Practice Essentials
Encephalocele represents one end of the spectrum of open neural tube diagnoses. The incidence of encephalocele is estimated at 0.95 in 10,000 live births. The incident is highest among indigenous populations (1.4) and African-Americans (1.34). Whites have the lowest incidence at 0.77 per 10,000 live births. [1] The exact cause of encephalocele is unknown; most likely, the disorder results from the combination of genetic and environmental factors. Encephaloceles are more common in individuals who have a family history of neural tube defects such as spina bifida or anencephaly. No specific environmental factors have been confirmed as contributing to the development of an encephalocele. Certain toxins or infections may be involved. An increased risk for encephalocele in HIV-infected women taking the antiviral dolutegravir at the time of conception has been reported. [2] Pregnant women exposed to Zika virus are at risk for significant fetal brain malformation including encephalocele. [3, 4]
Ultrasonogrpahic (US) scanning remains the mainstay of fetal imaging; there is some evidence, however, that fetal magnetic resonance imaging (MRI) may provide superior detail of central nervous system (CNS) anomalies. [5, 6] With US scanning, the diagnosis is based on the herniation of a spherical, fluid-filled structure, more correctly diagnosed as a meningocele or brain parenchyma (encephalocele) beyond the calvarial confines. The herniation occurs through a calvarial defect. [7]
(Ultrasonographic encephalocele images are shown below.)
 Meckel-Gruber syndrome. Ultrasonograms show oligohydramnios-enlarged echogenic kidneys (left) and a fairly large occipital encephalocele containing brain tissue (right).
Meckel-Gruber syndrome. Ultrasonograms show oligohydramnios-enlarged echogenic kidneys (left) and a fairly large occipital encephalocele containing brain tissue (right).
Radionuclide ventriculography and/or cisternography have been used postnatally to demonstrate the intracranial extension of an encephalocele. Currently, MRI can effectively demonstrate this extension. Radionuclide cisternography can be performed via lumbar puncture or ventricular injection by using technetium-99m (99mTc) diethylenetriamine penta-acetic acid (DPTA) followed by planar imaging or single-photon emission CT (SPECT) scanning.
Angiography may be needed to evaluate intracranial and extracranial vasculature before surgical repair is performed. Angiography is helpful if concern exists regarding the displacement of the dural venous sinus into the sac. Angiography remains the criterion standard for depicting vascular anomalies; however, cerebral angiography is rarely used in the evaluation of an encephalocele. MRI can usually depict the dural venous anatomy.
According to a study of 57 patients with suspected temporal bone encephalocele, CT scans were less sensitive than MRI. CT scanning had a 17% sensitivity, 100% specificity, 100% positive predictive value, and 46% negative predictive value. MRI had a 58% sensitivity, 100% specificity, 100% positive predictive value, and 24% negative predictive value for detecting temporal bone encephalocele. Worrall et al concluded that CT and MRI can provide complementary information that may aid surgical planning but that imaging cannot always rule out temporal bone encephalocele. They added that in cases with high clinical suspicion, surgical confirmation is often required for definitive diagnosis and treatment but that the cost of an additional preoperative study should be considered before its use. [8]
An encephalocele results from failure of the surface ectoderm to separate from the neuroectoderm. This leads to a bony defect in the skull table, which allows herniation of the meninges (cranial meningocele) or of brain tissue. The occiput is the most common site of this type of neural tube defect (75%) in the United States and Western Europe. Approximately 90% of cases involve the midline.
Other malformations and/or chromosomal anomalies are noted in at least 60% of patients with encephalocele. [9, 10] Most cases are diagnosed prenatally. [11, 12, 13, 14, 15, 16, 17, 18] Maternal serum alpha-fetoprotein levels are elevated in only 3% of patients, because most encephaloceles are covered with skin. Postnatally, infants may have associated cerebrospinal fluid (CSF) rhinorrhea and recurrent meningitis. [19]
The earliest reported ultrasonographic diagnosis was made at 13 weeks' gestation. Once an encephalocele is diagnosed, a thorough search for associated abnormalities should be performed. [20, 9]
Radiography
Cranial defects that are associated with encephaloceles usually occur in the midline of the skull and appear anywhere from the base of the nose to the base of the occipital bone. [20, 9, 21] The skull defect is smooth and well circumscribed, with no associated increased opacity at the margin of the bone defect.
