Practice Essentials
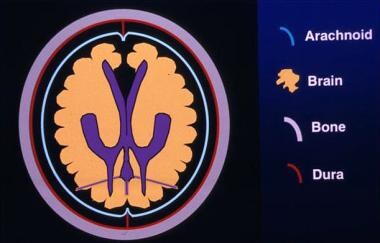
The skull is formed by the fusion of several flat bones held together by the cranial sutures. Each of the flat bones consists of a thick outer table, the spongy diploe, and a thinner inner table. The inner table is lined by a thick, fibrous, adherent dura mater. A shallow subdural space lies between the inner surface of the dura and the thin arachnoid mater that covers the surface of the brain.
A skull fracture is a break in the skull bone and generally occurs as a result of direct impact. The skull is deformed by localized impact, which may damage the cranial contents even when the skull does not fracture. If the force and deformation are excessive, the skull fractures at or near the site of impact. Uncomplicated skull fractures themselves rarely produce neurologic deficit, but the associated intracranial injury may have serious neurologic sequelae. A fracture indicates that substantial force has been applied to the head and is likely to have damaged the cranial contents.
Skull fractures may occur with no associated neurologic damage, and conversely, fatal injury to membranes, blood vessels, and brain may occur without overlying fracture. However, skull fractures may be associated with intracranial hemorrhage, which may create an intracranial space-occupying lesion. In addition, cerebral edema associated with skull fractures is a common and frequently fatal complication of head injury and may develop within minutes or hours of injury. Cerebral edema may accompany diffuse axonal injury or a space-occupying lesion, such as an intracranial hematoma. In children, brain swelling may be the only identifiable feature of head injury. Severe brain edema or a large intracranial hemorrhage may cause downward brain displacement and coning, which is usually fatal. [1, 2]
Anatomy
Skull thickness is not uniform, and therefore, the impact of forces required to cause a fracture depends on the site of the impact. The skull is thick at the glabella, the external occipital protuberance, the mastoid processes, and the external angular process. The skull vault is comparatively thinner than the base of the skull. The skull vault is composed of cancellous bone, the diploe, which is sandwiched between the inner and outer tables and consists of the lamina externa (1.5 mm) and the lamina interna (0.5 mm). The diploe does not form where the skull is covered with muscles, leaving the vault thin and prone to fracture.
Skull fractures are more easily sustained at the thin squamous temporal and parietal bones, [1, 3, 4] the sphenoid sinus, the foramen magnum, the petrous temporal ridge, and the inner parts of the sphenoid wings at the skull base. The middle cranial fossa forms the thinnest part of the skull and thus represents the weakest part, which is further weakened by the presence of multiple foramina. Other sites at risk for fracture are the cribriform plate, the roof of orbits in the anterior cranial fossa, and the areas between the mastoid and dural sinuses in the posterior cranial fossa.
(See the images below.)
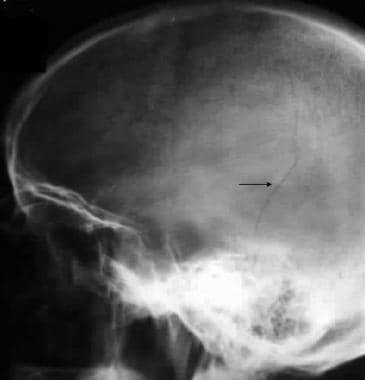
Linear skull fractures
Linear fractures, the most common skull fractures, involve a break in the bone but no displacement, and generally no intervention is required. These fractures are usually the result of low-energy transfer due to blunt trauma over a wide surface area of the skull. The fracture involves the entire thickness of the skull. Generally, these fractures are of little clinical significance unless they involve a vascular channel, a venous sinus groove, or a suture. Thus, complications include epidural hematoma, venous sinus thrombosis, and suture diastasis. (See the following images.)
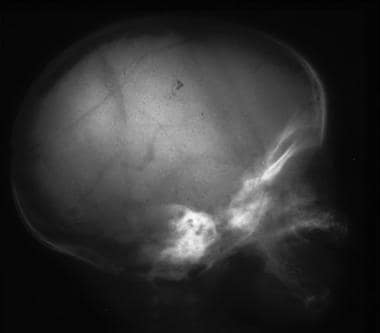
 Lateral skull radiograph in a child shows a long, linear fracture extending from the midline in the occipital region across the occipital bone into the temporal bone. The fracture is more radiolucent than the other sutures, has no serration along its edges, and is blind ending. At the blind end, it is more tapered than it is at the sutural or proximal end. Note the lack of branches.
Lateral skull radiograph in a child shows a long, linear fracture extending from the midline in the occipital region across the occipital bone into the temporal bone. The fracture is more radiolucent than the other sutures, has no serration along its edges, and is blind ending. At the blind end, it is more tapered than it is at the sutural or proximal end. Note the lack of branches.
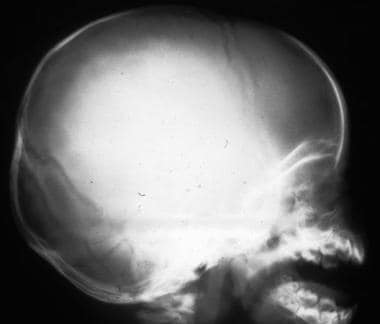
 Lateral skull radiograph in a child shows a long, linear fracture running across the occipital bone. Note its radiolucency and straightness and the lack of branches from it. This is not a vessel and not a known site for a suture.
Lateral skull radiograph in a child shows a long, linear fracture running across the occipital bone. Note its radiolucency and straightness and the lack of branches from it. This is not a vessel and not a known site for a suture.
A high-energy transfer, such as a blow from a baseball bat, may cause a depressed skull fracture, in which bone fragments are driven inward, with or without a breach in the scalp (see the first 2 images below). This fracture is usually comminuted (as exemplified in the third image below), with the bone fragments starting from the point of maximum impact and spreading peripherally. Most depressed fractures involve the frontoparietal region, because the bones in this area are relatively thin and because this part of the head is particularly prone to an assailant's attack.
Depressed skull fractures
A fracture is clinically significant and requires elevation when a fragment of bone is depressed deeper than the adjacent inner table. Depressed fractures may be closed or compound (open). Compound fractures may be exposed when they are associated with a skin laceration or when the fracture extends into the paranasal sinuses and the middle-ear structures. Depressed fractures may require surgery to correct the deformity.
Depressed compound skull fractures account for 42–66% of all fractures in children and for 9% of all fractures in children younger than 1 year. Dural injury can be observed under fractures; approximately 11% of pediatric depressed fractures are accompanied by dural injuries that resulted in intracranial lesions. [5]
 Lateral skull radiograph in a child shows an occipital fracture. It has a sclerotic margin and is therefore likely to be depressed. This is an example of a nonaccidental injury.
Lateral skull radiograph in a child shows an occipital fracture. It has a sclerotic margin and is therefore likely to be depressed. This is an example of a nonaccidental injury.
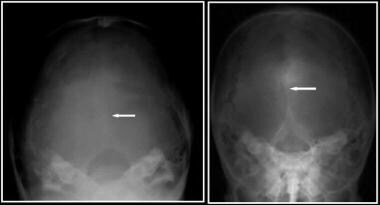 Plain radiographs of the head of a 25–year-old man who was assaulted with a baseball bat show a curvilinear shadow indicating a depressed fracture.
Plain radiographs of the head of a 25–year-old man who was assaulted with a baseball bat show a curvilinear shadow indicating a depressed fracture.
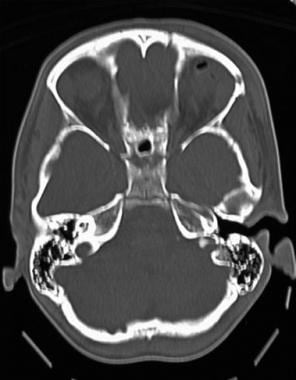
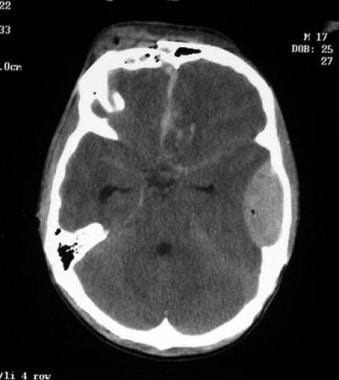 Axial computed tomography scan demonstrates an open comminuted and depressed frontal bone fracture with clotted blood along the interhemispheric fissure. Contusional hemorrhage is present in the left frontal lobe, as is a left-sided temporal extradural hematoma containing a small pocket of air; this finding implies an open fracture. The temporal horns are slightly dilated, suggesting the development of hydrocephalus.
Axial computed tomography scan demonstrates an open comminuted and depressed frontal bone fracture with clotted blood along the interhemispheric fissure. Contusional hemorrhage is present in the left frontal lobe, as is a left-sided temporal extradural hematoma containing a small pocket of air; this finding implies an open fracture. The temporal horns are slightly dilated, suggesting the development of hydrocephalus.
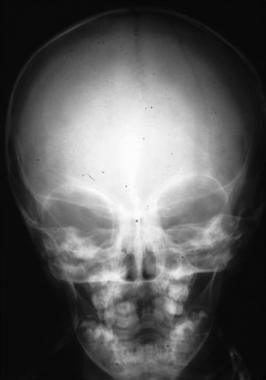
Diastatic skull fractures
Diastatic fractures occur along the suture lines and usually affect newborns and infants in whom suture fusion has not yet occurred. In this type of fracture, the normal suture lines are widened (see the images below).
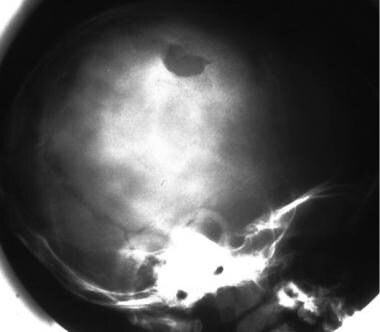
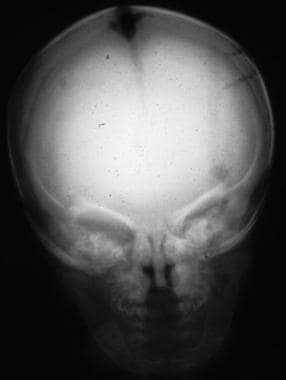 Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma show a diastatic fracture of the sagittal suture.
Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma show a diastatic fracture of the sagittal suture.
 Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma shows a diastatic fracture of the sagittal suture.
Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma shows a diastatic fracture of the sagittal suture.
Basilar skull fractures
Basilar skull fractures (BSFs) are the most serious and involve a linear break in the bone at the base of the skull. Most basilar fractures occur at 2 specific anatomic locations—namely, the temporal region and the occipital condylar region. These fractures are often associated with dural tears, of which cerebrospinal fluid (CSF) rhinorrhea and otorrhea are known complications. Such patients usually require close observation in the hospital.
Temporal fractures are divided into 3 subtypes: longitudinal, transverse, and mixed. [3] The longitudinal fracture is the most common subtype (70-90%) and involves the squamous part of the temporal bone, the superior wall of the external auditory canal, and the tegmen tympani. The fracture may run either anterior or posterior to the cochlea and labyrinthine capsule, ending in the middle cranial fossa near the foramen spinosum or in the mastoid air cells. Transverse fractures (5-30%) originate at the foramen magnum and extend through the cochlea and labyrinth, ending in the middle cranial fossa. As the name suggests, mixed fractures have components of both longitudinal and transverse fractures.
A retrospective review found a BSF prevalence of 26% in a group of 180 pediatric patients with severe traumatic brain injury (TBI). The temporal bone was fractured in two thirds of the patients with BSFs, and CSF leaks were observed in one third of these patients. In this series, BSFs were indicative of a significant linear blunt force and were independent predictors of mortality. [6]
Occipital condylar fractures are generally the result of high-energy transfer from blunt trauma with axial compression, lateral bending, or rotational injury to the alar ligament. These fractures can be subdivided into 3 types based on the morphology and mechanism of injury [7] or, alternatively, into stable and displaced fractures depending on the presence or absence of ligamentous injury. [8] A type I fracture is due to axial compression injury, which results in a comminuted fracture of the occipital condyle. This fracture is stable. A type II fracture is caused by a direct blow, and although it is an extensive fracture of the basioccipital region, it is regarded as a stable injury because of the preserved alar ligament and tectorial membrane. A type III fracture is potentially unstable and regarded as an avulsion injury due to forced rotation and lateral bending.
Ping-pong skull fractures
The ping-pong skull fracture (see the image below) is akin to a greenstick fracture of the long bones in children. It occurs in the first few months of life and is usually caused by a fall when the skull hits the edge of a hard blunt object, such as a table. The skull appears deformed, with a shallow trench on the surface of the skull. The ping-pong skull fracture was first described in a newborn whose head was impinging against the mother's sacral promontory during uterine contractions. The use of forceps also may cause this injury to the skull, but this mechanism is rare.
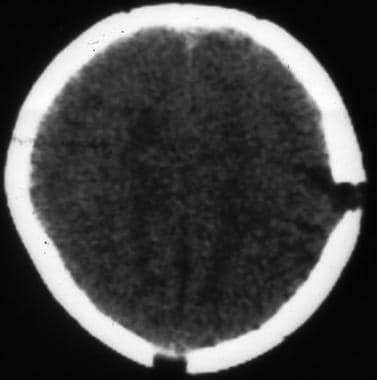
 Lateral computed tomography (CT) scanogram and axial bone-window CT scan demonstrate a temporal fracture. The CT scan shows slight inward bulging of the bone, but the inner and outer tables are intact. This is a classic ping-pong ball fracture roughly akin to a greenstick fracture in a long bone. This fracture only occurs in children because the skull vault is more elastic and less rigid than it is in adults.
Lateral computed tomography (CT) scanogram and axial bone-window CT scan demonstrate a temporal fracture. The CT scan shows slight inward bulging of the bone, but the inner and outer tables are intact. This is a classic ping-pong ball fracture roughly akin to a greenstick fracture in a long bone. This fracture only occurs in children because the skull vault is more elastic and less rigid than it is in adults.
Birth fractures
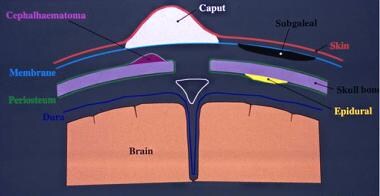
Caput succedaneum commonly occurs after vaginal delivery and is related to a serosanguineous effusion, which appears as a soft-tissue swelling over the presenting part of the skull. Caput succedaneum is a benign process that generally resolves within 2 weeks and usually does not require any form of imaging. However, a cephalohematoma may develop after an instrumental delivery and represents a subperiosteal hematoma.
