertebra). CT is the most sensitive means of identifying a linear fracture through the posterior vertebral cortex. [7, 8, 9, 10]
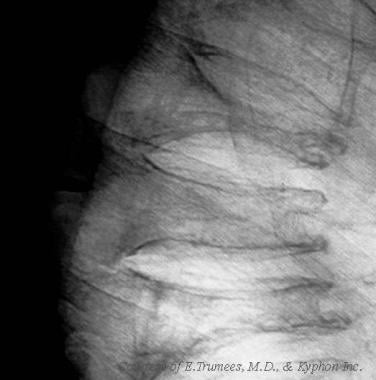 This image was obtained in an 80-year-old man with a steroid-induced osteoporosis and a painful acute midthoracic vertebral compression fracture. Several additional chronic fractures are also present.
This image was obtained in an 80-year-old man with a steroid-induced osteoporosis and a painful acute midthoracic vertebral compression fracture. Several additional chronic fractures are also present.
Nuclear medicine bone scanning is helpful in assessing metastatic disease and when pain is elicited on palpation at levels other than where a fracture is radiographically identified. The required imaging studies at Temple University Hospital include CT evaluation for fractures of the lumbar spine and both CT and MRI for fractures of the cervical and thoracic spine. Post procedural imaging of the treated levels is not considered cost effective and therefore infrequently obtained.
Patient selection
Inclusion criteria include the following: pain localized to a fracture or tumor, pain refractory to medical management, or a fracture less than 12 months old.
Exclusion criteria include the following: fracture extending to posterior vertebral cortex retropulsed fragment, cord compression, radiculopathy, fever and/or sepsis, or coagulopathy.
Technique
Vertebroplasty is a straightforward radiologic procedure that is performed on an outpatient basis in most institutions. The procedure is not painful and requires only mild sedation and analgesia, as described above in the Anesthesia section.
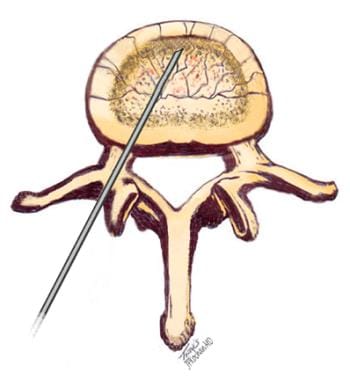
Lumbar vertebroplasty consists of the transpedicular placement of an 11-gauge bone biopsy needle into the affected vertebra under fluoroscopic or CT guidance (see images below). Thoracic vertebroplasty is performed via a transpedicular or peripedicular route by using a 13-gauge bone biopsy needle. Access to cervical lesions is via an anterolateral approach with a 13-gauge bone biopsy needle. Once positioned, methylmethacrylate is injected through the needle into the abnormal vertebral body.
The acrylic is then prepared under sterile conditions for injection. The dry, powdered polymer is mixed with barium and tantalum or tungsten, which makes the compound more visible during fluoroscopy. The polymer-metal admixture is then mixed with a liquid monomer of methylmethacrylate to a consistency similar to that of toothpaste. The acrylic cement is then injected with either a 1-mL Luer-Lok syringe or high-pressure torque handle syringe through the trocar. Injection is continued until complete opacification of the vertebral body is achieved or the first sign of extension into the epidural venous plexus appears. See image below.
Opacification of the paraspinous veins is common. When opacification occurs, the injection of acrylic is suspended for approximately 1 minute to allow the cement to harden within the vein. Injection may then be resumed, and the acrylic follows a new path of lower resistance. Opacification of the vertebral body need not be complete for successful vertebroplasty. If the acrylic reaches both the superior and inferior endplates and extends across midline, approximately 80% of the load-bearing benefit of a completely opacified vertebral body is achieved. [11] See image below.
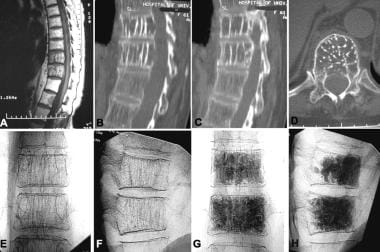 Two adjacent vertebral hemangiomas causing continuous back pain as seen by MRI (A) and CT (B, C, D). Fluoroscopic appearance prevertebroplasty (E, F) and postvertebroplasty (G, H). The patient's pain had abated by the end of the procedure.