Cranial defects occurring in association with encephaloceles (see the image below) have a nonspecific appearance. Moreover, plain radiographs rarely provide diagnostic information regarding the contents of an encephalocele. Epidermoid and dermoid cysts, craniolacunia, parietal foramina, frontal fenestrae, fibrous dysplasia, wide sutures, cranial dysostosis (including cleidocranial dysostosis), and hypophosphatasia can mimic encephalocele-related cranial defects.
 Skull radiograph in a 76-year-old woman presenting with headaches and a palpable depression in the region of the parietal bones on both sides of the skull. The radiograph shows a well-defined thinning of the parietal bone (arrow).
Skull radiograph in a 76-year-old woman presenting with headaches and a palpable depression in the region of the parietal bones on both sides of the skull. The radiograph shows a well-defined thinning of the parietal bone (arrow).
Computed Tomography
Although prenatal diagnosis of fetal encephalocele and its associated anomalies has been achieved by using computed tomography (CT) scans, the use of radiation for diagnosis in fetuses is discouraged, particularly in the first 2 trimesters.
Postnatally, CT scans provide an excellent depiction of the bony defect, particularly with coronal, sagittal, or 3-dimensional (3D) reconstruction. However, CT scanning is less capable than magnetic resonance imaging (MRI) in depicting soft-tissue components in an encephalocele. [5]
CT scans may be useful in the demonstration of associated intracranial anomalies, such as Chiari malformations, holoprosencephaly, Dandy-Walker complex, aqueduct stenosis, agenesis of the corpus callosum, and other midline abnormalities. MRI is considered superior to CT scanning in the analysis of these conditions.
(See the images below.)
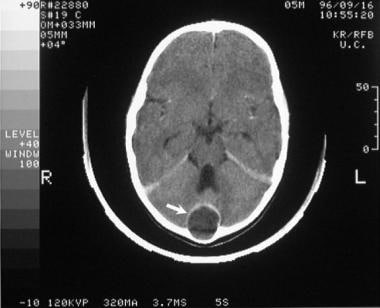 Axial, contrast-enhanced computed tomography (CT) scan through the basal cisterns in a 6-year-old child who presented with headaches and fever. Scan shows a rim-enhancing cystic mass eroding the inner skull table of the occiput (arrow). At surgery, an infected dermoid cyst was found.
Axial, contrast-enhanced computed tomography (CT) scan through the basal cisterns in a 6-year-old child who presented with headaches and fever. Scan shows a rim-enhancing cystic mass eroding the inner skull table of the occiput (arrow). At surgery, an infected dermoid cyst was found.
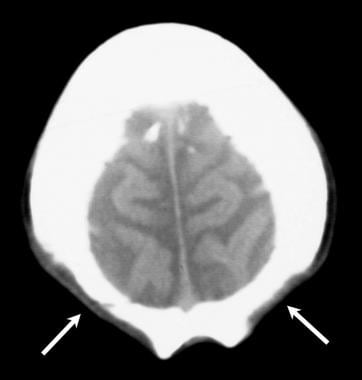 Transaxial, nonenhanced computed tomography (CT) scan through the vertex in a 76-year-old woman presenting with headaches and a palpable depression in the region of the parietal bones on both sides of the skull. The scan shows developmental, bilateral parietal foramina.
Transaxial, nonenhanced computed tomography (CT) scan through the vertex in a 76-year-old woman presenting with headaches and a palpable depression in the region of the parietal bones on both sides of the skull. The scan shows developmental, bilateral parietal foramina.