In contrast to a caput succedaneum, a cephalohematoma is limited by suture lines. In addition, a cephalohematoma may be visible on a plain radiograph as a subperiosteal elevation. Birth skull fractures may occur as a complication of forceps or vacuum extraction. (A forceps injury is shown below.) Most are simple parietal linear fractures, but occasionally, they are more complex or depressed. In some cases, associated extradural hematoma, [9] subdural hematoma, or axonal injury is observed.
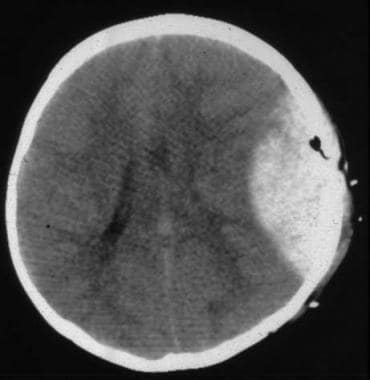
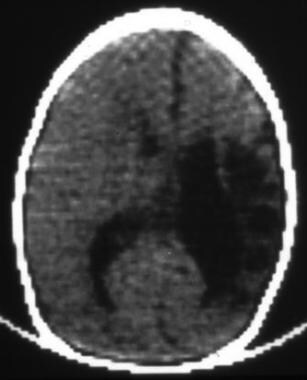 Computed tomography scan of an 8-week-old baby after forceps delivery shows a major insult to the left cerebral hemisphere, which is now atrophic. This scan shows hypoattenuating areas in the brain parenchyma, with dilatation of the ipsilateral lateral ventricle and a midline shift toward the atrophic side.
Computed tomography scan of an 8-week-old baby after forceps delivery shows a major insult to the left cerebral hemisphere, which is now atrophic. This scan shows hypoattenuating areas in the brain parenchyma, with dilatation of the ipsilateral lateral ventricle and a midline shift toward the atrophic side.
Growing skull fractures
In children, most skull fractures heal rapidly, with no long-term sequelae. However, in a small minority of children, a fracture may remain un-united and enlarge to form a growing skull fracture. Most growing skull fractures (GSFs) are located in the calvarium, but rare sites are the basiocciput and the orbital roof.
Most cases occur after falls, motor vehicle accidents, and child abuse. Cases related to difficult vacuum extraction and corrective surgery for craniosynostosis have also been described. In 1816, John Hopkins described an infant with GSF after a head injury. Since then, cases of GSF (see the images below) continue to appear in the literature, with various names such as a leptomeningeal cyst, traumatic meningocele, cerebrocranial erosion, cephalhydrocele, meningocele, and spuria.
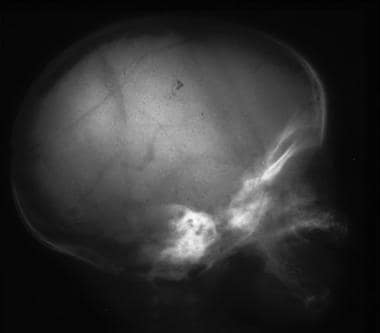
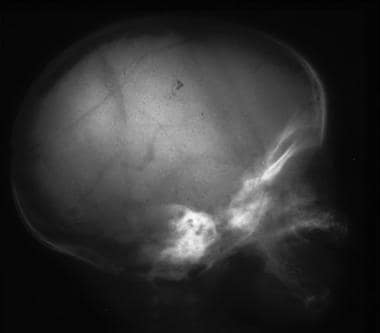
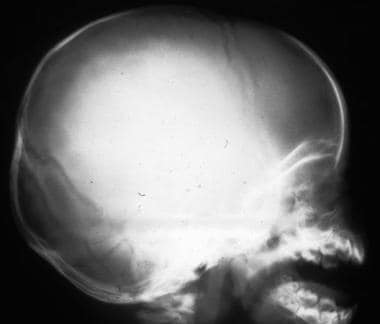
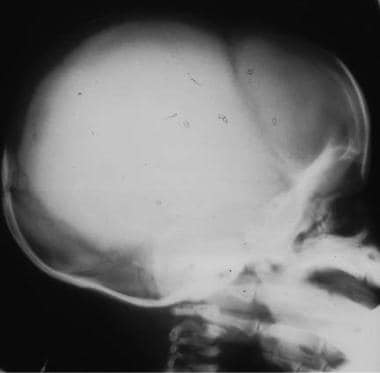
 Lateral skull radiograph in a child with a growing fracture. The mechanism of injury is usually a direct force applied to the cranial vault, resulting in the fracture, with tearing of the dura so that cerebrospinal fluid (CSF) leaks to form a collection. Because the CSF is under pressure and pulsatile, a transmitted pulsation from the subarachnoid space into the extra-axial fluid collection causes pressure enlargement of the fracture.
Lateral skull radiograph in a child with a growing fracture. The mechanism of injury is usually a direct force applied to the cranial vault, resulting in the fracture, with tearing of the dura so that cerebrospinal fluid (CSF) leaks to form a collection. Because the CSF is under pressure and pulsatile, a transmitted pulsation from the subarachnoid space into the extra-axial fluid collection causes pressure enlargement of the fracture.
 Lateral skull radiograph in a child with a growing fracture. The mechanism of injury is usually a direct force applied to the cranial vault, resulting in the fracture, with tearing of the dura so that cerebrospinal fluid (CSF) leaks to form a collection. Because the CSF is under pressure and pulsatile, a transmitted pulsation from the subarachnoid space into the extra-axial fluid collection causes pressure enlargement of the fracture.
Lateral skull radiograph in a child with a growing fracture. The mechanism of injury is usually a direct force applied to the cranial vault, resulting in the fracture, with tearing of the dura so that cerebrospinal fluid (CSF) leaks to form a collection. Because the CSF is under pressure and pulsatile, a transmitted pulsation from the subarachnoid space into the extra-axial fluid collection causes pressure enlargement of the fracture.
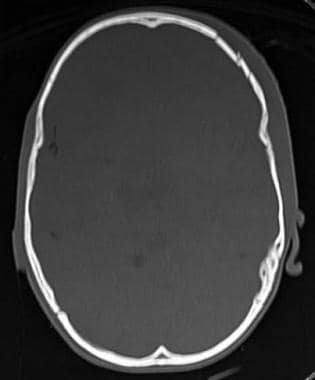
 Axial computed tomography scan shows a growing skull fracture nicely, depicting the widened fracture on the left and the fluid collection extending from the intracranial cavity into and through the fracture site.
Axial computed tomography scan shows a growing skull fracture nicely, depicting the widened fracture on the left and the fluid collection extending from the intracranial cavity into and through the fracture site.
The diagnosis is based on clinical and imaging findings; early recognition of growing skull fractures is crucial to prevent long-term neurologic sequelae. Hence, radiologic and clinical follow-up is essential in cases of head trauma.
Serial conventional radiographs of the skull show evolution of the initial diastatic fracture into a larger defect. Although plain radiographs are sufficient for diagnosis, brain CT scanning better defines the exact pathology. On CT scans, 3 types of growing skull fractures are described: types I, II, and III. Type I is a GSF with a leptomeningeal cyst, which may be seen herniating through the skull defect into the subgaleal space. Type II is characterized by a damaged lesion or gliotic brain. In type III, a porencephalic cyst can be seen.
Magnetic resonance imaging (MRI) is preferred over CT scanning for depicting dural tears early after the head injury and allows timely surgical intervention and prevention of growth of the fracture. Cranial Doppler ultrasonographic studies have also been used to achieve an early diagnosis.
A growing skull fracture poses a challenge to the pediatric neurosurgeon. Matsuura et al presented a case history of a 2-month-old baby boy who fell from his mother's arms and hit his head on the floor; he underwent radiography, MRI, and CT scanning before cranioplasty with dural plasty. Radiography at admission showed a diastatic fracture with a gap of 8 mm in the right frontal bone and a linear fracture in the right occipital bone. The diastatic fracture had increased to 25 mm on radiography performed 37 days after injury. Cranioplasty with dural plasty was performed on day 39. A combination of MRI and CT images enabled the edge of the dural tear to be plotted on a 3-dimensional image of the skull, which was used to estimate the location of the edge of the dural tear on the scalp. Excellent outcomes in terms of bony coverage and dural plasty were achieved. The authors recommended a combination of MRI and CT scanning for surgical repair of growing skull fracture in children. [10]
Scalp injuries
The scalp is made up of several tissue layers: hairy skin; subcutaneous fat and connective tissue; the galea, which is a thin fibrous layer to which the flat epicranial muscles are attached; a thin layer of connective tissue; and the innermost layer, the periosteum of the bony skull.
The scalp may be injured with or without a breach in its surface. Lacerations are particularly common, as the scalp is readily crushed and split against the underlying bone. Most scalp lacerations are linear because of the convexity of the skull. When injured, the scalp often becomes markedly edematous, and hematoma formation is common above or below the galeal layer.
Axonal injury
Minor jarring of the intracranial contents may cause concussion and a clinical state of transient loss of consciousness due to temporary neuronal dysfunction. Retrograde amnesia is common. With more severe injury, a cerebral contusion may occur; this is classified into 2 types: coup and contrecoup.
Coup-type contusion or laceration of the brain surface often occurs at the site of a fracture, especially if it is depressed. A blow to the head when it is free to move accelerates the head and causes cerebral contusion at the point of impact. At the primary point of impact, a bruise, abrasion, or laceration of the scalp is often present.
Contrecoup-type brain contusions occur when the head strikes a stationary object (eg, when the falling head strikes the ground). The head decelerates abruptly while the intracranial contents continue moving forward to the point of impact. The result is a severe contusion in a region opposite the point of impact. This contrecoup contusion is more severe than the coup contusion. A severe contrecoup force may also cause a laceration on the brain surface. Therefore, a backward fall causes contrecoup contusions at the frontal and temporal poles of the brain, whereas a fall on the side of the head causes contrecoup contusions at the opposite temporal lobe. Generally, a forward fall does not cause contrecoup contusions on the back of the brain because the interior surface of the skull is smooth at this point.
Missile wounds
Missiles can be subdivided into (1) low-velocity bullets, such as those used in air rifles, nail guns, stun guns (used for animal slaughter), handguns, shotguns, and shrapnel, and (2) high-velocity bullets, such as metal-jacket bullets fired from military weapons. Low-velocity and high-velocity bullet wounds are shown in the images below.
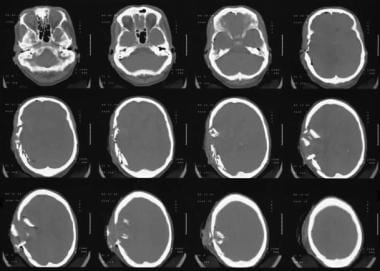
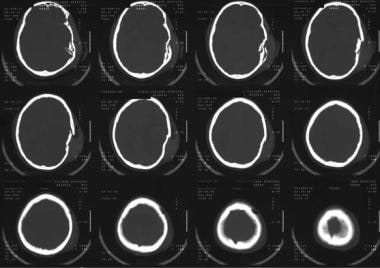
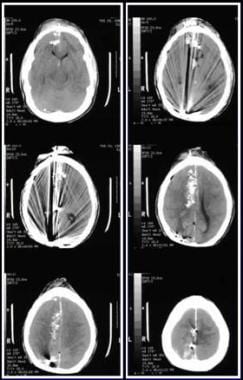 Axial computed tomography scans show penetrating injury from a low-velocity bullet. The entry site is the frontal bone; note the intracranial metallic bone attenuations, intracranial air, cerebral edema, and subarachnoid hemorrhage.
Axial computed tomography scans show penetrating injury from a low-velocity bullet. The entry site is the frontal bone; note the intracranial metallic bone attenuations, intracranial air, cerebral edema, and subarachnoid hemorrhage.
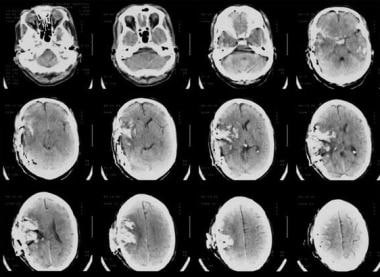
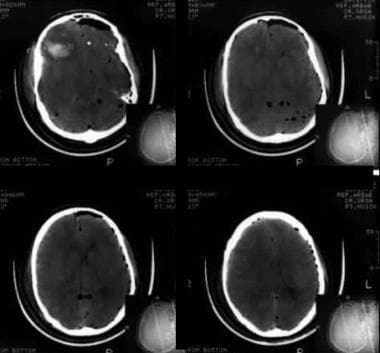 Computed tomography scans of the head show air in the cranium, intracerebral hematoma, and cerebral edema due to a high-velocity gunshot wound. The presence of the reversal sign suggests severe brain swelling and probably secondary hypoxic ischemic injury to the brain as a result of the pressure on the brain.
Computed tomography scans of the head show air in the cranium, intracerebral hematoma, and cerebral edema due to a high-velocity gunshot wound. The presence of the reversal sign suggests severe brain swelling and probably secondary hypoxic ischemic injury to the brain as a result of the pressure on the brain.
Missiles produce brain injury by causing laceration and crushing, cavitation, and shock waves. The injuries to the skull range from a graze to an entry wound and sometimes an exit hole (penetrating) or a depressed fracture, with results ranging from focal hemorrhage to extensive neuronal damage. Differentiating between penetrating and perforating skull wounds is important because of their different prognostic implications. A poor postsurgical outcome occurs in 50% of patients treated for perforating wounds, as compared with 20% of those with penetrating wounds. Additional examples of missile wounds are shown below.
 A missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
A missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
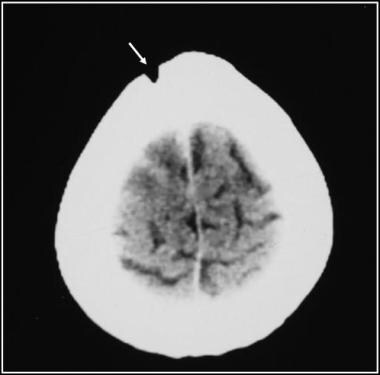
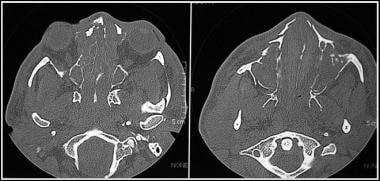
 Computed tomography scan of a missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
Computed tomography scan of a missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
 Computed tomography scan of a missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
Computed tomography scan of a missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
Stab wounds
Penetrating skull stab wounds are uncommon. Stab wounds are caused by knives, nails, spikes, forks, scissors, and other sharp objects. Skull penetration most commonly occurs in the thinnest parts of the skull, such as the orbital surfaces and the squamous portion of the temporal bone. Injury to the brain usually occurs in the path of the penetrating stab wound. Unlike missile injuries, stab wounds have no concentric zone of coagulative necrosis caused by dissipated energy, and unlike motor vehicle accidents, stab wounds cause no diffuse, shearing brain injury.