Two adjacent vertebral hemangiomas causing continuous back pain as seen by MRI (A) and CT (B, C, D). Fluoroscopic appearance prevertebroplasty (E, F) and postvertebroplasty (G, H). The patient's pain had abated by the end of the procedure.
A small amount of methylmethacrylate is retained on the bench as a control. After approximately 10 minutes, the cement solidifies and becomes harder than the native bone. Once the control sample has solidified, the patient can be safely transferred to a stretcher. After the procedure, the patient remains supine for 1 hour; then, he or she can be discharged. Postprocedural medications are limited to Flexeril for muscle spasm and Tylenol for incisional pain.
Although no cases of infection are reported in the literature, the use of antibiotics in this institution is routine. All patients are pretreated with either 1 g of Ancef or 500 mg of vancomycin. In addition, in severely immunosuppressed patients, as much as 1.2 g of tobramycin can be added to the acrylic admixture in an attempt to further minimize the risk of infection. Other institutions perform vertebroplasty without apparent adverse results. The author believes that the benefit of antibiotic therapy outweighs the potential risk.
Kyphoplasty
Kyphoplasty is a refinement of the vertebroplasty procedure. In addition to the reduction of fracture-related pain, some or all of the height is restored to the compressed vertebral body. Normalizing the height of the fractured vertebra reduces the focally exaggerated curvature of the spine (ie, kyphosis). This effect, in turn, results in an esthetic improvement, improved posture, and a reduced risk of fracture of the adjacent vertebra as a result of abnormal load bearing. The restoration of a more normal appearing configuration of the vertebral body and improvement in the load-bearing physics is accomplished with the intravertebral inflation of 1 or 2 high-pressure balloon tamps (KyphX; Kyphon). As with vertebroplasty, access is via a transpedicular or peripedicular approach. The procedure distracts the fragments and elevates the collapsed vertebral endplate. The inflated balloons create cavities in the vertebral body, the margins of which are lined by the displaced, fragmented trabeculae.
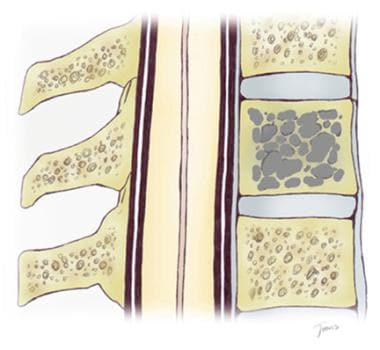
In kyphoplasty, a KyphX inflatable bone tamp is percutaneously advanced into the collapsed vertebral body (A). It is then inflated, (B) elevating the depressed endplate, creating a central cavity, and compacting the remaining trabeculae to the periphery. Once the balloon tamp is deflated and withdrawn, the cavity (C) is filled under low pressure with a viscous preparation of methylmethacrylate (D). See image below.
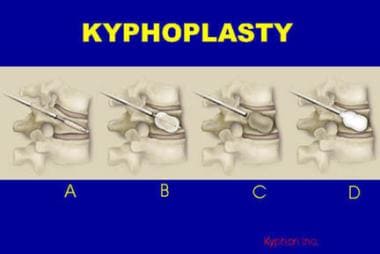 In kyphoplasty, a KyphX inflatable bone tamp is percutaneously advanced into the collapsed vertebral body (A). It is then inflated, (B) elevating the depressed endplate, creating a central cavity, and compacting the remaining trabeculae to the periphery. Once the balloon tamp is deflated and withdrawn, the cavity (C) is filled under low pressure with a viscous preparation of methylmethacrylate (D).
In kyphoplasty, a KyphX inflatable bone tamp is percutaneously advanced into the collapsed vertebral body (A). It is then inflated, (B) elevating the depressed endplate, creating a central cavity, and compacting the remaining trabeculae to the periphery. Once the balloon tamp is deflated and withdrawn, the cavity (C) is filled under low pressure with a viscous preparation of methylmethacrylate (D).
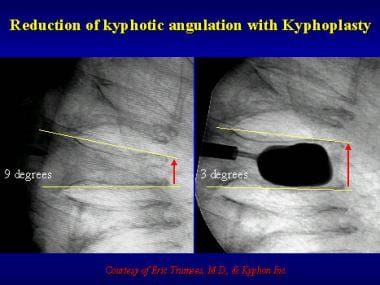
The degree to which the height of the vertebral body and the angulation of depressed endplates are corrected appears to vary from case to case. The maximum volume of the balloon and the pressure required for inflation determine the inflation of the balloons, and therefore, the degree of height restoration. See image below.