Water-soluble contrast material that is placed in the theca and that flows into the encephalocele may allow better evaluation of the contents. CT cisternography scanning often demonstrates a communication of the herniated sac with the intracranial subarachnoid space. Attenuation measurements may be used to differentiate brain tissue from CSF in the herniated sac.
Magnetic Resonance Imaging
Although US scanning has traditionally been the mainstay in fetal imaging, its resolution of the fine details of the brain and/or CNS is sometimes limited by the mother's body habitus, the surrounding amniotic fluid, and the position of the fetus. MRI may provide better detail in prenatal imaging. Fetal MRI requires fetal and maternal sedation, but it appears to be an effective means of noninvasively assessing fetal CNS anomalies. [17, 22, 23, 5]
The ability of MRI to resolve posterior fossa anatomy appears to be superior to that of US scanning. Moreover, fluid-filled and/or CSF-filled structures are demonstrated well on MRI scans.
Postnatally, MRI is the examination of choice for the evaluation of an encephalocele. With the ability to depict the brain in multiple projections, MRI scans can provide exquisite detail of the cranial defect and the herniated contents, as demonstrated in the images below. (Contents of the herniated sac may include CSF, disorganized brain tissue, and even ventricles.) Basal encephaloceles may be noted as masses protruding into the nasal cavity. They may mimic nasal polyps on CT and MRI scans. Because adenoids and nasal polyps are rare in infancy, the presence of a nasopharyngeal mass should alert the clinician to the possibility of a basal encephalocele.
MRI can also be useful in demonstrating associated intracranial anomalies, such as Chiari malformation, holoprosencephaly, Dandy-Walker complex, aqueduct stenosis, agenesis of the corpus callosum, and other midline abnormalities.
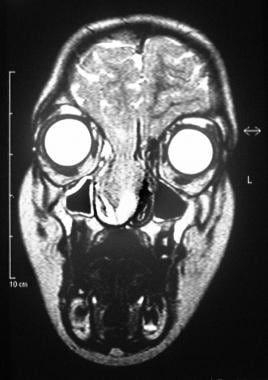 Coronal, T2-weighted magnetic resonance imaging (MRI) scan in a 7-year-old boy. The patient was examined by an ear, nose, and throat surgeon because of a nasal voice and a blocked nose. Images show a sphenoid encephalocele. Herniated brain tissue is seen in the right nostril through a sphenoid defect.
Coronal, T2-weighted magnetic resonance imaging (MRI) scan in a 7-year-old boy. The patient was examined by an ear, nose, and throat surgeon because of a nasal voice and a blocked nose. Images show a sphenoid encephalocele. Herniated brain tissue is seen in the right nostril through a sphenoid defect.
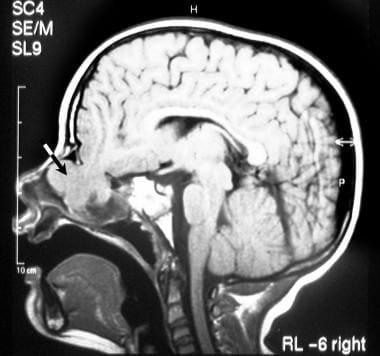 Sagittal, T1-weighted magnetic resonance imaging (MRI) scan through the midline (same patient as in the previous image) shows brain herniation through the sphenoid into the nasal cavity (arrow).
Sagittal, T1-weighted magnetic resonance imaging (MRI) scan through the midline (same patient as in the previous image) shows brain herniation through the sphenoid into the nasal cavity (arrow).
Ultrasonography
US scanning remains the modality of choice for detecting prenatal CNS anomalies. To diagnose an encephalocele with certainty, a skull defect must be demonstrated. This is possible in 80% of fetuses with an encephalocele. Finding the defect may be difficult because of its small size; also, artifacts caused by shadowing may be present, and these can mimic a skull defect. The prenatal ultrasound diagnosis of an encephalocele is based on the demonstration of a cranial defect with varying degrees of brain herniation. The US appearance of an encephalocele is variable in the first trimester. [24, 11, 12, 13, 14, 15, 16, 6]
The classic ultrasonographic appearance is that of a mass in the midline of the skull, with most cases occurring in the occipital and (less commonly) frontal regions. The size of the bony defect can vary from a few millimeters upward, and the extruded sac can be small or can be larger than the fetal skull itself. The mass may be purely cystic, or it can contain echoes from brain tissue.