Stab wounds may cause an intracranial hematoma or infarct. Cerebral damage caused by stabbing is largely restricted to the wound tract. Stab wounds occasionally produce a narrow, elongated defect (a slot fracture); this injury is diagnostic when identified. However, in some cases in which skull penetration is proven, no radiologic abnormality is identified. A stab wound to the temporal fossa is most likely to cause major neurologic injury because of the thinness of the squamous temporal bone and because of the short distance to the brainstem and blood vessels.
The type of skull fracture sustained and the underlying brain injury depend on the variation in skull thickness and on the strength and angle of the impact. A stab wound nearly perpendicular to the skull may cause bone fragments to travel along the same trajectory as that of the penetrating object, it may shatter the skull in an irregular pattern, or it may produce linear fractures that radiate away from the entry site. Tangential stab wounds result in complex single defects, with both internal and external beveling of the skull and varying degrees of neurologic injury.
Nonaccidental trauma
Most fractures in children are a result of falls and bicycle accidents, but skull fractures in infants may originate from neglect, falls, or abuse. Nonaccidental injury or shaken baby syndrome is a major cause of skull fractures and head injury in infants. The classic syndrome is an infant with a mean age of about 6 months who has retinal hemorrhages, subdural hematomas, and absent or minimal signs of external trauma. Because the parents seldom volunteer a history of nonaccidental injury or shaken baby syndrome, this condition is difficult to document and diagnose. Examples of nonaccidental trauma are shown below.
 Lateral skull radiograph in a child shows an occipital fracture. It has a sclerotic margin and is therefore likely to be depressed. This is an example of a nonaccidental injury.
Lateral skull radiograph in a child shows an occipital fracture. It has a sclerotic margin and is therefore likely to be depressed. This is an example of a nonaccidental injury.
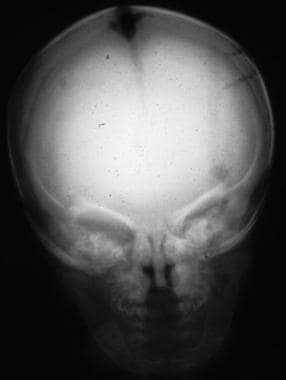 Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma show a diastatic fracture of the sagittal suture.
Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma show a diastatic fracture of the sagittal suture.
 Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma shows a diastatic fracture of the sagittal suture.
Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma shows a diastatic fracture of the sagittal suture.
About 25% of all patients with shaken baby syndrome die. Usually, the child is grasped around the chest by using 2 hands and repeatedly shaken with its head moving forward and backward, causing rotational acceleration/deceleration injury. Injuries most often observed in inflicted head trauma are subgaleal hematomas, skull fractures, subarachnoid hemorrhages (SAHs), subdural hematomas, and parenchymal brain injuries.
In an infant, anything but a nonwidely spaced simple linear fracture of the parietal bone should be viewed with suspicion and regarded as a nonaccidental injury until proven otherwise. Such fractures include depressed, stellate, comminuted, or other complex skull fractures. Some researchers believe that falls from a distance less than 3 feet rarely produce any kind of skull fracture and that skull fractures occur only with extremely violent forces. However, Plunkett demonstrated that simple and complex skull fractures can occur with short falls. [11]
Greenes and Schutzman showed that skull fractures may be asymptomatic and yet be associated with underlying dural or brain injury. [12] Young infants (< 6 mo) may have major cranial deformation due to an impact but no skull fracture because their skulls are malleable and elastic, whereas older children have more rigid adultlike ossified skulls and are more vulnerable to skull fractures.
Margulies and Thibault have shown that the fracture threshold for an infant is approximately 10% that of a child or adult. [13] A special pattern of bilateral skull fractures can occur when crushing forces are applied against the infant skull. Skull fractures cannot occur without impact of the head against a rigid object. They cannot occur with shaking.
Hobbs demonstrated that fracture characteristics found considerably more often in abused children were a multiple or complex configuration; depressed, wide, and growing skull fractures; involvement of more than one cranial bone; nonparietal fracture; and associated intracranial injury, including subdural hematoma. [14] Multiple injuries and an inadequate history assisted in diagnosing abuse. No fractures >5 mm on presentation were found after accidents, but 6 growing skull fractures were found in abused children. However, accidents usually resulted in single, narrow, linear fractures, most commonly in the parietal bone, with no associated intracranial injury. [14] The results suggest that in young children with skull fracture in whom a minor fall is alleged, it is possible to recognize abuse by considering the fracture alone.
Extradural hemorrhage
The temporal bone is usually the thinnest part of the skull. A fracture at this site may tear the middle meningeal artery as it passes upward within a groove between the inner skull table and the dura. A blow to the temporal bone may result in a tear of the temporal artery without a fracture (15%). An arterial bleed from a middle meningeal artery accumulates, forming a hematoma between the inner skull table and stripped dura; this is called an extradural hemorrhage, which acts as a space-occupying lesion. This accumulation can be immediate or delayed.
Subdural hemorrhage
Subdural hemorrhages are more common than epidural hemorrhages, and they are especially common in the elderly, children, and individuals with alcoholism. Subdural hemorrhages are not usually associated with skull fractures but may occur after sudden jarring or rotation of the head, a blow to the head, or a fall. Trauma to the head may be trivial. Movement of the brain relative to the dura, often associated with widened CSF spaces, causes shears and tears of the small veins that bridge the gap between the dura and the cortical surface of the brain. Blood from torn vessels accumulates over several hours and usually tracks extensively as a thin film over the surface of the brain. A small, self-limiting subdural hemorrhage may remain asymptomatic and be an incidental finding.
Subarachnoid hemorrhage
Subarachnoid hemorrhages may occur as a result of a ruptured intracranial arterial aneurysm or trauma. Traumatic subarachnoid hemorrhage is usually associated with brain contusion or laceration. In rare cases, this type of hemorrhage is due to a direct blow to the side of the neck, which ruptures the vertebral artery as it enters the cranial cavity. This phenomenon is called traumatic basal subarachnoid hemorrhage and is most often due to a blow to the side of the chin or jaw in an alcohol-induced fistfight. The degree of traumatic force required to cause a basal subarachnoid is less than reasonably expected.
Intracerebral hemorrhage
Intracerebral hemorrhage may occur as a result of a ruptured atheromatous intracerebral arteriole, vasculitis, ruptured intracranial arterial aneurysm, or trauma. Traumatic intracerebral hemorrhage is usually due to extension of hemorrhage from surface contusions deep into the substance of the brain. Traumatic intracerebral hemorrhage may also be the result of rupture of small blood vessels deep within the brain due to shearing stress.
Preferred Examination
Imaging plays a vital role in the diagnosis and characterization of head injuries. Skull radiography is useful for imaging of calvarial fractures, penetrating injuries, and radiopaque foreign bodies.
CT scanning is an essential imaging modality in detecting intracranial lesions that require urgent surgical intervention, such as an acute subdural hematoma. Skull fractures are detected on plain radiographs in 5% of patients with mild head injuries, but the detection of a skull fracture on a radiograph is regarded as an indication for CT evaluation. Therefore, obtaining a radiograph can only delay the diagnosis of an associated intracranial injury. Because cervical spine trauma may accompany a head injury, radiographs of the cervical spine are indicated for many patients with head injury who have signs, symptoms, or a mechanism of injury that might result in spinal injury, as well as for those patients who are neurologically impaired. [15]
Masters et al developed and prospectively tested a management strategy for the selection of patients who may benefit from skull radiography after head trauma; the effect of this study was to shift the focus of imaging of head injury away from skull radiography and toward the recognition of intracranial pathology, as demonstrated by CT scanning. [16] They offered recommendations for selection of patients who should receive CT scanning following head injury.
CT scanning is increasingly being used to identify minimal and minor head injury in patients who may benefit from observation; clinical criteria have not proven to be consistently reliable for the identification of those with significant intracranial injury. MRI depicts nonsurgical pathology not visible on CT. In the assessment of complications, CT may be appropriate; however, MRI is useful in identifying vestibular hemorrhage and delayed complications of head injury.
In a study of preoperative CT scans in 141 patients with calvarial skull fractures, the number of fractured calvarial bones was found to be an independent predictor of outcome in traumatic brain injury patients after early craniotomy. [17]
Ultrasonography is a noninvasive technique that may be useful for evaluating growing skull fractures and associated intracranial hemorrhage in infants. In adults, the orbit can also be assessed for soft-tissue injury by using sonograms.
Cerebral angiography may be indicated if a vascular injury is suspected and if the patient is stable, though CT angiography (CTA) or magnetic resonance angiography (MRA) can be used to obtain similar information. CTA can be used for the evaluation of both intracranial and extracranial vessels. The American College of Radiology (ACR) has issued Appropriateness Criteria for imaging in cases of head injury (see Table 1). [18]
Table 1. Head Trauma--Adult. ACR Appropriateness Criteria Scales* [18] (Open Table in a new window)
Criterion |
Skull X-ray |
CT without IV contrast |
CT with IV contrast |
MRI |
MRA |
Comments |
Minor or mild acute closed head injury (GCS ≥13), imaging not indicated by NOC or CCHR or NEXUS-II clinical criteria |
1 |
2 |
1 |
1 |
1 |
|
Minor or mild acute closed head injury (GCS ≥13), imaging indicated by NOC or CCHR or NEXUS-II clinical criteria |
1 |
9 |
1 |
5 |
2 |
MRI may be appropriate in the outpatient setting, but panel members disagreed on the appropriateness rating. |
Moderate or severe acute closed head injury (GCS < 13) |
1 |
9 |
1 |
2 |
1 |
|
Short-term follow-up imaging of acute traumatic brain injury. No neurologic deterioration |
1 |
5 | 1 | 2 | 2 | CT without IV contrast can be used in patients with risk factors |
Short-term follow-up imaging of acute traumatic brain injury. Neurologic deterioration, delayed recovery, or persistent unexplained deficits |
1 |
9 |
5 |
8 |
5 |
MRI is complementary if CT does not explain clinical symptoms. CT with IV contrast and MRA may be appropriate in patients with suspected post-traumatic infarction |
Subacute or chronic traumatic brain injury with new cognitive and/or neurologic deficit(s) |
1 |
7 |
2 |
9 |
3 |
|
Suspected intracranial arterial injury |
1 | 9 | 1 | 9 | 9 | Either CTA or MRA can be performed, depending on institutional preference; MRI is is complementary, in conjunction with MRA; CT is complementary, in conjunction with CTA |
* Scales are designated 1-9, where 1, 2 3 = usually not appropriate; 4,5,6 = may be appropriate; and 7,8, 9 = usually appropriate. NOC = New Orleans Criteria, CCHR = Canadian CT Head Rules, NEXUS-II = National Emergency X-Ray Utilization Study Clinical Criteria. |
||||||
Approximately 3-5% of children with minor head trauma have identifiable abnormalities by imaging, and typically less than 1% require neurosurgical intervention. [19] In fact, routine CT scanning for all patients with skull fractures may be unnecessary, because few patients with minor head injury develop a life-threatening intracranial hematoma that must be rapidly detected and surgically treated.
Noncontrast CT has a central role in screening for intracranial traumatic injury due to its wide availability, speed, and ability to detect significant hemorrhage, herniation, hydrocephalus, and fractures. Small hemorrhages may be missed by CT, although the sensitivity can be improved with multiplanar reformations. Three-dimensional (3-D) reconstructed images can also be particularly helpful in young patients to help distinguish fractures from normal or variant sutures. The most significant disadvantage of CT is the necessary exposure to ionizing radiation. This is of particular concern in pediatric patients because of the increased radiosensitivity of young tissues, longer lifespan, and overall greater risk of subsequent iatrogenic malignancy. The absolute incidence of induced lethal malignancy has not been definitively proven, but the estimated risk in children is 1/1000 to 1/5000 per cranial CT. [19]
Isotopic bone scans may be useful in children with suspected nonaccidental injury, as the scans may show fractures elsewhere in the body in various stages of healing. CSF rhinorrhea and otorrhea can be detected and localized by using overpressure cisternography with technetium-99m (99mTc) diethylenetriaminepentaacetic acid (DTPA). The ACR suggests that 99mTc whole body bone scans be used as a problem solving study rather than first-line assessment. The ACR Appropriateness Criteria for imaging in cases of head injury and suspected physical abuse in children is summarized in Table 2 below. [19, 20]
Table 2. Head Trauma. ACR Appropriateness Criteria Scales* [19, 20] (Open Table in a new window)
Criterion |
Skull X-ray |
CT without IV contrast |
CT with IV contrast |
MRI |
MRA |
Comments |
Minor head injury (GCS >13) ≥2 years of age without neurologic signs or high risk factors (eg, altered mental status, clinical evidence of basilar skull fracture). Excluding nonaccidental trauma. |
1 |
3 |
1 |
2 |
1 |
|
Minor head injury (GCS >13), < 2 years of age, no neurologic signs or high-risk factors. Excluding nonaccidental trauma. |
3 |
3 |
2 |
3 |
2 |
CT has shown to be low yield in the absence of signs or symptoms. It may be considered if clinical assessment is uncertain or indeterminate. |
Moderate or severe head injury (GCS ≤13) or minor head trauma with high-risk factors. Excluding nonaccidental trauma. |
2 |
9 |
2 |
7 |
4 |
Consider MRA if vascular injury is suspected. |
| Subacute head injury with cognitive and/or neurologic signs | 1 | 7 | 2 | 8 | 3 | Consider MRA if vascular injury is suspected |
| Suspected nonaccidental head trauma | 7 | 9 | 2 | 8 | 3 | Consider MRA if vascular injury is suspected |
Suspected physical abuse. Child ≤24 months of age. Neurological or visceral injuries not clinically suspected |
9 | 5 | 1 | 6 | N/A | |
| Suspected physical abuse. Child >24 months of age. Neurological or visceral injuries not clinically suspected | 9 | 6 | 1 | 5 | N/A | |
| Child with one or more of the following: neurologic signs or symptoms, apnea, complex skull fracture, other fractures, or injuries highly suspicious for child abuse. | 9 | 9 | 1 | 8 | N/A | CT is used in the emergent setting. MRI is typically performed in a nonemergent setting; consider MRI of cervical spine at the time of MRI brain imaging. |
* Scales are designated 1-9, where 1, 2 3 = usually not appropriate, 4,5,6 = may be appropriate and 7,8, 9 = usually appropriate. N/A = not applicable |
||||||
Single-photon emission CT (SPECT) scanning, positron emission tomography (PET) scanning, and transcranial Doppler ultrasonography have complementary roles in the assessment of brain injury.
