Practice Essentials
Midgut volvulus is a condition in which the intestine has become twisted as a result of malrotation during. Malrotation of the intestine occurs when the normal embryologic sequence of bowel development and fixation is interrupted. Although midgut volvulus is a complication of malrotation of bowel and mesenteric malfixation, primary volvulus of the small bowel is a distinctly different and rare entity characterized by torsion of the entire small bowel with normal mesenteric fixation. [1] The condition can occur at any age but is more frequent in infants and children. [2, 3, 4, 5]
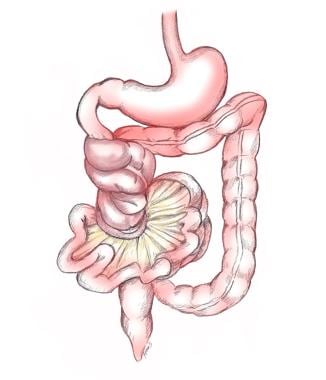
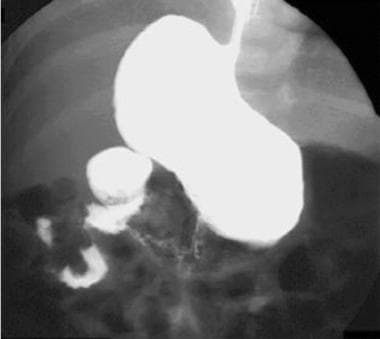
The malrotated bowel is prone to torsion (as demonstrated in the first image below), which can lead to midgut volvulus. The second image, from a GI series, shows a lateral view of midgut volvulus.
In neonates, malrotation with midgut volvulus classically presents with bilious vomiting and, as the radiograph below demonstrates, high intestinal obstruction. While most neonates with bilious vomiting do not have midgut volvulus, this diagnosis must be excluded.
Older children with malrotation may manifest a failure to thrive, chronic recurrent abdominal pain, malabsorption, or other vague presentations. The older the child, the less clear the clinical presentation. Nonrotation of the intestine may be asymptomatic and is an incidental finding on upper GI series performed for other reasons.
Associated anomalies are seen in approximately 60% of patients and include congenital heart disease with heterotaxy (abnormal positioning and arrangement of the abdominal organs, such as the spleen, liver, and major blood vessels; right-sided or left-sided isomerism). Malrotation is almost always present in patients with congenital diaphragmatic hernia and abdominal wall defects, such as omphalocele and gastroschisis. Also, malrotation is more common with imperforate anus, duodenal atresia, duodenal web, duodenal stenosis, preduodenal portal vein, annular pancreas, Hirschsprung disease, and biliary atresia. [6] .
In a meta-analysis, the incidence of rotational abnormalities and incidence of acute midgut volvulus were significantly greater in patients with heterotaxy than in the normal population. The prophylactic Ladd procedure was associated with less morbidity and mortality than with emergency surgery. [7] The Ladd procedure consists of division of Ladd bands, widening of the mesentery, and incidental appendectomy. [4]
(Malrotation in a patient with congenital heart disease and heterotaxy is shown below.)
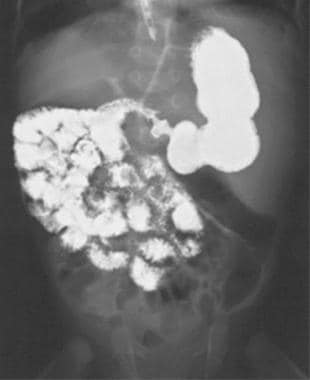 Upper GI series and a small bowel study show malrotation without midgut volvulus in a patient with complex congenital heart disease and heterotaxy. Note the small bowel in the right abdomen.
Upper GI series and a small bowel study show malrotation without midgut volvulus in a patient with complex congenital heart disease and heterotaxy. Note the small bowel in the right abdomen.