(Ultrasonographic characteristics of encephaloceles are demonstrated in the images below.)
 Meckel-Gruber syndrome. Ultrasonograms show oligohydramnios-enlarged echogenic kidneys (left) and a fairly large occipital encephalocele containing brain tissue (right).
Meckel-Gruber syndrome. Ultrasonograms show oligohydramnios-enlarged echogenic kidneys (left) and a fairly large occipital encephalocele containing brain tissue (right).
 Sagittal ultrasonogram through the fetal skull shows a fairly large occipital encephalocele containing brain tissue.
Sagittal ultrasonogram through the fetal skull shows a fairly large occipital encephalocele containing brain tissue.
 Sagittal ultrasonogram through the fetal skull shows a fairly massive occipital encephalocele associated with Dandy-Walker syndrome.
Sagittal ultrasonogram through the fetal skull shows a fairly massive occipital encephalocele associated with Dandy-Walker syndrome.
 Encephalocele and cervical meningocele. Courtesy of Ravi Devidas Kadasne, MBBS, MD, Specialist in Radiology, Emirates International Hospital, UAE.
Encephalocele and cervical meningocele. Courtesy of Ravi Devidas Kadasne, MBBS, MD, Specialist in Radiology, Emirates International Hospital, UAE.
 Encephalocele and cervical meningocele. Courtesy of Ravi Devidas Kadasne, MBBS, MD, Specialist in Radiology, Emirates International Hospital, UAE.
Encephalocele and cervical meningocele. Courtesy of Ravi Devidas Kadasne, MBBS, MD, Specialist in Radiology, Emirates International Hospital, UAE.
Because skull ossification begins at 10 weeks' gestation, diagnosis is usually not possible before this time. The earliest reported diagnosis established by using a transvaginal scan was at 13 weeks' gestation. However, some have suggested that, starting at 9 weeks' gestation, the enlargement of the rhombencephalon cavity may indicate the presence of an encephalocele.
Most encephaloceles are covered with skin; therefore, they are more likely to be diagnosed with screening US scanning than with maternal serum alpha-fetoprotein testing.
The skull defect is identified in more than 80% of fetuses with an occipital encephalocele (75%). Associated findings may include a flattening of the basiocciput, an acute angle between the mass and skin line of the neck and occiput, ventriculomegaly, and a lemon sign (33%).
A cyst-within-a-cyst appearance is occasionally seen. This results from herniation of the fourth ventricle in the encephalocele surrounded by CSF.
A true frontal encephalocele is seen as an extrinsic mass near the dorsum of the nose, orbits, or forehead. Such encephaloceles are often associated with hypertelorism, midline craniofacial dysraphism, agenesis of the corpus callosum, interhemispheric lipoma, or heterotopias. [25]
Sphenoidal encephaloceles are usually clinically occult and appear in the first decade of life, when it is more appropriate to use CT scanning and/or MRI than it is to employ other modalities.
Frontal encephaloceles almost always contain brain tissue and involve the bridge of the nose (60%), as well as the nasal cavity (30%).
Parietal encephaloceles are associated with hydrocephalus, aqueduct stenosis, Arnold-Chiari malformation, microcephaly, and Dandy-Walker cysts.
US scanning may reveal a bony defect in the sphenoid bone that is associated with an overlying soft-tissue mass, but the mantle of the brain tissue in the encephalocele is often difficult to detect. In these cases, MRI is useful.
In one example of a fatal encephalocele, the encephalocele herniated through the clivus into the oropharynx. This appeared as a cystic mass that was surrounded by an echogenic rim protruding through the mouth. Ventriculomegaly and polyhydramnios were also noted. At delivery, airway intubation was not possible, and the baby did not survive.