Limitations of Techniques
Conventional radiographs do not help in assessing intracranial complications associated with skull fractures. In addition, temporal bone fractures may be easily missed.
Temporal bone CT scanning requires additional imaging time and patient cooperation, neither of which may be possible in the immediate posttraumatic period. CT scanning cannot be used to distinguish between CSF and hemorrhage in the middle ear. CT scanning does involve exposure to x-ray radiation, but the benefit of an accurate diagnosis far outweighs the risk. The effective radiation dose from this procedure is about 2 millisievert (mSv), which is about the same as that which the average person receives from background radiation in 8 months. This dose is equal to the radiation dose of 100 posteroanterior (PA) chest radiographs.
MRI has limited availability in the acute trauma setting, long imaging times, sensitivity to patient motion, incompatibility with various medical and life-support devices, and relative insensitivity to subarachnoid hemorrhage. Other disadvantages include the need for MRI-specific monitoring equipment and ventilators and the risk associated with imaging patients with certain indwelling devices or foreign bodies. Some of these limitations can be overcome by placing the MRI unit close to emergency care areas, with appropriate design and equipment for the management of acutely injured patients. The development of wide-bore magnets, fast imaging protocols, and MRI-compatible resuscitation equipment promises a greater role for MRI in the evaluation of closed head injuries.
Cisternography with 99mTc DTPA may not be immediately available, as this study is expensive and cumbersome. Cerebral angiography is an invasive procedure and generally performed only in patients in stable condition.
Other Problems to Be Considered
Sutures may be confused with fractures. Sutures are winding, serpiginous lines; less than 2 mm in width, with same width throughout; and don't run in a straight line. Well-corticated sclerotic margins are symmetrical, with standard anatomic locations. (See the images below.)
 Lateral skull radiograph shows the importance of having the patient positioned straight for lateral imaging. Because the patient is slightly malpositioned, both coronal sutures are seen as separate entities. This problem also applies to the lambdoid sutures; because they are separated, one could be mistaken for a fracture. Accessory occipital sutures are also exaggerated by the patient's rotation.
Lateral skull radiograph shows the importance of having the patient positioned straight for lateral imaging. Because the patient is slightly malpositioned, both coronal sutures are seen as separate entities. This problem also applies to the lambdoid sutures; because they are separated, one could be mistaken for a fracture. Accessory occipital sutures are also exaggerated by the patient's rotation.
 Anteroposterior (AP) skull radiograph in a child shows the sagittal and lambdoid sutures and a prominent squamous cell suture on the right side. None of these are fractured, and all have serrated edges. The sutures communicate one with another; they are not blind ending. The child is probably younger than 1 year.
Anteroposterior (AP) skull radiograph in a child shows the sagittal and lambdoid sutures and a prominent squamous cell suture on the right side. None of these are fractured, and all have serrated edges. The sutures communicate one with another; they are not blind ending. The child is probably younger than 1 year.
 Lateral skull radiograph shows the normal bilateral squamous temporal sutures, not to be confused with fractures.
Lateral skull radiograph shows the normal bilateral squamous temporal sutures, not to be confused with fractures.
 Frontal skull radiograph of a child shows the usual coronal and sagittal sutures. On the left is an accessory suture, which is seen to extend from the squamous central suture to the lambdoid suture. Although fractures and sutures can be difficult to differentiate, the accessory suture can be identified as such because it connects 2 sutures, has an even caliber and radiopacity throughout, and has slightly serrated edges. In general, when a fracture connects 2 sutures, the fracture line is wide open or open mouthed at the sutural connection and is narrowest away from the suture. In this case, the fracture line is of even caliber all the way across.
Frontal skull radiograph of a child shows the usual coronal and sagittal sutures. On the left is an accessory suture, which is seen to extend from the squamous central suture to the lambdoid suture. Although fractures and sutures can be difficult to differentiate, the accessory suture can be identified as such because it connects 2 sutures, has an even caliber and radiopacity throughout, and has slightly serrated edges. In general, when a fracture connects 2 sutures, the fracture line is wide open or open mouthed at the sutural connection and is narrowest away from the suture. In this case, the fracture line is of even caliber all the way across.
 Frontal skull radiograph shows a persistent metopic suture that has not yet fused; this is not a fracture.
Frontal skull radiograph shows a persistent metopic suture that has not yet fused; this is not a fracture.
Vascular markings may also be difficult to differentiate from fractures. These markings engrave the inner table of the skull only, are less translucent than fractures, have ill-defined margins, and have symmetrical branching patterns. In addition, meningeal grooves taper as they run peripherally, and diploic venous markings are wide (see the following image).
 Frontal skull radiograph demonstrates a left-sided fracture. The fracture is radiolucent and wide, and it courses without interruption across the occipital and parietal bones. The other side shows a vascular marking of similar radiolucency, but it is of even caliber and its origin in the occipital region is from another vessel.
Frontal skull radiograph demonstrates a left-sided fracture. The fracture is radiolucent and wide, and it courses without interruption across the occipital and parietal bones. The other side shows a vascular marking of similar radiolucency, but it is of even caliber and its origin in the occipital region is from another vessel.
 Lateral skull radiograph demonstrates a left-sided fracture. The fracture is radiolucent and wide, and it courses without interruption across the occipital and parietal bones. The other side shows a vascular marking of similar radiolucency, but it is of even caliber and its origin in the occipital region is from another vessel.
Lateral skull radiograph demonstrates a left-sided fracture. The fracture is radiolucent and wide, and it courses without interruption across the occipital and parietal bones. The other side shows a vascular marking of similar radiolucency, but it is of even caliber and its origin in the occipital region is from another vessel.
Special Concerns
Failure to recognize skull fracture has more consequences than the complications resulting from treatment. About 15% of patients with skull fractures sustain concomitant injury to the cervical spine; therefore, missing such a fracture has both clinical and medicolegal implications.
In infants and children, a simple linear fracture may be associated with a dural tear, which can lead to subepicranial hygroma or a growing skull fracture. This complication may take up to 6 months to develop, and hence, close radiologic follow-up is important in these patients. In addition, a fracture line crossing a vascular groove may be associated with an epidural hematoma; therefore, recognition of this possibility is important, as the hematoma may need surgical drainage. Similarly, a fracture line that crosses over a suture may cause sutural diastasis and a growing fracture.
A complete and sudden onset of facial palsy at the time of fracture is usually secondary to nerve transection, and patients in this condition have a poor prognosis. Moreover, a sphenoid bone fracture may affect cranial nerves III, IV, and VI, and it also may disrupt the internal carotid artery. In rare cases, pseudoaneurysm formation and caroticocavernous fistulas occur as complications. Therefore, efforts should be made to recognize these complications early.
The risk of epilepsy after a depressed fracture is low, but the risk increases when patients lose consciousness for longer than 2 hours and when they have associated dural tears. Dural tears can be recognized on imaging, and therefore, it is important to make this distinction from both the therapeutic and prognostic point of view. In addition, basilar skull fractures with CSF leak pose a risk of meningitis if the CSF leak is chronic and not repaired.
Controversy exists regarding the need to elevate a depressed fracture and whether the choice to elevate a skull fracture is the surgeon's. From an imaging point of view, it is important to assess the degree of depression. Obtaining 3-D CT scan reconstructions may help in decision making.
Skull fractures pose a significant potential risk of underlying direct injury to the brain, CNs, and vessels. However, most skull fractures are linear vault fractures, particularly in children, and are not associated with epidural hematoma. Some skull fractures are associated with serious neurologic complications, and hence, the medicolegal implications of missing a primary fracture during the diagnostic workup can be serious as well.
Patients treated surgically for contaminated open depressed skull fractures should be monitored with repeat CT studies to check for abscess formation. Follow-up CT evaluation is also recommended when complications, such as seizures and infections, occur in association with skull fractures.
Preoperative angiography with a venous-phase image or MRA is indicated when depressed fractures overlie the dural venous sinuses. A retrospective review of 472 patients with blunt skull trauma concluded that an increased suspicion for dural venous sinus thrombosis (DVST) is warranted in patients with skull fractures with a low Glasgow Coma Scale score and recent fall from a height greater than 10 ft. [21]
Radiography
In most patients with suspected head injury, radiographs of the lateral cervical spine and chest are obtained in the resuscitation room.
In general, conventional radiography of the skull has a limited role, if any, to play in the management of skull fractures with or without blunt head injury. Skull fractures are detected on plain radiographs in 5% of patients with mild head injuries, but the detection of a skull fracture on a conventional radiograph is regarded as an indication to proceed to CT scanning. Therefore, obtaining a radiograph only delays the diagnosis of associated intracranial injury.
Skull radiography still has a role to play in evaluating nonaccidental trauma in both adults [18] and children (demonstrated in the images below), when it is usually performed as a part of a skeletal survey. [2, 19, 20]
 Lateral skull radiograph in a child shows an occipital fracture. It has a sclerotic margin and is therefore likely to be depressed. This is an example of a nonaccidental injury.
Lateral skull radiograph in a child shows an occipital fracture. It has a sclerotic margin and is therefore likely to be depressed. This is an example of a nonaccidental injury.
The following are postmortem radiographs of skull fractures in a child with nonaccidental trauma.
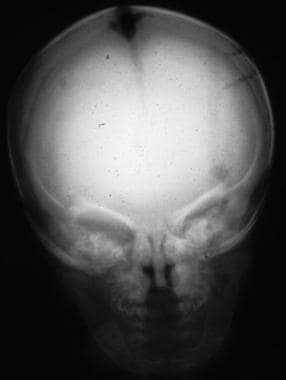 Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma show a diastatic fracture of the sagittal suture.
Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma show a diastatic fracture of the sagittal suture.
 Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma shows a diastatic fracture of the sagittal suture.
Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma shows a diastatic fracture of the sagittal suture.
Conventional radiographic appearances of skull fractures include the following:
-
Straight, translucent lines with sharp margins
-
Width >3 mm, widest at the center and narrow at the ends
-
Course through both the outer and the inner lamina of bone
-
Involvement of both tables of the skull
-
Straight in most fractures, possibly with a sudden change in direction
-
Fracture margins that are usually parallel and that generally do not taper
-
With growing skull fractures, a fracture line that crosses a coronal or a lambdoid suture, usually limited to a parietal bone
Radiographs are suboptimal in detecting basilar skull fractures. However, although fractures at the skull vertex may be missed on CT scans, they may be depicted on plain radiographs. In general, skull radiographs are of no benefit when CT scanning is performed. In the developing world, with limited access to CT scanners, plain radiography of the skull is regarded as useful in screening head injuries. The detection of skull fractures allows for admission of the patient to the hospital for observation.
Skull radiographs reveal most linear fractures, show air-fluid levels in the paranasal sinuses and cranium, and delineate the craniocervical junction well. Because most adult patients have a calcified pineal gland, a skull radiograph may reveal a midline shift due to a mass effect, and patients are treated in light of the plain radiographic results, especially when there is no access to CT scanning. When no cross-sectional imaging is available, fractures of the skull base can be diagnosed on clinical grounds aided by associated radiologic signs of pneumocephaly; on conventional radiographs, an air-fluid level may be seen in the frontal or sphenoid sinuses.
False positives/negatives
A false-positive diagnosis may be made when unusual vascular markings and suture lines (as seen below) are found on radiographs. Many skull-base fractures may be missed on conventional radiography.
 Lateral skull radiograph shows the importance of having the patient positioned straight for lateral imaging. Because the patient is slightly malpositioned, both coronal sutures are seen as separate entities. This problem also applies to the lambdoid sutures; because they are separated, one could be mistaken for a fracture. Accessory occipital sutures are also exaggerated by the patient's rotation.
Lateral skull radiograph shows the importance of having the patient positioned straight for lateral imaging. Because the patient is slightly malpositioned, both coronal sutures are seen as separate entities. This problem also applies to the lambdoid sutures; because they are separated, one could be mistaken for a fracture. Accessory occipital sutures are also exaggerated by the patient's rotation.
 Anteroposterior (AP) skull radiograph in a child shows the sagittal and lambdoid sutures and a prominent squamous cell suture on the right side. None of these are fractured, and all have serrated edges. The sutures communicate one with another; they are not blind ending. The child is probably younger than 1 year.
Anteroposterior (AP) skull radiograph in a child shows the sagittal and lambdoid sutures and a prominent squamous cell suture on the right side. None of these are fractured, and all have serrated edges. The sutures communicate one with another; they are not blind ending. The child is probably younger than 1 year.
 Lateral skull radiograph shows the normal bilateral squamous temporal sutures, not to be confused with fractures.
Lateral skull radiograph shows the normal bilateral squamous temporal sutures, not to be confused with fractures.
 Frontal skull radiograph of a child shows the usual coronal and sagittal sutures. On the left is an accessory suture, which is seen to extend from the squamous central suture to the lambdoid suture. Although fractures and sutures can be difficult to differentiate, the accessory suture can be identified as such because it connects 2 sutures, has an even caliber and radiopacity throughout, and has slightly serrated edges. In general, when a fracture connects 2 sutures, the fracture line is wide open or open mouthed at the sutural connection and is narrowest away from the suture. In this case, the fracture line is of even caliber all the way across.
Frontal skull radiograph of a child shows the usual coronal and sagittal sutures. On the left is an accessory suture, which is seen to extend from the squamous central suture to the lambdoid suture. Although fractures and sutures can be difficult to differentiate, the accessory suture can be identified as such because it connects 2 sutures, has an even caliber and radiopacity throughout, and has slightly serrated edges. In general, when a fracture connects 2 sutures, the fracture line is wide open or open mouthed at the sutural connection and is narrowest away from the suture. In this case, the fracture line is of even caliber all the way across.
 Frontal skull radiograph shows a persistent metopic suture that has not yet fused; this is not a fracture.
Frontal skull radiograph shows a persistent metopic suture that has not yet fused; this is not a fracture.
 Frontal skull radiograph demonstrates a left-sided fracture. The fracture is radiolucent and wide, and it courses without interruption across the occipital and parietal bones. The other side shows a vascular marking of similar radiolucency, but it is of even caliber and its origin in the occipital region is from another vessel.