ACR guidelines
The American College of Radiology recommendations for imaging of vomiting infants are based on the age of the infant. For vomiting within the first 2 days after birth, abdominal radiography is usually appropriate for initial imaging. In the case of radiographic findings of a classic double-bubble or triple-bubble sign with little or no gas distally, which are common indications of obstruction of the duodenum, a fluoroscopic upper GI series may be appropriate if another rare cause is suspected. In the case of a nonclassic double-bubble sign with gas in the distal small bowel, few distended bowel loops, or a normal bowel gas pattern on initial radiographs, a fluoroscopic upper GI series is usually appropriate to differentiate between congenital intestinal atresia and stenosis and midgut volvulus. For bilious vomiting in infants older than 2 days, a fluoroscopic upper GI series is usually appropriate for initial imaging. [8]
The ACR has noted that there is limited evidence supporting the use of ultrasonography for primary evaluation of malrotation and midgut volvulus. However, they have noted that there are some studies showing high sensitivity and specificity for diagnosis of midgut volvulus, particularly when the whirlpool sign is present. [8, 9, 10, 11]
Imaging modalities
The diagnostic test of choice in a child with possible malrotation, with or without midgut volvulus, is an upper GI series. [12, 13] In a study by Sizemore et al, an upper GI series in the detection of intestinal malrotation in infants and youths had a sensitivity of 96%, providing positive results in 156 of the 163 patients with surgically verified malrotation. In addition, the series showed midgut volvulus in 30 of 38 patients in whom volvulus was surgically verified (sensitivity, 79%). Data from the study indicated that jejunal position can result in inaccurate interpretation of an upper GI series. [12]
Midgut volvulus, although rare, can cause high duodenal obstruction. In these cases, the abdominal radiograph can mimic the classic appearance of the double-bubble sign of duodenal atresia (the first bubble corresponds to the stomach, and the second bubble to the dilated duodenal loop). Gilbertson-Dahdal et al recommended performing an upper GI radiographic or ultrasound study to identify possible malrotation with midgut volvulus when there is delay in surgical treatment of patients with the double-bubble sign. [14]
In most patients with malrotation, an upper GI series is easy to perform and, in experienced hands, is easy to interpret, with the following exceptions:
-
With complete duodenal obstruction, an upper GI series does not differentiate between the causes of proximal intestinal obstruction. In such cases, surgical exploration is indicated.
-
A redundant duodenum, seen in some normal individuals, can be confused with malrotation. Careful tracking of the barium shows a normal duodenojejunal junction (DJJ); if uncertainty exists, a contrast enema can confirm normal rotation if the cecum is seen in the right lower quadrant.
A false-negative diagnosis of malrotation with midgut volvulus can lead to delays in the diagnosis and, possibly, death or severe morbidity. False-negative diagnoses result from misinterpretation of a finding as a normal variant. [6, 15] A false-positive diagnosis can lead to an unnecessary laparotomy and a delay in obtaining the correct diagnosis. False-positive conclusions occur when there is failure to recognize normal variations, such as redundant or wandering duodenum, duodenum inversum, or mobility of the DJJ. The DJJ can be mobile in children younger than 4 years, and displacement can occur in cases of gaseous distention of the stomach or bowel, as well as intra-abdominal processes that cause mass effect.
The highest sensitivities and specificities with upper GI series are in pediatric centers where operators with experience and pediatric expertise perform the examinations. If the upper GI results are in question, the examination should be repeated through a nasogastric feeding tube, or the study should be continued to determine the position of the cecum, because the cecum is abnormal in 80% of patients with malrotation. [6]
Katz et al proposed 9 findings on upper GI series to detect subtle abnormalities. Three or more abnormalities indicated malrotation, the presence of 2 abnormalities was considered indeterminate, and 1 abnormality represented normal variation. [16] Findings included assessment of the location of the pylorus, 3 descriptors of the duodenojejunal junction, 3 descriptors of the segment between the inferior-most and duodenojejunal flexures, and the course and positioning of the jejunum.
Long et al applied the Katz criteria in difficult-to-diagnose cases. In their series, 9 patients with malrotation only had 1 of the Katz criteria. They suggested the possibility of malrotation and further evaluation if the jejunum is in the right upper quadrant, if the DJJ is slightly low, or if there is unusual redundancy of the duodenum. Although redundancy of the sweep can be normal, they describe features suggestive of malrotation that include the following [15] :
-
Angularity or kinking of the loops (due to Ladd bands)
-
Formation of more than a single loop in the course of the sweep
-
Unusual redundancy
The relationship between the superior mesenteric vein and artery is also important in the assessment for malrotation and volvulus. Normally, the superior mesenteric vein lies to the right of the superior mesenteric artery at the level of the confluence of the superior mesenteric vein (SMV) and portal vein. This relationship can be readily assessed by ultrasonography. Reversal of this relationship may suggest malrotation, and correlation with patient presentation and upper GI series is warranted. Conversely, normal orientation of these vessels does not exclude malrotation. In Taylor's series of 38 surgically proven cases of malrotation, 11 patients had a normal SMV/SMA relationship. [17] If clinical suspicion is high, further evaluation should be undertaken with an upper GI series.