Most parietal encephaloceles result from amniotic band syndrome, in which early disruption of skull development probably occurs. Encephaloceles that are secondary to amniotic bands are atypical, and their appearance is variable; moreover, they are usually not associated with other syndromes and/or genetic abnormalities.
Once an encephalocele is diagnosed, a search should be made for associated anomalies, such as Meckel-Gruber syndrome (which is characterized by an occipital encephalocele), microcephaly, cystic dysplastic kidneys, and polydactyly. [20, 9] Meckel-Gruber syndrome may be more easily diagnosed in the first trimester, when the amniotic fluid volume is usually normal. In the second trimester, oligohydramnios may hamper visualization of polydactyly and the encephalocele.
Walker-Warburg syndrome, which also is associated with encephaloceles, is a lethal complex of the CNS and eyes. [26] The diagnosis is established by the detection of lissencephaly, hydrocephalus, and a cerebellar malformation. Recognizing these syndromes is important because they are autosomal recessive conditions. Because they can be recognized on prenatal US scans, targeted screening may be possible in the mother's subsequent pregnancies.
Degree of confidence
Occipital encephaloceles can be confused with a cystic hygroma, which has no cranial vault defect and contains no brain tissue. [13] A high cervical meningocele also can mimic an encephalocele. A frontal encephalocele may be mistaken for a nasal teratoma; both conditions are rare, and the prognosis for each of them is poor.
The prenatal diagnosis of an epidermal scalp cyst simulating an encephalocele has been reported. [27] Mimics of a parietal encephalocele include an ultrasonographic refraction artifact at the skull edge and a cloverleaf skull in which the temporal bone may be partially absent. An intra-oral salivary gland cyst can mimic a basal encephalocele.
-
Meckel-Gruber syndrome. Ultrasonograms show oligohydramnios-enlarged echogenic kidneys (left) and a fairly large occipital encephalocele containing brain tissue (right).
-
Sagittal ultrasonogram through the fetal skull shows a small occipital encephalocele.
-
Sagittal ultrasonogram through the fetal skull shows a fairly large occipital encephalocele containing brain tissue.
-
Sagittal ultrasonogram through the fetal skull shows a fairly massive occipital encephalocele associated with Dandy-Walker syndrome.
-
Coronal, T2-weighted magnetic resonance imaging (MRI) scan in a 7-year-old boy. The patient was examined by an ear, nose, and throat surgeon because of a nasal voice and a blocked nose. Images show a sphenoid encephalocele. Herniated brain tissue is seen in the right nostril through a sphenoid defect.
-
Sagittal, T1-weighted magnetic resonance imaging (MRI) scan through the midline (same patient as in the previous image) shows brain herniation through the sphenoid into the nasal cavity (arrow).
-
Axial, contrast-enhanced computed tomography (CT) scan through the basal cisterns in a 6-year-old child who presented with headaches and fever. Scan shows a rim-enhancing cystic mass eroding the inner skull table of the occiput (arrow). At surgery, an infected dermoid cyst was found.
-
Skull radiograph in a 76-year-old woman presenting with headaches and a palpable depression in the region of the parietal bones on both sides of the skull. The radiograph shows a well-defined thinning of the parietal bone (arrow).
-
Transaxial, nonenhanced computed tomography (CT) scan through the vertex in a 76-year-old woman presenting with headaches and a palpable depression in the region of the parietal bones on both sides of the skull. The scan shows developmental, bilateral parietal foramina.
-
Encephalocele and cervical meningocele. Courtesy of Ravi Devidas Kadasne, MBBS, MD, Specialist in Radiology, Emirates International Hospital, UAE.
-
Encephalocele and cervical meningocele. Courtesy of Ravi Devidas Kadasne, MBBS, MD, Specialist in Radiology, Emirates International Hospital, UAE.
-
Encephalocele and cervical meningocele. Courtesy of Ravi Devidas Kadasne, MBBS, MD, Specialist in Radiology, Emirates International Hospital, UAE.