Once height is improved, the balloon catheters are deflated and withdrawn. A preparation of methylmethacrylate thicker than that used in vertebroplasty is then injected under relatively low pressure into the cavities created by the inflated balloons. This procedure is used to maintain the elevation of the endplate and stabilize the fracture fragments, thereby reducing or eliminating pain and promoting healing (see images below). Because this acrylic is more viscous that that used for vertebroplasty and because it is injected under lower pressure that in vertebroplasty, the risk of intravascular extension of acrylic is thought to be lower.
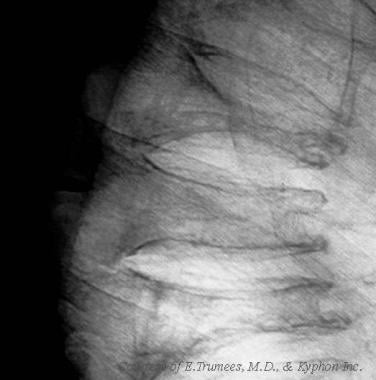 This image was obtained in an 80-year-old man with a steroid-induced osteoporosis and a painful acute midthoracic vertebral compression fracture. Several additional chronic fractures are also present.
This image was obtained in an 80-year-old man with a steroid-induced osteoporosis and a painful acute midthoracic vertebral compression fracture. Several additional chronic fractures are also present.
 After inflation of balloon tamp, the depressed superior endplate is elevated, and some height is restored. The cavity is then filled with methylmethacrylate. Pain is reduced, and the patient's posture is improved.
After inflation of balloon tamp, the depressed superior endplate is elevated, and some height is restored. The cavity is then filled with methylmethacrylate. Pain is reduced, and the patient's posture is improved.
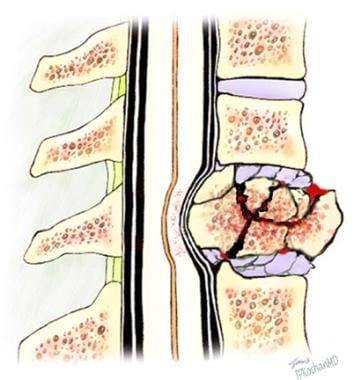
The compact 4d trabeculae at the periphery of the acrylic acts as a bone graft, providing a dense matrix of bone upon which endosteal healing can occur. Kyphoplasty is most effective with acute compression fractures secondary to either trauma or osteoporosis, but it is not recommended for the treatment of fractures secondary to infection, most solid tumors, and vascular lesions. The presence of a burst fracture with loss of integrity of the posterior vertebral cortex and retropulsion of a fracture fragment into the spinal canal is considered exclusionary (see image below). Kyphoplasty is not indicated for the treatment of degenerative disk or joint disease.
As with vertebroplasty, patients must exercise caution in subsequent activities because other osteoporotic vertebral bodies also may be prone to fracture. Medical management of the underlying disorder that weakens the vertebral bodies should be initiated. This procedure does not eliminate the need for aggressive treatment of osteoporosis, without which other fractures may ensue. Ideally, treatment should include risedronate (Actonel), alendronate (Fosamax), calcitonin (Miacalcin), calcium supplements, and multivitamins, including vitamins C and D. Hormonal replacement therapy should also be considered in female patients. Alterations in the medications and dosage of drugs that predispose patients to osteoporosis (eg, steroids) should also be evaluated. Progress should be monitored with serial DEXA scans.
In 1998, the FDA approved the use of this acrylic in kyphoplasty. To the author's knowledge, no investigators from long-term outcome studies have reported the breakdown of the acrylic over time. Preliminary clinical 2-year follow-up data from approximately 4000 kyphoplasties in more than 3000 patients is favorable.
Methylmethacrylate is an FDA-approved medical-grade tissue adhesive that has been used for more than 30 years in the fixation of artificial joint prostheses. Its use in vertebroplasty, however, is not approved by the FDA, which means that it has not been reviewed in the process whereby the government approves the bone cement and technique specifically used for this procedure. In vertebroplasty, the acrylic cement, which the FDA considers a medical device, is used in an off-label application.