In symptomatic patients with midgut volvulus who undergo computed tomography or ultrasonography, the whirlpool sign can be seen, which represents the clockwise rotation of the SMV, mesentery, and small bowel loops, twisting around the SMA. This finding is specific for volvulus. The reference point of the clock direction is the appearance on an axial slice of a CT scan where the anterior abdominal wall is at 12 o'clock and the spine is at 6 o'clock. These patients may also have a dilated proximal duodenum. [13]
Case reports of counterclockwise swirling, also known as the barber-pole sign, have been infrequently described in cases of surgically proven midgut volvulus. [18, 19] A normal variant that may be mistaken for swirling of the mesentery is the appearance of the proximal left jejunal veins as they course in a counterclockwise direction to join the superior mesenteric vein. Sodhi et al described 72 patients in a series of 200 consecutive pediatric abdominal CTs, performed for reasons other than evaluation for malrotation and volvulus, with counterclockwise swirling of the proximal mesenteric veins ranging from 90 degrees to more than 270 degrees. [20] In the Taylor series, this pattern was similarly described in 10% of patients without malrotation. [17]
Diagnosis of malrotation with midgut volvulus on fetal magnetic resonance imaging (MRI) has been reported, [21] but in practice, this is a difficult diagnosis to make. MRI is not recommended in infants suspected of having malrotation with midgut volvulus. According to Sciarrone et al, prenatal ultrasonographic signs of midgut volvulus can be direct and specific (eg, whirlpool sign and coffee bean sign) or indirect and nonspecific (eg, abdominal mass, dilated bowel loops, pseudocysts, ascites, and polyhydramnios). [22]
Angiographic abnormalities with chronic volvulus have been well described, and they include proximal occlusion of the SMA, a barber-pole sign (whirling SMA and its branches), [23] extensive collateral vessels, and thickening of the small bowel folds. Angiography is not used to diagnose acute midgut volvulus. The degree of confidence is high, but this examination is rarely indicated.
Pathophysiology
Malrotation of the bowel causes shortening of the mesenteric root, which predisposes to volvulus. Malrotation results from disruption of the normal embryologic development of the bowel. The midgut (middle of duodenum to the splenic flexure of the colon) develops as a long, straight tube with arterial blood flow supplied by the superior mesenteric artery.
By 12 weeks' gestation, it normally has undergone 270-degree counterclockwise rotation (toward the right), so that the duodenojejunal junction (DJJ) is positioned in the left upper quadrant and the cecum is in the right lower quadrant. [24] Once in their final anatomic positions, mesenteric attachments stabilize the position of the bowel loops. If rotation is arrested at any point in the process, these loops reside in abnormal positions in the abdomen and stabilization in the abdomen may fail to occur.
The duodenojejunal loop and cecocolic loops rotate independently of one another. [6, 24] Although most cases of malrotation affect both loops, cases of abnormal duodenojejunal rotation with normal cecal position (and rarely isolated cecocolic malrotation) occur. [25] Long et al described 7 patterns of duodenal malrotation in a series of 69 cases of surgically proven malrotation. Almost all individuals had abnormal fixation of both the duodenum and colon; however, 1 patient had a normal duodenum, and 4 had normal cecal positions. [25]
Ladd procedure
Individuals diagnosed with malrotation who are believed to be at risk for volvulus, as well as those with midgut volvulus, undergo a Ladd procedure. During this procedure, the bowel is untwisted if volvulus is present; adhesive or Ladd bands are resected; the mesentery is widened; the bowel is positioned in the abdomen in a nonrotated orientation (small bowel on the right and colon on the left); and the appendix is removed. Recurrence of volvulus is reported to be less than 1% following this procedure; in cases of recurrence, it may be due to an incomplete initial procedure or decreased formation of adhesions. [26, 27, 4] The most common complication is bowel obstruction due to adhesions. Patients with omphalocele have a greater risk of developing midgut volvulus, and in these patients, a Ladd procedure should be considered during repair to reduce risk. [28]
Prognosis
The prognosis of prenatal intestinal volvulus depends on the length of the segment involved, the level of intestinal obstruction, the presence of meconium peritonitis, and the gestational age at birth. [29] In 30% of patients with midgut volvulus in one study, the only clinical sign was a sudden worsening of the general condition and abdominal distention. Of the 37 children studied, 43% developed complications, and mortality was 16%. [30]
Radiography
An upper GI series is the preferred diagnostic test for malrotation with midgut volvulus and must be performed, unless a delay in surgical treatment will compromise outcome (as in the case of a moribund child). Sensitivity of upper GI series is 85-95%, with a higher specificity (false positives are rare). [6, 12, 13, 31, 32]
In midgut volvulus, the classic radiographic finding is a partial duodenal obstruction (dilation of both the stomach and the proximal duodenum, with a small amount of distal bowel gas). Complete obstruction of the duodenum may also be found. Less frequent, but more ominous, signs are a gasless abdomen, ileus, or a distal small bowel obstruction with multiple dilated loops and air-fluid levels. A normal abdominal film does not exclude malrotation.