Frontal skull radiograph demonstrates a left-sided fracture. The fracture is radiolucent and wide, and it courses without interruption across the occipital and parietal bones. The other side shows a vascular marking of similar radiolucency, but it is of even caliber and its origin in the occipital region is from another vessel.
 Lateral skull radiograph demonstrates a left-sided fracture. The fracture is radiolucent and wide, and it courses without interruption across the occipital and parietal bones. The other side shows a vascular marking of similar radiolucency, but it is of even caliber and its origin in the occipital region is from another vessel.
Lateral skull radiograph demonstrates a left-sided fracture. The fracture is radiolucent and wide, and it courses without interruption across the occipital and parietal bones. The other side shows a vascular marking of similar radiolucency, but it is of even caliber and its origin in the occipital region is from another vessel.
 Skull radiograph in a premature baby. The skull vault develops in membrane, whereas the skull base develops in cartilage. When ossification of the skull vault is impaired or premature, the frontal, temporal, and parietal bones form reasonably well but do not meet in the midline. As a result, the outer table of the skull is often not visible on a lateral skull radiograph. Moreover, the sutures appear to be widened, but only because the bone margins have not come together and because of increased intracranial pressure.
Skull radiograph in a premature baby. The skull vault develops in membrane, whereas the skull base develops in cartilage. When ossification of the skull vault is impaired or premature, the frontal, temporal, and parietal bones form reasonably well but do not meet in the midline. As a result, the outer table of the skull is often not visible on a lateral skull radiograph. Moreover, the sutures appear to be widened, but only because the bone margins have not come together and because of increased intracranial pressure.
Computed Tomography
CT scanning is the modality of choice in the evaluation of suspected skull fractures and intracranial injury. Once the patient's cardiopulmonary condition has been stabilized, a CT scan of the head should be obtained to determine the extent of intracranial damage and whether there are intracranial metallic fragments in penetrating injuries. Thin-section bone windows of up to 1-1.5 mm, with sagittal reconstruction, are useful in assessing injuries. [22, 23]
Technique
Helical and/or multisection CT scanning is helpful in assessing occipital condylar fractures, but 3-D reconstruction is usually not necessary. However, 3-D reconstructions are valuable when evaluating facial fractures. (Such reconstructions are exhibited in the images below, along with follow-up MRI scans.) The study should always include bone windows to evaluate for fractures, especially when the skull base or orbits are compromised.
 Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
 Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
 Computed tomography scans in a child with a high-impact injury to the frontoethmoid region show a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scans of the maxillofacial skeleton nicely show the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
Computed tomography scans in a child with a high-impact injury to the frontoethmoid region show a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scans of the maxillofacial skeleton nicely show the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
 Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
 Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
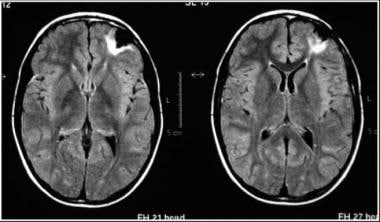 Axial fluid-attenuated inversion recovery (FLAIR) magnetic resonance images obtained at 2-year follow-up of a child who had a high-impact injury to the frontoethmoid region demonstrate focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
Axial fluid-attenuated inversion recovery (FLAIR) magnetic resonance images obtained at 2-year follow-up of a child who had a high-impact injury to the frontoethmoid region demonstrate focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
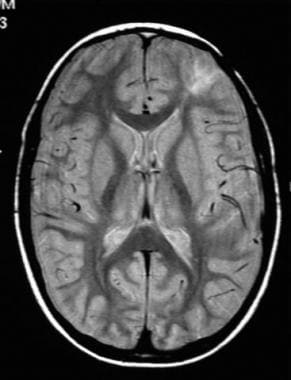 Axial proton density–weighted magnetic resonance image obtained at 2-year follow-up of a child who had a high-impact injury to the frontoethmoid region demonstrate focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
Axial proton density–weighted magnetic resonance image obtained at 2-year follow-up of a child who had a high-impact injury to the frontoethmoid region demonstrate focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
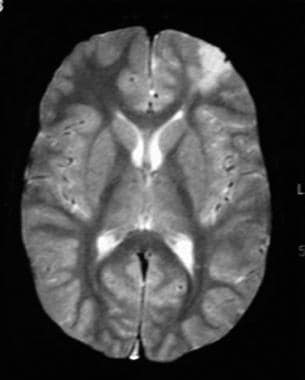 Axial T2-weighted axial MRI obtained at 2-year follow-up demonstrates focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
Axial T2-weighted axial MRI obtained at 2-year follow-up demonstrates focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
CT images with wide windows (1000-4000 Hounsfield units [HU]) are needed to evaluate skull injuries. (Examples of bone-window CT scans are seen in the images below.) CT scanning is as effective as conventional radiographs in depicting linear, comminuted, and depressed skull fractures. The degree of skull depression is easily measured on CT scans. In addition, skull sutures can be readily distinguished from fractures by their symmetry and corticated margins.
However, a linear or minimally depressed fracture may be easily overlooked on CT scans, particularly when viewed with narrow windows. Often, a small streak artifact caused by a misaligned fracture may be a clue. Basilar skull fractures may also remain elusive, as with conventional radiographs. The CT scan appearance that suggests a basilar fracture includes a traumatic pneumocephalus, which indicates a communication between the intracranial space and a paranasal sinus. Sometimes, an air-fluid level is seen in the sphenoid sinus.
 Axial brain and bone-window computed tomography scans show multiple fractures involving the right temporal and parietal bones, with depression of several bone fragments into the brain around which contusional hemorrhage is present. Also present are soft-tissue swelling, air in the cranial cavity related to the bone fragments, and air in the subarachnoid space.
Axial brain and bone-window computed tomography scans show multiple fractures involving the right temporal and parietal bones, with depression of several bone fragments into the brain around which contusional hemorrhage is present. Also present are soft-tissue swelling, air in the cranial cavity related to the bone fragments, and air in the subarachnoid space.
 Axial brain and bone-window computed tomography scans show multiple fractures involving the right temporal and parietal bones, with depression of several bone fragments into the brain around which contusional hemorrhage is present. Also present are soft-tissue swelling, air in the cranial cavity related to the bone fragments, and air in the subarachnoid space.
Axial brain and bone-window computed tomography scans show multiple fractures involving the right temporal and parietal bones, with depression of several bone fragments into the brain around which contusional hemorrhage is present. Also present are soft-tissue swelling, air in the cranial cavity related to the bone fragments, and air in the subarachnoid space.
 Axial brain and bone-window computed tomography scans show an extensive comminuted and markedly depressed open fracture in the left temporoparietal region. Note the soft-tissue swelling associated with air in the soft tissues and intracranial region. The fracture extends into the petrous bone. Contusion of the underlying brain is noted.
Axial brain and bone-window computed tomography scans show an extensive comminuted and markedly depressed open fracture in the left temporoparietal region. Note the soft-tissue swelling associated with air in the soft tissues and intracranial region. The fracture extends into the petrous bone. Contusion of the underlying brain is noted.
 Axial brain and bone-window computed tomography scans show an extensive comminuted and markedly depressed open fracture in the left temporoparietal region. Note the soft-tissue swelling associated with air in the soft tissues and intracranial region. The fracture extends into the petrous bone. Contusion of the underlying brain is noted.
Axial brain and bone-window computed tomography scans show an extensive comminuted and markedly depressed open fracture in the left temporoparietal region. Note the soft-tissue swelling associated with air in the soft tissues and intracranial region. The fracture extends into the petrous bone. Contusion of the underlying brain is noted.
 Bone-window computed tomography scan shows a fracture of the frontal bone. Note the fluid level in the frontal sinus, which suggests that clotted blood is layering out.
Bone-window computed tomography scan shows a fracture of the frontal bone. Note the fluid level in the frontal sinus, which suggests that clotted blood is layering out.
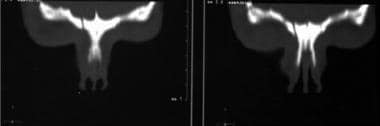
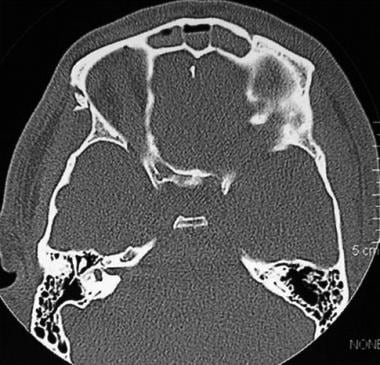
 Bone-window axial computed tomography scans of the maxillofacial skeleton and orbits demonstrate extensive fractures of the entire maxillofacial complex, including the medial walls of the orbits, the medial walls of the antra, and the posteroinferior walls of the antra (in fact all the bones). The pterygoid plates are intact, and the midface is not displaced or dislocated.
Bone-window axial computed tomography scans of the maxillofacial skeleton and orbits demonstrate extensive fractures of the entire maxillofacial complex, including the medial walls of the orbits, the medial walls of the antra, and the posteroinferior walls of the antra (in fact all the bones). The pterygoid plates are intact, and the midface is not displaced or dislocated.
 Lateral computed tomography (CT) scanogram and axial bone-window CT scan demonstrate a temporal fracture. The CT scan shows slight inward bulging of the bone, but the inner and outer tables are intact. This is a classic ping-pong ball fracture roughly akin to a greenstick fracture in a long bone. This fracture only occurs in children because the skull vault is more elastic and less rigid than it is in adults.
Lateral computed tomography (CT) scanogram and axial bone-window CT scan demonstrate a temporal fracture. The CT scan shows slight inward bulging of the bone, but the inner and outer tables are intact. This is a classic ping-pong ball fracture roughly akin to a greenstick fracture in a long bone. This fracture only occurs in children because the skull vault is more elastic and less rigid than it is in adults.
Nonenhanced CT studies show features of intracranial hematomas, which are hyperattenuating in the acute phase. An acute subdural hematoma appears as a crescentic hyperattenuating mass adjacent to the inner skull table, with smooth, well-demarcated borders. Most subdural hematomas are located over the frontal or parietal convexity (as shown below). A subdural hematoma may have a mass effect.
In the acute setting, the attenuation of a subdural hematoma is 40-90 HU. The attenuation values are related to the hemoglobin content and clot. As the acute subdural clot ages, the hemoglobin is degraded and the attenuation values decrease. A subdural hematoma may become isoattenuating, usually within 1-3 weeks. With lysis of the solid elements of the hematoma, attenuation values continue to decrease. In 4-6 weeks, most subdural hematomas have decreased attenuation of around 15-30 HU. The shape in chronic hematomas remains crescentic and well defined.
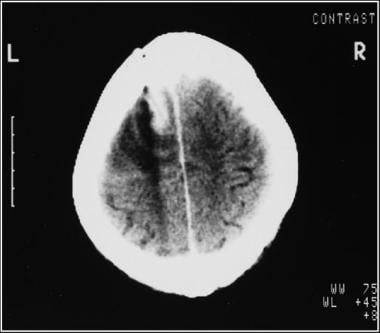
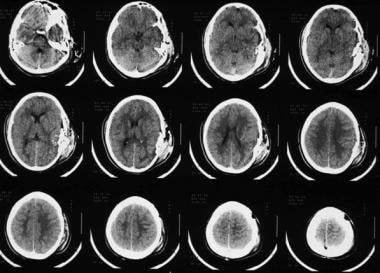
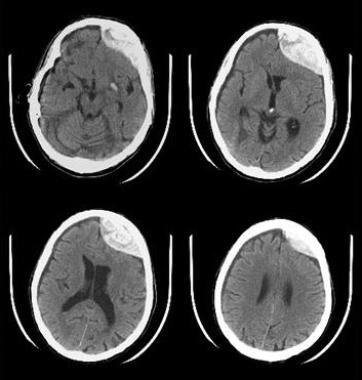 Axial nonenhanced brain computed tomography scans show a left frontal subdural hematoma, which is not totally homogeneous probably because unclotted blood is mixed with it; this implies active hemorrhage.
Axial nonenhanced brain computed tomography scans show a left frontal subdural hematoma, which is not totally homogeneous probably because unclotted blood is mixed with it; this implies active hemorrhage.
Findings
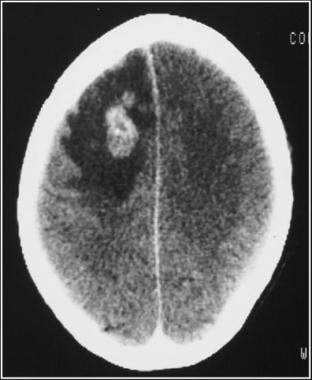
Epidural (extradural) hematomas (shown in the images below) are usually associated with skull fractures that lacerate a meningeal artery, causing blood under arterial pressure to dissect the dura from the inner table of the skull. The skull fracture is demonstrated on imaging in 85% of patients. Epidural hematomas tend to accumulate rapidly, and they are medical emergencies. The characteristic appearance of an epidural hematoma on a CT scan is that of a hyperattenuating, focal, biconvex, smoothly marginated lesion adjacent to the inner table of the skull. These hematomas generally have a mass effect on the intracranial contents. Like subdural hematomas, epidural hematomas may become chronic if the bleeding stops spontaneously. They still appear as biconvex lesions, but their attenuation values are reduced.
 Axial nonenhanced computed tomography scan of the brain shows an open comminuted fracture of the left parietal bone with an underlying extradural hematoma. Air is tracked from the scalp tissues through the fracture into the hematoma.
Axial nonenhanced computed tomography scan of the brain shows an open comminuted fracture of the left parietal bone with an underlying extradural hematoma. Air is tracked from the scalp tissues through the fracture into the hematoma.
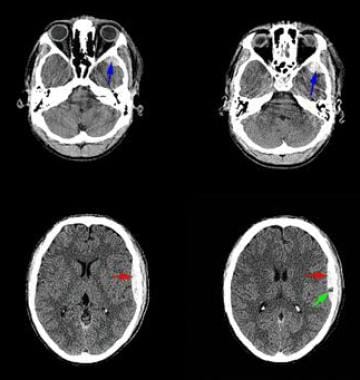 Axial nonenhanced computed tomography scans shows an extradural hematoma anterior to the left temporal lobe (blue arrows). Red arrows point to an extradural hematoma over the upper part of the left temporal lobe. The hematoma in this region is not totally homogeneous, probably because unclotted blood is mixed with it; this implies active hemorrhage. The green arrow points to a small bubble of air in the hematoma, which suggests an open compound fracture. Despite the extradural hematoma, gray matter is clearly distinguishable from white matter, and the ventricles are of normal size. These findings suggest no serious elevation of intracranial pressure at this early stage.