Balloon kyphoplasty, a minimally invasive procedure for the treatment of painful vertebral fractures, was compared with nonsurgical care in an international, multicenter, randomized trial by Wardlaw et al. In the study, 300 patients with 1-3 acute vertebral fractures were randomized to kyphoplasty treatment (149 patients) or nonsurgical therapy (151 patients). In the kyphoplasty group, the mean short-form 36 physical component summary (PCS) score improved by 7.2 points (26.0 at baseline to 33.4 at 1 month) as compared to a 2.0 points improvement while the short-form 36 PCS score improved by 2.0 points (from 25.5 to 27.4) in the nonsurgical group (difference between groups 5.2 points, 2.9-7.4; p< 0.0001). The 2 groups did not differ in frequency of adverse events, and the authors concluded, based on the study findings, that balloon kyphoplasty is both safe and effective in patients with acute vertebral fractures and that the procedure may be considered as an early treatment option. [12]
Complications
The risks of the procedure are low, but they potentially include infection, worsening of pain, and neurologic problems such as weakness or pain in the legs.
Occasionally, the acrylic may extend into the epidural or paraspinous veins. Cement in the epidural venous plexus may lead to an ascending venous thrombosis or contribute to a spinal stenosis or cord or nerve root compression. Acrylic may extend from the paraspinous veins into the vena cava and may result in a pulmonary embolus. The risk of venous embolization increases if the operator cannot adequately identify when the cement begins to pass into the venous system. This risk is reduced by using angiographic equipment with the highest resolution available. The visibility of methylmethacrylate is further improved with the addition of fine metallic powders such as barium mixed with tantalum or tungsten.
Controversy has arisen regarding patients previously treated with vertebroplasty. Patients with osteoporosis should be aware that new fractures can occur in vertebra adjacent to previously treated vertebra. This, however, is not the result of the vertebroplasty procedure; rather, it is a consequence of the wedge deformity of the original fracture exerting additional stresses on the adjacent weakened osteoporotic vertebra (see image below). These patients are at risk of a second fracture of an adjacent vertebral body from this deformity, regardless of whether a vertebroplasty procedure was performed on the first fracture.
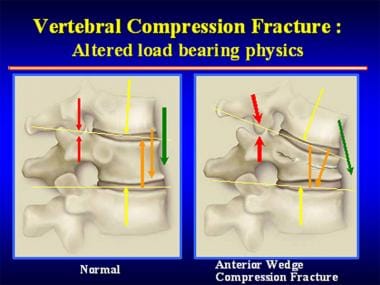 Once an anterior wedge compression fracture has occurred, the physics of load bearing distribution are altered, creating abnormal stress points on the adjacent vertebra that can lead to a second fracture. This, however, is not the result of the vertebroplasty procedure; rather, it is a consequence of the wedge deformity of the original fracture exerting additional stresses on the adjacent weakened osteoporotic vertebra. A second fracture is likely to occur from this deformity, regardless of whether a vertebroplasty procedure is performed on the first fracture. Some authorities believe vertebroplasty stops the progression of a compression fracture, preventing further wedge deformity and likely reducing the chance of a second fracture.
Once an anterior wedge compression fracture has occurred, the physics of load bearing distribution are altered, creating abnormal stress points on the adjacent vertebra that can lead to a second fracture. This, however, is not the result of the vertebroplasty procedure; rather, it is a consequence of the wedge deformity of the original fracture exerting additional stresses on the adjacent weakened osteoporotic vertebra. A second fracture is likely to occur from this deformity, regardless of whether a vertebroplasty procedure is performed on the first fracture. Some authorities believe vertebroplasty stops the progression of a compression fracture, preventing further wedge deformity and likely reducing the chance of a second fracture.
This author believes that vertebroplasty stops the progression of a compression fracture, preventing further wedge deformity; therefore, vertebroplasty probably reduces the likelihood of a second fracture (see image below), although no studies to date have verified this theory.
Results
Approximately 85-90% of patients have rapid pain relief.
This procedure is associated with a low morbidity rate. Less than 1% of patients with nonneoplastic lesions and only 5-8% of patients with neoplastic lesions have morbidity. Morbidity may include local pain, rib pain, spinal stenosis, nerve root compression, and intravascular extension of acrylic.