The upper GI series is performed with barium administered either orally or through a nasogastric tube. The normal duodenojejunal junction (DJJ) lies to the left of the left-sided spinal pedicle at the level of the duodenal bulb on a true frontal view. The duodenal C-sweep courses posteriorly, inferiorly, anteriorly, and then superiorly.
The findings of a malrotation on upper GI series include the following:
-
The DJJ is displaced downward and to the right on frontal view
-
The duodenum has an abnormal course on lateral view
-
Abnormal positioning of the jejunum (lying on right side of abdomen) should alert the physician to the possibility of a malrotation, but this finding should not be relied upon to either make or exclude the diagnosis
In malrotation with midgut volvulus, the findings also include the following:
-
A dilated, fluid-filled duodenum
-
A proximal small bowel obstruction
-
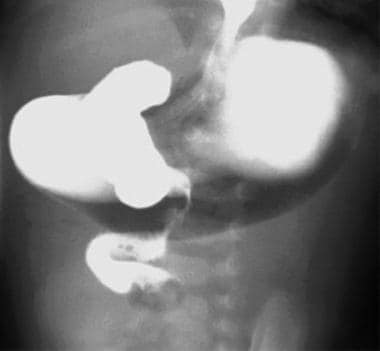
A "corkscrew" pattern (proximal jejunum spiraling downward in the right- or mid-upper abdomen in midgut volvulus, which is rare), as seen in the images below.
-
Mural edema and thick folds
 Upper GI series shows malrotation with midgut volvulus. An incomplete duodenal obstruction and dilation of the first and second portions are seen, as is the "corkscrew sign."
Upper GI series shows malrotation with midgut volvulus. An incomplete duodenal obstruction and dilation of the first and second portions are seen, as is the "corkscrew sign."
False-negatives and false-positives
Normal radiographs are common with malrotation. In malrotation without midgut volvulus, the degree of confidence on plain radiographs is low. Radiographs are rarely normal in malrotation with midgut volvulus, increasing the degree of confidence in this clinical scenario.
Findings in midgut volvulus are nonspecific and can be seen in other conditions that may cause ileus or ischemia, such as acute pyelonephritis, appendicitis, and necrotizing enterocolitis.
Duodenal obstruction, seen in midgut volvulus and malrotation (due to Ladd bands), is also seen with duodenal stenosis, duodenal web, annular pancreas, preduodenal portal vein, and duodenal atresia.
Although a DJJ low and to the right of normal is a sensitive indicator of malrotation, this finding can also be due to other etiologies. Distended bowel, masses, and splenomegaly can displace the DJJ, especially in children younger than 4 years, whose mesenteric attachments are not as well fixed as they are in later years. Scoliosis makes it difficult to exclude malrotation, because the normal bony landmarks are lost.
Radiographic diagnosis can be difficult in patients with intermittent or incomplete small bowel volvulus without malrotation. In young infants, the clinical and imaging findings may mimic necrotizing enterocolitis. [1]
Computed Tomography
CT, while not the preferred examination for evaluation of suspected malrotation, can detect abnormal bowel rotation and volvulus and may be performed in the clinical setting of abdominal pain.
Findings that raise suspicion of malrotation include the following [20, 33] :
-
Inversion of the normal relationship of the SMV and SMA
-
Third portion of the duodenum anterior to the SMA
-
Duodenum not reaching midline
-
Jejunal bowel loops in the right abdomen; ileal bowel loops in the left abdomen
-
Ectopic ileoceal junction
Ultrasonography
Ultrasound signs of intestinal volvulus can be direct and specific (whirlpool sign, coffee bean sign) or indirect and nonspecific (abdominal mass, dilated bowel loops, pseudocysts, ascites, polyhydramnios). [29, 34] Ultrasonography and CT may suggest the diagnosis of malrotation; however, their sensitivities and specificities are lower than those of an upper GI series. An upper GI examination is mandatory to confirm the diagnosis, if it is suspected on CT or ultrasonography. If the SMV lies to the left of or posterior to the SMA (as demonstrated in the CT scan below), malrotation is suggested; however, normal vascular positioning (the SMV being slightly ventral and to the right of SMA) can be seen in approximately 30% of patients with malrotation.