Axial nonenhanced computed tomography scans shows an extradural hematoma anterior to the left temporal lobe (blue arrows). Red arrows point to an extradural hematoma over the upper part of the left temporal lobe. The hematoma in this region is not totally homogeneous, probably because unclotted blood is mixed with it; this implies active hemorrhage. The green arrow points to a small bubble of air in the hematoma, which suggests an open compound fracture. Despite the extradural hematoma, gray matter is clearly distinguishable from white matter, and the ventricles are of normal size. These findings suggest no serious elevation of intracranial pressure at this early stage.
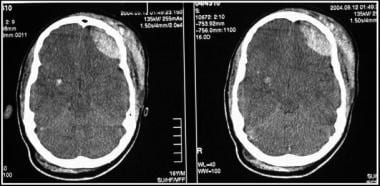 Computed tomography scans show the effect of a direct impact to the left frontal region that resulted in an extracranial hematoma and an intracranial extradural hematoma. Contrecoup hemorrhages are seen in the right temporal region.
Computed tomography scans show the effect of a direct impact to the left frontal region that resulted in an extracranial hematoma and an intracranial extradural hematoma. Contrecoup hemorrhages are seen in the right temporal region.
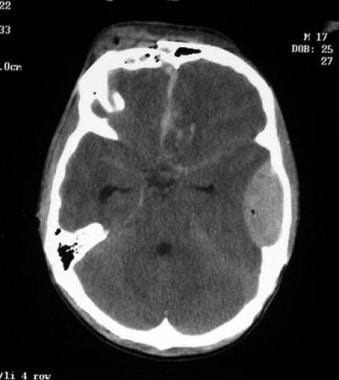 Axial computed tomography scan demonstrates an open comminuted and depressed frontal bone fracture with clotted blood along the interhemispheric fissure. Contusional hemorrhage is present in the left frontal lobe, as is a left-sided temporal extradural hematoma containing a small pocket of air; this finding implies an open fracture. The temporal horns are slightly dilated, suggesting the development of hydrocephalus.
Axial computed tomography scan demonstrates an open comminuted and depressed frontal bone fracture with clotted blood along the interhemispheric fissure. Contusional hemorrhage is present in the left frontal lobe, as is a left-sided temporal extradural hematoma containing a small pocket of air; this finding implies an open fracture. The temporal horns are slightly dilated, suggesting the development of hydrocephalus.
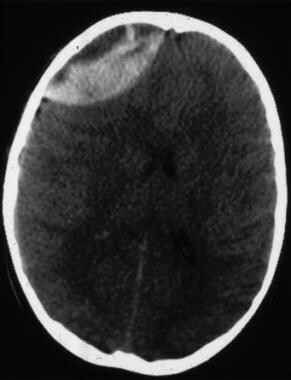 Axial nonenhanced brain computed tomography scan shows a right frontal extradural hematoma. Note that the deep aspect of the hematoma is homogeneously white (high attenuation), whereas the peripheral or outer part is more isoattenuating relative to the brain. The reason for this lack of homogeneity is the presence of clotted blood (white) and unclotted blood (dark) within the hematoma. Three reasons are possible: The most common reason is that the patient is actively bleeding when the hematoma occurred and that the blood has not yet clotted. The second is that the patient was taking anticoagulants, which delayed the clotting time. The third possibility is consumption coagulopathy, in which all the patient's clotting factors are used up in other sites of trauma.
Axial nonenhanced brain computed tomography scan shows a right frontal extradural hematoma. Note that the deep aspect of the hematoma is homogeneously white (high attenuation), whereas the peripheral or outer part is more isoattenuating relative to the brain. The reason for this lack of homogeneity is the presence of clotted blood (white) and unclotted blood (dark) within the hematoma. Three reasons are possible: The most common reason is that the patient is actively bleeding when the hematoma occurred and that the blood has not yet clotted. The second is that the patient was taking anticoagulants, which delayed the clotting time. The third possibility is consumption coagulopathy, in which all the patient's clotting factors are used up in other sites of trauma.
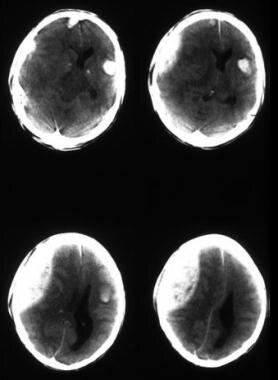 Axial nonenhanced computed tomography scans of the brain demonstrate a right-sided extradural hematoma, which is not homogeneous in its attenuation; this finding suggests the presence of unclotted blood. The images show considerable mass effect on the underlying brain, with subfalcine herniation of the brain to the right side, with a contrecoup left temporal hematoma, and hemorrhage around the anterior aspect of the falx.
Axial nonenhanced computed tomography scans of the brain demonstrate a right-sided extradural hematoma, which is not homogeneous in its attenuation; this finding suggests the presence of unclotted blood. The images show considerable mass effect on the underlying brain, with subfalcine herniation of the brain to the right side, with a contrecoup left temporal hematoma, and hemorrhage around the anterior aspect of the falx.
Most skull fractures and intracranial injuries are associated with extracranial trauma. CT scans reliably depict extracalvarial soft-tissue injuries, such as subgaleal hematomas, elevated and avulsed soft tissues, and scalp edema. Air within the scalp tissue suggests a scalp laceration, but if air, gas, or both are detected several days after trauma, infection should be considered.
Subarachnoid, intraventricular, and intracerebral hematomas are well depicted on nonenhanced CT scans. Subarachnoid hemorrhage after head injury is most frequently the result of tearing of leptomeningeal vessels at the vertex, where the greatest brain movement occurs at impact; less commonly, it is due to a tear of a major intracerebral vessel. An acute subarachnoid hemorrhage is depicted as high attenuation replacing the CSF in the interhemispheric or sylvian fissure, cerebral sulci, or basal cisterns. With extensive subarachnoid hemorrhage, the brainstem, infundibulum, or branches of the carotid artery are bathed by blood, and they may appear as filling defects. (See the image below.)
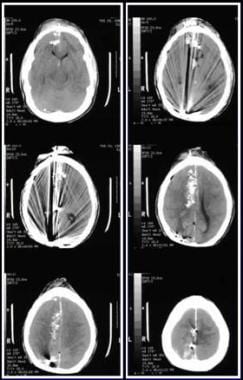 Axial computed tomography scans show penetrating injury from a low-velocity bullet. The entry site is the frontal bone; note the intracranial metallic bone attenuations, intracranial air, cerebral edema, and subarachnoid hemorrhage.
Axial computed tomography scans show penetrating injury from a low-velocity bullet. The entry site is the frontal bone; note the intracranial metallic bone attenuations, intracranial air, cerebral edema, and subarachnoid hemorrhage.
Intracerebral hematoma after trauma is usually the result of shearing of small intracerebral vessels from coup or contrecoup forces (see the following images). Intracerebral hematomas appear as focal areas of increased attenuation, usually surrounded by low attenuation due to edema or contusion. Posttraumatic hematomas are usually irregular and may have a mass effect. Over time, the intracerebral hematomas may become isoattenuating and then hypoattenuating.
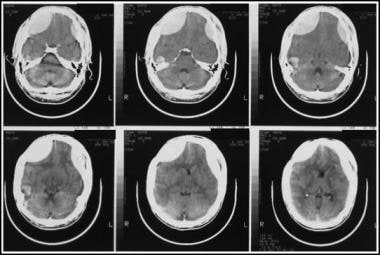 Axial brain computed tomography scans show bilateral contusion and intracerebral hematoma in the frontal extradural and right temporal regions, with features of increased intracranial pressure. The hematoma is adjacent to the attachment of the tentorium to the skull vault; this is a site commonly associated with contrecoup hematomas, because the brain moves but the dura cannot.
Axial brain computed tomography scans show bilateral contusion and intracerebral hematoma in the frontal extradural and right temporal regions, with features of increased intracranial pressure. The hematoma is adjacent to the attachment of the tentorium to the skull vault; this is a site commonly associated with contrecoup hematomas, because the brain moves but the dura cannot.
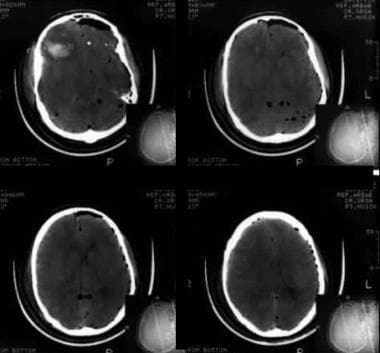 Computed tomography scans of the head show air in the cranium, intracerebral hematoma, and cerebral edema due to a high-velocity gunshot wound. The presence of the reversal sign suggests severe brain swelling and probably secondary hypoxic ischemic injury to the brain as a result of the pressure on the brain.
Computed tomography scans of the head show air in the cranium, intracerebral hematoma, and cerebral edema due to a high-velocity gunshot wound. The presence of the reversal sign suggests severe brain swelling and probably secondary hypoxic ischemic injury to the brain as a result of the pressure on the brain.
Intraventricular hemorrhage has been reported in 5% of patients after head injury. Most cases are associated with extracranial or intracerebral hemorrhage. On CT scans, intraventricular blood is identified as hyperintense tissue in the ventricles. Unclotted blood may layer in the most dependent part of the ventricles.
Intracranial penetrating injuries due to bullets or other sharp objects are characterized by focal areas of increased attenuation representing parenchymal, intraventricular, subarachnoid, or extracerebral hemorrhage. The path of the missile through the brain is often obvious from the location of hemorrhage and metallic fragments. Intracranial metallic fragments from penetrating objects produce streak artifacts that degrade the images. (See the images below.)
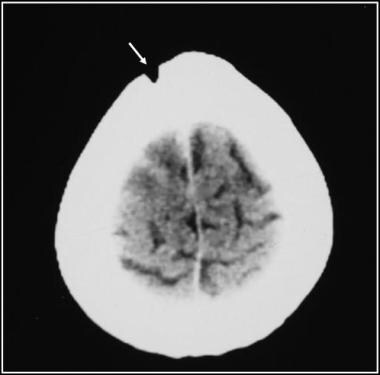 A missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
A missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
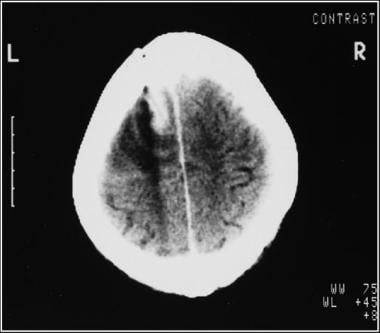 Computed tomography scan of a missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
Computed tomography scan of a missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
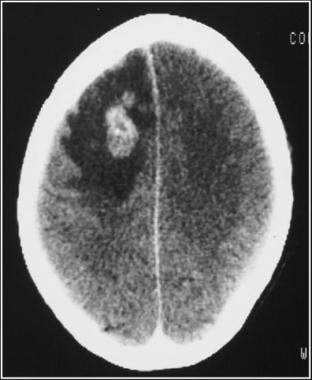 Computed tomography scan of a missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
Computed tomography scan of a missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
Brain edema appears as enlargement of the gyri, obliterating the intervening sulci and compressing the ventricles.
On CT scans, cerebral contusions appear as small, ill-defined foci of increased attenuation surrounded by a large zone of a low-attenuation mass. The central high attenuation represents hemorrhage, and the surrounding low-attenuation mass represents edema and tissue necrosis. Cerebral contusions may cause a mass effect, resulting in ventricular compression, midline shift, and sulcal effacement.
Growing skull fractures may be depicted as hypoattenuating lesions near the fracture site. An intracranial hypoattenuating area may be an encephalomalacia, arachnoid loculation, or cortical atrophy. Below are radiographs and a CT scan of a growing skull fracture.
 Lateral skull radiograph in a child with a growing fracture. The mechanism of injury is usually a direct force applied to the cranial vault, resulting in the fracture, with tearing of the dura so that cerebrospinal fluid (CSF) leaks to form a collection. Because the CSF is under pressure and pulsatile, a transmitted pulsation from the subarachnoid space into the extra-axial fluid collection causes pressure enlargement of the fracture.
Lateral skull radiograph in a child with a growing fracture. The mechanism of injury is usually a direct force applied to the cranial vault, resulting in the fracture, with tearing of the dura so that cerebrospinal fluid (CSF) leaks to form a collection. Because the CSF is under pressure and pulsatile, a transmitted pulsation from the subarachnoid space into the extra-axial fluid collection causes pressure enlargement of the fracture.
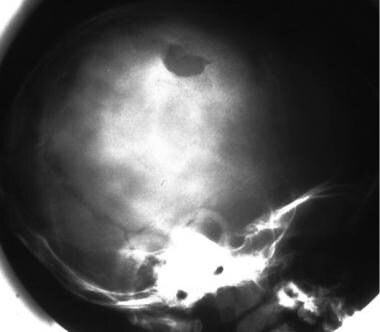 Lateral skull radiograph in a child with a growing fracture. The mechanism of injury is usually a direct force applied to the cranial vault, resulting in the fracture, with tearing of the dura so that cerebrospinal fluid (CSF) leaks to form a collection. Because the CSF is under pressure and pulsatile, a transmitted pulsation from the subarachnoid space into the extra-axial fluid collection causes pressure enlargement of the fracture.
Lateral skull radiograph in a child with a growing fracture. The mechanism of injury is usually a direct force applied to the cranial vault, resulting in the fracture, with tearing of the dura so that cerebrospinal fluid (CSF) leaks to form a collection. Because the CSF is under pressure and pulsatile, a transmitted pulsation from the subarachnoid space into the extra-axial fluid collection causes pressure enlargement of the fracture.
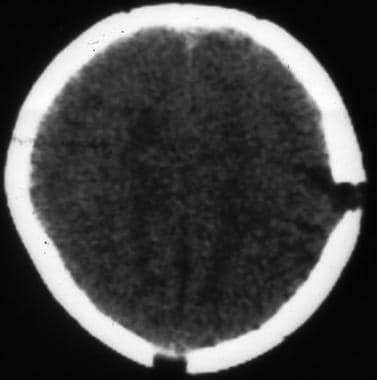 Axial computed tomography scan shows a growing skull fracture nicely, depicting the widened fracture on the left and the fluid collection extending from the intracranial cavity into and through the fracture site.
Axial computed tomography scan shows a growing skull fracture nicely, depicting the widened fracture on the left and the fluid collection extending from the intracranial cavity into and through the fracture site.
CT scanning is an excellent modality at demonstrating intermediate and late sequelae of head trauma, such as hydrocephalus, generalized brain atrophy, encephalomalacia, porencephaly, subdural hygroma (see the image below), leptomeningeal cysts, and vascular complications.