At the author's institution, pain improved in all patients who have undergone vertebroplasty; approximately 90% of patients note a complete resolution of pain. Incisional and muscular pain may persist for the first few days after the procedure. Point tenderness that is noted before the procedure has not been noted in any of the patients after the procedure. Follow-up assessment is made by telephone. The patient completes a questionnaire before the procedure and 3 weeks and 6 months after the procedure for comparison. Preliminary survey results suggest that patients have a new baseline pain and mobility level at 3 weeks after the procedure, and their use of narcotics for pain control is significantly reduced or eliminated. Anecdotal evidence suggests that vertebroplasty of metastatic spinal lesions may also retard the growth of the tumor and reduce and stabilize pain. [13]
Although pain is reduced or eliminated after the procedure, patients must exercise caution in subsequent activities because other osteoporotic vertebral bodies may also be prone to fracture. Medical management of the underlying disorder that weakens the vertebral bodies should be initiated. This procedure does not eliminate the need for aggressive treatment of osteoporosis, without which other fractures may ensue. Ideally, treatment should include Actonel; Fosamax; Miacalcin; calcium supplements; and multivitamins, including vitamins C and D. Hormonal replacement therapy should also be considered in female patients. Alterations in the medications and dosage of drugs that predispose the patients to osteoporosis (eg, steroids) should also be evaluated. Progress should be monitored with serial dual-energy x-ray absorptiometric (DEXA) scans. For complete medical treatment details, see Medscape Reference article Osteoporosis.
Questions & Answers
Overview
What is percutaneous vertebroplasty and kyphoplasty?
What are the indications for percutaneous vertebroplasty and kyphoplasty?
When is percutaneous vertebroplasty and kyphoplasty contraindicated?
What is the role of anesthesia in the performance of percutaneous vertebroplasty and kyphoplasty?
What are the inclusion and exclusion criteria for percutaneous vertebroplasty and kyphoplasty?
How is percutaneous vertebroplasty performed?
What are the possible complications of percutaneous vertebroplasty and kyphoplasty?
What are the reported outcomes of percutaneous vertebroplasty and kyphoplasty?
-
Anterior wedge compression fracture with intact posterior vertebral cortex.
-
Transpedicular placement of a trocar in the anterior third of the fractured vertebral body.
-
Anterior wedge compression fracture after fusion of the fracture fragments with methylmethacrylate.
-
Lateral radiograph of fractured vertebra shows the initial placement of the trocar.
-
Injection of methylmethacrylate through the trocar in anterior one third of the vertebral body.
-
Compression fracture after vertebroplasty.
-
In a vertebral hemangioma, the fine trabeculae are replaced by venous channels, which predispose the patient to painful microfractures.
-
In a vertebral hemangioma after vertebroplasty, the venous channels are now filled with acrylic.
-
Two adjacent vertebral hemangiomas causing continuous back pain as seen by MRI (A) and CT (B, C, D). Fluoroscopic appearance prevertebroplasty (E, F) and postvertebroplasty (G, H). The patient's pain had abated by the end of the procedure.
-
A vertebral burst fracture is a fracture that cannot be treated safely by using vertebroplasty.
-
Once an anterior wedge compression fracture has occurred, the physics of load bearing distribution are altered, creating abnormal stress points on the adjacent vertebra that can lead to a second fracture. This, however, is not the result of the vertebroplasty procedure; rather, it is a consequence of the wedge deformity of the original fracture exerting additional stresses on the adjacent weakened osteoporotic vertebra. A second fracture is likely to occur from this deformity, regardless of whether a vertebroplasty procedure is performed on the first fracture. Some authorities believe vertebroplasty stops the progression of a compression fracture, preventing further wedge deformity and likely reducing the chance of a second fracture.
-
In kyphoplasty, a KyphX inflatable bone tamp is percutaneously advanced into the collapsed vertebral body (A). It is then inflated, (B) elevating the depressed endplate, creating a central cavity, and compacting the remaining trabeculae to the periphery. Once the balloon tamp is deflated and withdrawn, the cavity (C) is filled under low pressure with a viscous preparation of methylmethacrylate (D).
-
Reduction in kyphotic angulation after kyphoplasty.
-
This image was obtained in an 80-year-old man with a steroid-induced osteoporosis and a painful acute midthoracic vertebral compression fracture. Several additional chronic fractures are also present.
-
After inflation of balloon tamp, the depressed superior endplate is elevated, and some height is restored. The cavity is then filled with methylmethacrylate. Pain is reduced, and the patient's posture is improved.