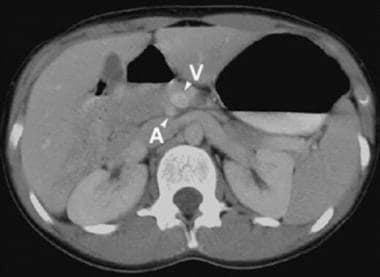 CT scan shows the abnormal relationship of the superior mesenteric vein (SMV) to the superior mesenteric artery (SMA). The SMV should lie to the right of the SMA in this adolescent with undiagnosed malrotation without volvulus (V=SMV, A=SMA).
CT scan shows the abnormal relationship of the superior mesenteric vein (SMV) to the superior mesenteric artery (SMA). The SMV should lie to the right of the SMA in this adolescent with undiagnosed malrotation without volvulus (V=SMV, A=SMA).
The whirlpool sign on color Doppler ultrasonography (as seen in the image below) shows mesentery and flow within the SMV wrapping around the SMA (in a clockwise direction), suggesting, but not entirely specific for, malrotation with midgut volvulus. [35, 36] A dilated, fluid-filled duodenum is frequently seen in patients who have obstruction without volvulus.
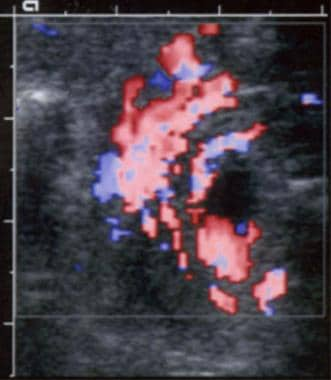 Color Doppler ultrasonographic scan shows malrotation with midgut volvulus demonstrating the "whirlpool sign." The superior mesenteric vein (SMV) in this patient wraps around the superior mesenteric artery (SMA).
Color Doppler ultrasonographic scan shows malrotation with midgut volvulus demonstrating the "whirlpool sign." The superior mesenteric vein (SMV) in this patient wraps around the superior mesenteric artery (SMA).
Ultrasound can be used to assess the position of the third portion of the duodenum, which should be positioned between the SMA and aorta in a normal individual. Yousefzadeh describes this as a more reliable marker of rotation than identifying the duodenojejunal junction (DJJ), because of the inherent mobility of the DJJ in infants and young children. [33] The use of bedside ultrasound to identify the third part of the duodenum in newborns was shown to be successful, providing rapid visualization of this segment in all 33 infants. [37] The authors acknowledged that the technique would need to be assessed in slightly older children, who are the most common group to present with symptoms of malrotation and volvulus. However, other cases have been described of normal positioning of the third portion of the duodenum in the setting of cecal malrotation.
In a retrospective case series of neonatal volvulus by Bartholmot et cl, based on postnatal and prenatal ultrasound imaging findings in 13 patients, a decrease in active fetal movements was reported in 8 patients (61.5%); the prenatal whirlpool sign was directly seen in 10 cases; and a fluid-filled level within the dilated loops was present in 5 cases. [38]
The moderate-to-low degree of confidence associated with ultrasonography and CT necessitates an upper GI series to confirm the diagnosis. [39, 40, 41] Ultrasonography and CT have false-negative rates of approximately 30% and false-positive rates as high as 20%.
-
Malrotation with midgut volvulus shows torsion around the narrow mesenteric stalk.
-
Supine radiograph in a newborn with midgut volvulus shows a high intestinal obstruction.
-
Upper GI series shows malrotation without midgut volvulus in an infant with vomiting but without failure to thrive. The duodenojejunal junction is low and to the right of the spine on this frontal view.
-
Upper GI series shows malrotation with midgut volvulus. An incomplete duodenal obstruction and dilation of the first and second portions are seen, as is the "corkscrew sign."
-
Upper GI series shows malrotation with midgut volvulus in a lateral view.
-
Upper GI series shows the "corkscrew sign" in a frontal view.
-
Upper GI series and a small bowel study show malrotation without midgut volvulus in a patient with complex congenital heart disease and heterotaxy. Note the small bowel in the right abdomen.
-
Color Doppler ultrasonographic scan shows malrotation with midgut volvulus demonstrating the "whirlpool sign." The superior mesenteric vein (SMV) in this patient wraps around the superior mesenteric artery (SMA).
-
CT scan shows the abnormal relationship of the superior mesenteric vein (SMV) to the superior mesenteric artery (SMA). The SMV should lie to the right of the SMA in this adolescent with undiagnosed malrotation without volvulus (V=SMV, A=SMA).