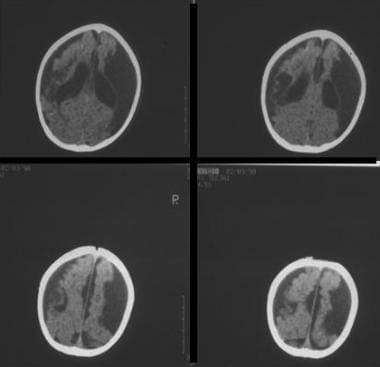 Computed tomography scans of a baby demonstrate bilateral subdural collections of cerebrospinal fluid (CSF) attenuation that are larger on the left than on the right. These are probably subdural hygromas (because the fluid is almost certainly CSF), rather than subdural hematomas or effusions (which would have attenuation higher than that of CSF). The brain is atrophic. Note the relative absence of mass effect despite the bilateral collections. Also note atrophic enlargement of the ventricles.
Computed tomography scans of a baby demonstrate bilateral subdural collections of cerebrospinal fluid (CSF) attenuation that are larger on the left than on the right. These are probably subdural hygromas (because the fluid is almost certainly CSF), rather than subdural hematomas or effusions (which would have attenuation higher than that of CSF). The brain is atrophic. Note the relative absence of mass effect despite the bilateral collections. Also note atrophic enlargement of the ventricles.
Degree of confidence
A skull fracture indicates significant head injury. CT scanning accurately documents the skull fracture, the degree of depression, and the extent of intracranial damage.
A linear or minimally depressed fracture may be easily overlooked on CT scans, as can fractures at the skull vertex. Basilar skull fractures are often difficult to demonstrate on conventional radiographs and CT scanning. In patients with shearing injury of the white matter, a CT scan may initially be normal.
Although CT scanning is highly accurate in depicting recent subarachnoid hemorrhage, the differentiation of interhemispheric blood from a relatively attenuating falx cerebri may be difficult. The differentiation can usually be made by paying attention to the distribution of blood, which usually extends into the paramedian sulci, where it produces an attenuating, irregular, dentate appearance.
An interhemispheric subdural hematoma may mimic a subarachnoid hemorrhage. After several days, subarachnoid blood adjacent to the falx usually clears. In comparison, an interhemispheric subdural hematoma appears as a wedge-shaped, smooth-bordered, hyperattenuating lesion that clears more slowly.
Intracerebral hematomas are usually irregular in shape and tend to be multiple; spontaneous hematomas are generally solitary and spherical.
Metallic foreign bodies from bullet fragments, shotgun pellets, or knife blades produce artifacts that degrade image quality. Exact localization of nonmetallic objects, such as wood or glass, on CT scans may be problematic because of their variable attenuation values.
In a study of preoperative CT scans in 141 patients with calvarial skull fractures, the number of fractured calvarial bones was found to be an independent predictor of outcome in traumatic brain injury patients after early craniotomy. [17]
Magnetic Resonance Imaging
MRI is a sensitive modality in the detection and characterization of both subacute and chronic brain injuries. Brain abnormalities on MRI have been used to predict the recovery outcomes of patients in the posttraumatic vegetative state. Although CT scanning is sensitive for injuries requiring a change in treatment, MRI is also used to assess acute head injury in patients with nonsurgical and medically stable pathology.
Some authors now advocate the use of MRI instead of CT scanning in the assessment of neurologically stable patients with moderate to severe closed head injury, whereas CT scanning is reserved for patients who are neurologically unstable. Although the substitution of MRI for CT scanning does not alter surgical management, the superior depiction of nonsurgical lesions with MRI could help optimize medical management and help predict the success of neurologic recovery.
MRI is better than CT scanning in depicting axonal injury, small areas of contusion, and subtle neurologic damage. However, they are equivalent in the diagnosis of surgically correctable lesions in the acute setting. Pitts found that 10% of patients discharged from the emergency department after minor head injury had abnormalities detected on MRI; however, this added information did not affect their care. [24]
(Below are CT scan images from a child with a high-impact injury with MRI follow-up images.)
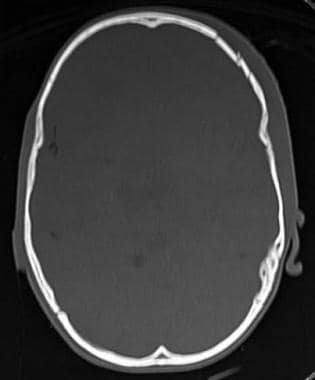 Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
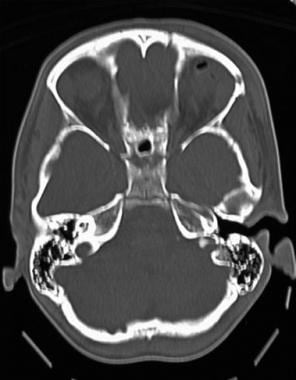 Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
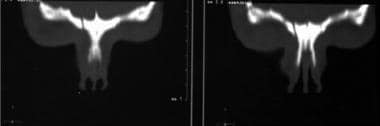 Computed tomography scans in a child with a high-impact injury to the frontoethmoid region show a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scans of the maxillofacial skeleton nicely show the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
Computed tomography scans in a child with a high-impact injury to the frontoethmoid region show a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scans of the maxillofacial skeleton nicely show the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
 Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
 Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
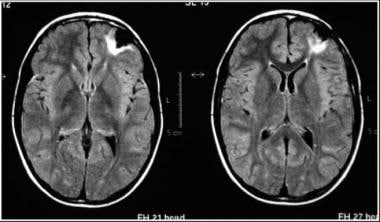 Axial fluid-attenuated inversion recovery (FLAIR) magnetic resonance images obtained at 2-year follow-up of a child who had a high-impact injury to the frontoethmoid region demonstrate focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
Axial fluid-attenuated inversion recovery (FLAIR) magnetic resonance images obtained at 2-year follow-up of a child who had a high-impact injury to the frontoethmoid region demonstrate focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
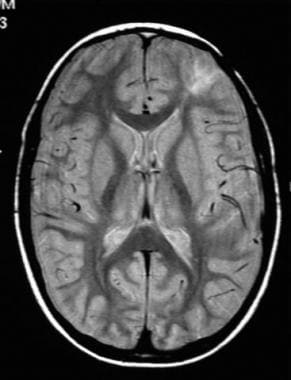 Axial proton density–weighted magnetic resonance image obtained at 2-year follow-up of a child who had a high-impact injury to the frontoethmoid region demonstrate focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
Axial proton density–weighted magnetic resonance image obtained at 2-year follow-up of a child who had a high-impact injury to the frontoethmoid region demonstrate focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
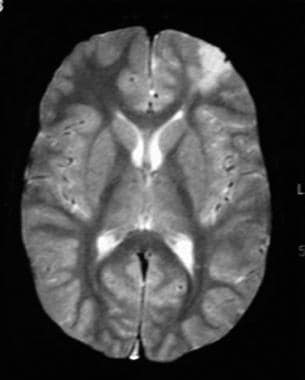 Axial T2-weighted axial MRI obtained at 2-year follow-up demonstrates focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
Axial T2-weighted axial MRI obtained at 2-year follow-up demonstrates focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
T2-weighted gradient-echo sequences are hemosiderin sensitive and useful in imaging small intracerebral hemorrhages, whereas diffusion-weighted images (DWIs) improve the detection of cerebral infarction associated with head injuries. Fluid attenuation inversion recovery (FLAIR) sequences are more sensitive in depicting subarachnoid hemorrhage than conventional MRI sequences. Lang et al found that the addition of gadolinium enhancement offered no notable advantage in lesion detection or characterization, as compared with nonenhanced MRI, in patients with head injury. [25]
Freund et al compared MRI findings with CT findings in 30 patients and found that MRI can demonstrate orbital floor fractures as sensitively as CT scanning but that CT scanning is superior to MRI in showing small and associated fractures. [26] Therefore, CT scanning remains the imaging modality of choice for assessing orbital fractures. However, MRI is superior to CT scanning in showing soft-tissue herniations; therefore, MRI may have a role as an adjunct to CT scanning if soft-tissue entrapment remains unclear. [26]
Gadolinium warning
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more information, see the eMedicine topic Nephrogenic Systemic Fibrosis. The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see the FDA Public Health Advisory or Medscape.
Degree of confidence
The sensitivity and specificity of MRI in detecting skull fractures is low, and fractures are easily missed. MRI is of ancillary value for suspected ligamentous and vascular injuries; however, MRI reportedly depicts cerebral lesions better than CT scanning. [27] . Bony injuries are better visualized by CT scanning than by MRI. Although advances in MRI will undoubtedly increase its use, particularly in the subacute period, CT scanning will likely continue to have a primary role in the management of these injuries in the foreseeable future.
Fiser et al evaluated the role of MRI and resource utilization in traumatic brain injuries (TBIs) and found that although MRI depicts lesions not evident on CT scans, MRI does not alter management plans and is of limited value in the acute management of acute brain injury. [27] However, MRI may be of medicolegal benefit in cases of child abuse. [27]
Ultrasonography
Ultrasonography is not reliable in the diagnosis of skull fractures and neuronal injury. Fractures of the skull base may be especially difficult to image. The role of transcranial Doppler ultrasonography in the evaluation of head injury has not been ascertained. However, transcranial Doppler ultrasonographic imaging offers a noninvasive bedside study with which to assess cerebral blood flow velocity and resistance in the major proximal vessels of the circle of Willis. Results of several studies have suggested that transcranial Doppler ultrasonography can be used to monitor early changes in blood flow velocities that may be related to vasospasm, hypervolemia, or edema.
In a study of 18 patients with orbital trauma, Forrest et al concluded that orbital ultrasonography was an accurate diagnostic modality in the investigation of orbital trauma and that the results were well correlated with CT findings. [28]
Lata and associates evaluated the role of real-time ultrasonography in 19 patients with orbital trauma and reported that this imaging modality adequately displayed the anatomic features of the orbit and depicted clinically significant fractures, suggesting this technique may have a role in posttraumatic imaging of the orbit when coronal CT scanning is not possible. [29]
In addition, Decarie and Mercier found that ultrasonography is a promising tool for assessing the state of the dura in patients with a diastatic skull fracture. [30] Ultrasonograms can be used to identify patients at high risk for complications associated with this type of fracture as early as possible, which helps keep neurosurgical repair as simple as possible.
Nuclear Imaging
SPECT, PET, and xenon-enhanced CT scanning do not provide the anatomic detail or the imaging resolution of CT scanning or MRI to demonstrate acute or neurosurgical lesions in patients with a closed head injury.
CSF rhinorrhea can be detected and localized by using overpressure cisternography with 99mTc DTPA. Although radionuclide cisternography can demonstrate a leak into the nasal cavity or ear, it fails to delineate the fistula site.
Curnes et al performed 32 overpressure radionuclide cisternographic studies to examine 26 patients with clinically suspected CSF fistula with rhinorrhea and determined these are safe, rapid, and accurate methods of investigating a suspected or proven CSF rhinorrhea and that they are complementary to metrizamide cisternography. [31] In addition, Frick et al described radioisotope cisternography as a proven and valuable diagnostic procedure in patients with CSF rhinorrhea. [32] They concluded, however, that defining the origin of the leak is not possible and that extensive intracranial exploration may be required, which may or may not result in successful correction of the defect.
Cowan and associates showed residual oropharyngeal 99mTc activity on an 111In-DTPA cisternogram, which created the appearance of a CSF leak. [33] They suggested that this mimic can be prevented by using a spectrometric setting that encompasses only the higher principal photopeak of 111In.
As a functional examination with limited risk to the patient and minimal radiation exposure, isotopic cisternography can be used to establish a diagnosis of CSF rhinorrhea or eliminate CSF as a cause of rhinorrhea. A CSF leak can be depicted as a path extending from the cranial fossa into the nasal cavity. In the present technique, tampons are placed in each nostril. CSF rhinorrhea is diagnosed when a tampon is impregnated with at least twice the radioactivity of the control tampon in the opposite nostril (in the presence of an intact septum). A positive anterior fossa cisternogram may be the only evidence of a hidden site of CSF leakage, especially when other signs are lacking.
Functional imaging, such as SPECT and PET scanning, may have a role in the evaluation of select patients with head injury in conjunction with cognitive and neuropsychologic disturbances. SPECT scanning may reveal focal areas of hypoperfusion that are discordant with MRI or CT scan findings. Results of functional imaging may explain or be predictive of postinjury neuropsychologic and cognitive deficits that are not explained on MRI or CT scanning. Furthermore, focal lesions demonstrated on SPECT studies offer objective evidence of organic injury in patients whose anatomic images are otherwise normal. Oder et al showed that a pattern of global reduced cerebral blood flow on SPECT evaluation was predictive of a poor likelihood of recovery in patients in a persistent vegetative state because of head injury. [34]
Angiography
Angiography remains the criterion standard for the assessment of vascular injuries, although it is being challenged by CTA and MRA. MRA is sensitive for diagnosis and follow-up of vertebral or carotid artery dissection. Nevertheless, angiography remains the mainstay for endovascular intervention. Vascular injuries typically occur with penetrating injury, basal skull fracture, or trauma to the neck. With the advent of CT scanning, the need for cerebral angiography to assess head injury has declined considerably.
Cerebral angiography is often used for traumatic vascular injuries, such as pseudoaneurysm, dissection, arteriovenous fistulas, and dural venous injuries. It is also used for diagnosing and performing neurointerventions for uncontrolled hemorrhage.
MRA is useful in depicting vascular lesions associated with head injury.
-
Diagram of the cranium shows the anatomic layers.
-
Diagram of the skull vault shows the location of various collections of fluid and/or blood.
-
Occipital skull fracture due to a nonaccidental injury in a toddler.
-
Lateral skull radiograph in a child shows a long, linear fracture extending from the midline in the occipital region across the occipital bone into the temporal bone. The fracture is more radiolucent than the other sutures, has no serration along its edges, and is blind ending. At the blind end, it is more tapered than it is at the sutural or proximal end. Note the lack of branches.
-
Skull radiograph in a man shows a linear temporoparietal fracture.
-
Lateral skull radiograph in a child shows a long, linear fracture running across the occipital bone. Note its radiolucency and straightness and the lack of branches from it. This is not a vessel and not a known site for a suture.
-
Lateral skull radiograph in a child shows an occipital fracture. It has a sclerotic margin and is therefore likely to be depressed. This is an example of a nonaccidental injury.
-
Plain radiographs of the head of a 25–year-old man who was assaulted with a baseball bat show a curvilinear shadow indicating a depressed fracture.
-
Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma show a diastatic fracture of the sagittal suture.
-
Postmortem radiograph in a child with multiple fractures due to nonaccidental trauma shows a diastatic fracture of the sagittal suture.
-
Axial nonenhanced computed tomography scan of the brain shows an open comminuted fracture of the left parietal bone with an underlying extradural hematoma. Air is tracked from the scalp tissues through the fracture into the hematoma.
-
Axial brain computed tomography scans show the reversal sign, brain swelling, hypoxic/ischemic injury, and high attenuation along the free edges of the tentorium and over the tentorium itself; this finding is almost certainly the result of increased intracranial pressure, which causes venous engorgement rather than clotted blood.
-
Axial bone-window computed tomography scans show swelling of the soft tissue overlying a left parietal fracture (arrow).
-
Axial brain and bone-window computed tomography scans show multiple fractures involving the right temporal and parietal bones, with depression of several bone fragments into the brain around which contusional hemorrhage is present. Also present are soft-tissue swelling, air in the cranial cavity related to the bone fragments, and air in the subarachnoid space.
-
Axial brain and bone-window computed tomography scans show multiple fractures involving the right temporal and parietal bones, with depression of several bone fragments into the brain around which contusional hemorrhage is present. Also present are soft-tissue swelling, air in the cranial cavity related to the bone fragments, and air in the subarachnoid space.
-
Axial brain and bone-window computed tomography scans show an extensive comminuted and markedly depressed open fracture in the left temporoparietal region. Note the soft-tissue swelling associated with air in the soft tissues and intracranial region. The fracture extends into the petrous bone. Contusion of the underlying brain is noted.
-
Axial brain and bone-window computed tomography scans show an extensive comminuted and markedly depressed open fracture in the left temporoparietal region. Note the soft-tissue swelling associated with air in the soft tissues and intracranial region. The fracture extends into the petrous bone. Contusion of the underlying brain is noted.
-
Axial brain computed tomography scans show bilateral contusion and intracerebral hematoma in the frontal extradural and right temporal regions, with features of increased intracranial pressure. The hematoma is adjacent to the attachment of the tentorium to the skull vault; this is a site commonly associated with contrecoup hematomas, because the brain moves but the dura cannot.
-
Axial computed tomography scans show penetrating injury from a low-velocity bullet. The entry site is the frontal bone; note the intracranial metallic bone attenuations, intracranial air, cerebral edema, and subarachnoid hemorrhage.
-
Computed tomography scans of the head show air in the cranium, intracerebral hematoma, and cerebral edema due to a high-velocity gunshot wound. The presence of the reversal sign suggests severe brain swelling and probably secondary hypoxic ischemic injury to the brain as a result of the pressure on the brain.
-
Axial nonenhanced brain computed tomography scans show a left frontal subdural hematoma, which is not totally homogeneous probably because unclotted blood is mixed with it; this implies active hemorrhage.
-
Axial nonenhanced computed tomography scans shows an extradural hematoma anterior to the left temporal lobe (blue arrows). Red arrows point to an extradural hematoma over the upper part of the left temporal lobe. The hematoma in this region is not totally homogeneous, probably because unclotted blood is mixed with it; this implies active hemorrhage. The green arrow points to a small bubble of air in the hematoma, which suggests an open compound fracture. Despite the extradural hematoma, gray matter is clearly distinguishable from white matter, and the ventricles are of normal size. These findings suggest no serious elevation of intracranial pressure at this early stage.
-
Computed tomography scans show the effect of a direct impact to the left frontal region that resulted in an extracranial hematoma and an intracranial extradural hematoma. Contrecoup hemorrhages are seen in the right temporal region.
-
Bone-window computed tomography scan shows a fracture of the frontal bone. Note the fluid level in the frontal sinus, which suggests that clotted blood is layering out.
-
Bone-window axial computed tomography scans of the maxillofacial skeleton and orbits demonstrate extensive fractures of the entire maxillofacial complex, including the medial walls of the orbits, the medial walls of the antra, and the posteroinferior walls of the antra (in fact all the bones). The pterygoid plates are intact, and the midface is not displaced or dislocated.
-
Axial computed tomography scan demonstrates an open comminuted and depressed frontal bone fracture with clotted blood along the interhemispheric fissure. Contusional hemorrhage is present in the left frontal lobe, as is a left-sided temporal extradural hematoma containing a small pocket of air; this finding implies an open fracture. The temporal horns are slightly dilated, suggesting the development of hydrocephalus.
-
Computed tomography scans show bilateral isoattenuating subdural collections and no extradural ones.
-
Axial nonenhanced brain computed tomography scan shows a right frontal extradural hematoma. Note that the deep aspect of the hematoma is homogeneously white (high attenuation), whereas the peripheral or outer part is more isoattenuating relative to the brain. The reason for this lack of homogeneity is the presence of clotted blood (white) and unclotted blood (dark) within the hematoma. Three reasons are possible: The most common reason is that the patient is actively bleeding when the hematoma occurred and that the blood has not yet clotted. The second is that the patient was taking anticoagulants, which delayed the clotting time. The third possibility is consumption coagulopathy, in which all the patient's clotting factors are used up in other sites of trauma.
-
One of a series of 5 sets of computed tomography scans with coronal and sagittal reconstructions show multiple fractures. This image shows a blowout fracture of the left orbit with a hematoma in the left maxillary antrum and probable herniation of orbital contents into the widely separated or open fracture. Also present is a fracture of the medial wall of the maxillary antrum on the left, and a small pocket of air has migrated from the maxillary antrum into the orbit. Herniation of orbital contents through the defect is likely.
-
One of a series of 5 sets of computed tomography scans with coronal and sagittal reconstructions show multiple fractures. This image shows a blowout fracture of the left orbit with a hematoma in the left maxillary antrum and probable herniation of orbital contents into the widely separated or open fracture. Also present is a fracture of the medial wall of the maxillary antrum on the left, and a small pocket of air has migrated from the maxillary antrum into the orbit. Herniation of orbital contents through the defect is likely.
-
One of a series of 5 sets of computed tomography scans with coronal and sagittal reconstructions show multiple fractures. This image shows a blowout fracture of the left orbit with a hematoma in the left maxillary antrum and probable herniation of orbital contents into the widely separated or open fracture. Also present is a fracture of the medial wall of the maxillary antrum on the left, and a small pocket of air has migrated from the maxillary antrum into the orbit. Herniation of orbital contents through the defect is likely.
-
One of a series of 5 sets of computed tomography scans with coronal and sagittal reconstructions show multiple fractures. These images show a blowout fracture of the left orbit with a hematoma in the left maxillary antrum and probable herniation of orbital contents into the widely separated or open fracture. Also present is a fracture of the medial wall of the maxillary antrum on the left, and a small pocket of air has migrated from the maxillary antrum into the orbit. Herniation of orbital contents through the defect is likely.
-
One of a series of 5 sets of computed tomography scans with coronal and sagittal reconstructions show multiple fractures. This image shows a blowout fracture of the left orbit with a hematoma in the left maxillary antrum and probable herniation of orbital contents into the widely separated or open fracture. Also present is a fracture of the medial wall of the maxillary antrum on the left, and a small pocket of air has migrated from the maxillary antrum into the orbit. Herniation of orbital contents through the defect is likely.
-
Axial nonenhanced computed tomography scans of the brain demonstrate a right-sided extradural hematoma, which is not homogeneous in its attenuation; this finding suggests the presence of unclotted blood. The images show considerable mass effect on the underlying brain, with subfalcine herniation of the brain to the right side, with a contrecoup left temporal hematoma, and hemorrhage around the anterior aspect of the falx.
-
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
-
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
-
Computed tomography scans in a child with a high-impact injury to the frontoethmoid region show a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scans of the maxillofacial skeleton nicely show the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
-
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
-
Computed tomography scan in a child with a high-impact injury to the frontoethmoid region shows a comminuted fracture in the left frontal bone and disruption of the left orbit with air in the orbital cavity. Reformatted 3-dimensional scan of the maxillofacial skeleton nicely shows the fracture on the left, which involves the frontal and ethmoidal bones and the medial plate of the left orbit (ie, this is a complex fracture involving 3 bones).
-
Axial fluid-attenuated inversion recovery (FLAIR) magnetic resonance images obtained at 2-year follow-up of a child who had a high-impact injury to the frontoethmoid region demonstrate focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
-
Axial proton density–weighted magnetic resonance image obtained at 2-year follow-up of a child who had a high-impact injury to the frontoethmoid region demonstrate focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
-
Axial T2-weighted axial MRI obtained at 2-year follow-up demonstrates focal cystic atrophy in the left frontal region (black) and gliosis of the brain (white). Gliosis is a highly cellular response of the brain to injury and is, in effect, scar tissue. It has high signal intensity partly because of its high cellular content and also because of the absence of normal neural structures.
-
Computed tomography scan of an 8-week-old baby after forceps delivery shows a major insult to the left cerebral hemisphere, which is now atrophic. This scan shows hypoattenuating areas in the brain parenchyma, with dilatation of the ipsilateral lateral ventricle and a midline shift toward the atrophic side.
-
Computed tomography scan of a newborn with hemophilia shows an extensive extracranial hematoma present immediately after birth, a blood clot draped over the tentorium, and an axial blood clot overlying the bilateral temporal lobes.
-
Computed tomography scans of a patient who was attacked with an ax show an open midline frontal fracture, with air in the extracranial soft tissues, air in the fracture itself, and air in the brain underlying it. Also present is contusional hemorrhage in the frontal region of the brain. A clotted blood is seen in the lateral third and fourth ventricles, which are slightly dilated.
-
Lateral skull radiograph shows the importance of having the patient positioned straight for lateral imaging. Because the patient is slightly malpositioned, both coronal sutures are seen as separate entities. This problem also applies to the lambdoid sutures; because they are separated, one could be mistaken for a fracture. Accessory occipital sutures are also exaggerated by the patient's rotation.
-
Anteroposterior (AP) skull radiograph in a child shows the sagittal and lambdoid sutures and a prominent squamous cell suture on the right side. None of these are fractured, and all have serrated edges. The sutures communicate one with another; they are not blind ending. The child is probably younger than 1 year.
-
Lateral skull radiograph shows the normal bilateral squamous temporal sutures, not to be confused with fractures.
-
Frontal skull radiograph of a child shows the usual coronal and sagittal sutures. On the left is an accessory suture, which is seen to extend from the squamous central suture to the lambdoid suture. Although fractures and sutures can be difficult to differentiate, the accessory suture can be identified as such because it connects 2 sutures, has an even caliber and radiopacity throughout, and has slightly serrated edges. In general, when a fracture connects 2 sutures, the fracture line is wide open or open mouthed at the sutural connection and is narrowest away from the suture. In this case, the fracture line is of even caliber all the way across.
-
Frontal skull radiograph shows a persistent metopic suture that has not yet fused; this is not a fracture.
-
Vessel markings simulating a fracture.
-
Frontal skull radiograph demonstrates a left-sided fracture. The fracture is radiolucent and wide, and it courses without interruption across the occipital and parietal bones. The other side shows a vascular marking of similar radiolucency, but it is of even caliber and its origin in the occipital region is from another vessel.
-
Lateral skull radiograph demonstrates a left-sided fracture. The fracture is radiolucent and wide, and it courses without interruption across the occipital and parietal bones. The other side shows a vascular marking of similar radiolucency, but it is of even caliber and its origin in the occipital region is from another vessel.
-
Skull radiograph in a premature baby. The skull vault develops in membrane, whereas the skull base develops in cartilage. When ossification of the skull vault is impaired or premature, the frontal, temporal, and parietal bones form reasonably well but do not meet in the midline. As a result, the outer table of the skull is often not visible on a lateral skull radiograph. Moreover, the sutures appear to be widened, but only because the bone margins have not come together and because of increased intracranial pressure.
-
Lateral skull radiograph in a child with a growing fracture. The mechanism of injury is usually a direct force applied to the cranial vault, resulting in the fracture, with tearing of the dura so that cerebrospinal fluid (CSF) leaks to form a collection. Because the CSF is under pressure and pulsatile, a transmitted pulsation from the subarachnoid space into the extra-axial fluid collection causes pressure enlargement of the fracture.
-
Lateral skull radiograph in a child with a growing fracture. The mechanism of injury is usually a direct force applied to the cranial vault, resulting in the fracture, with tearing of the dura so that cerebrospinal fluid (CSF) leaks to form a collection. Because the CSF is under pressure and pulsatile, a transmitted pulsation from the subarachnoid space into the extra-axial fluid collection causes pressure enlargement of the fracture.
-
Axial computed tomography scan shows a growing skull fracture nicely, depicting the widened fracture on the left and the fluid collection extending from the intracranial cavity into and through the fracture site.
-
Computed tomography scans of a baby demonstrate bilateral subdural collections of cerebrospinal fluid (CSF) attenuation that are larger on the left than on the right. These are probably subdural hygromas (because the fluid is almost certainly CSF), rather than subdural hematomas or effusions (which would have attenuation higher than that of CSF). The brain is atrophic. Note the relative absence of mass effect despite the bilateral collections. Also note atrophic enlargement of the ventricles.
-
Lateral computed tomography (CT) scanogram and axial bone-window CT scan demonstrate a temporal fracture. The CT scan shows slight inward bulging of the bone, but the inner and outer tables are intact. This is a classic ping-pong ball fracture roughly akin to a greenstick fracture in a long bone. This fracture only occurs in children because the skull vault is more elastic and less rigid than it is in adults.
-
Lateral skull radiograph in a premature neonate shows relative radiolucency of the calvarium because the membrane bone is not fully ossified. The coronal and sagittal sutures appear to be wide; this is not because of increased pressure but because the membranous bone is not fully ossified, and therefore, it has not reached the sutural margin of the bone.
-
The normal parietal suture (arrows) should not be mistaken for a fracture.
-
Left: Towne view of the skull shows a central suture (arrow). This anomalous midline occipital suture (cerebellar synchondrosis) is a normal anatomic variant. Differentiation from a skull fracture is important, because the occipital bone is a common site of a fracture in children. Right: Radiograph shows an occipital fracture (arrow).
-
A frontal skull radiograph showing a metopic suture.
-
A missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
-
Computed tomography scan of a missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
-
Computed tomography scan of a missile injury through the frontal bone associated with an intracerebral hematoma/infarction along the missile tract.
-
A plain radiograph of the facial bones shows a right orbital floor fracture associated with orbital emphysema.
-
A plain radiograph of the facial bones shows features suggestive of a right orbital floor fracture. See the next image.
-
Coronal computed tomography sections of the orbits in the same patient as the previous image show no fracture.