Practice Essentials
Meralgia paresthetica (MP) is pain or an irritating sensation felt over the anterior or anterolateral aspect of the thigh due to injury, compression, or disease of the lateral femoral cutaneous nerve (LFCN) (see the image below). Early investigators of MP include Bernhardt, who first described the condition in 1878; Hagar, who attributed the pain to compression of the LFCN; and Roth, who coined the term meralgia paresthetica (thigh pain). [1]
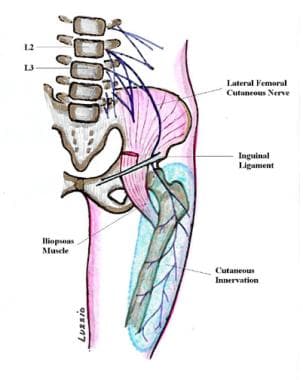 Basic anatomy of the lateral femoral cutaneous sensory nerve. The blue region over the anterolateral thigh outlines the area of cutaneous innervation.
Basic anatomy of the lateral femoral cutaneous sensory nerve. The blue region over the anterolateral thigh outlines the area of cutaneous innervation.
Diagnosis of MP is based on history and examination. Nerve conduction studies are used to verify the presence of the neuropathy and rule out other causes for the symptoms. Treatment for uncomplicated or benign forms of MP includes conservative measures initially, followed by surgical intervention for chronic discomfort. Malignant pathologic processes can produce symptoms of MP and must therefore be ruled out before conservative treatments are initiated.
Symptoms of meralgia paresthetica
A patient whose MP is idiopathic or is caused by mechanical injury near the inguinal ligament (IL) may describe paresthesias or dysesthesias within the cutaneous distribution of the LFCN.
Isolated lesions of the LFCN result only in abnormalities on sensory examination. Reduced perception of pinprick or dysesthesia within the receptive fields of the LFCN is typical.
Workup in meralgia paresthetica
Indicated laboratory and radiologic studies for LFCN pathology depend on the suspected etiology and clinical impression. MP caused by obvious benign compressive forces requires no further investigation; however, the following scenarios may necessitate more testing:
-
Magnetic resonance imaging (MRI) to investigate the lumbar plexus
-
Serum tests for diabetes
-
Radiography for possible pelvic fracture or cancer
-
Computed tomography (CT) scanning for retroperitoneal hemorrhage in patients who have undergone anticoagulation therapy
Electromyography is very helpful for ruling out radiculopathy, plexopathy, generalized polyneuropathy, or other neuropathic causes for symptoms.
Management of meralgia paresthetica
MP is treated with conservative therapy, such as physical therapy, weight reduction to reduce abdominal girth, heat application, and analgesics. Patients should avoid wearing constrictive garments, belts, or braces that impart excessive focal pressure at the IL. [2]
Patients failing conservative measures are referred to a surgeon for consideration of surgical decompression of the LFCN. [3, 4, 5, 6, 7, 8]
Pathophysiology
The lateral femoral cutaneous nerve (LFCN) is formed by the fusion of the posterior branches of the second and third lumbar nerves. This purely sensory nerve traverses the retroperitoneum around the lateral circumference of the ileum to the inguinal ligament (IL). Just medial to the anterosuperior iliac spine (ASIS), the LFCN passes underneath the IL and enters the anterior thigh beneath its fascia (see the image below). Ordinarily, a few centimeters distal to the IL, the LFCN divides into anterior and posterior branches. Tributaries of these branches perforate thigh fascia and receive sensory information from portions of the associated dermatomes L2-L3. Typically, this area encompasses the anterior lateral thigh from just below the hip to above the knee. Variations in the anatomy of the LFCN, such as splitting by the inguinal ligament, are hypothesized to predispose it to neuropathic processes. [9, 10, 11]
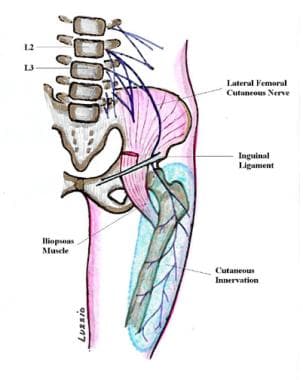 Basic anatomy of the lateral femoral cutaneous sensory nerve. The blue region over the anterolateral thigh outlines the area of cutaneous innervation.
Basic anatomy of the lateral femoral cutaneous sensory nerve. The blue region over the anterolateral thigh outlines the area of cutaneous innervation.
A study by Moritz et al found the LFCN to be closer to the ASIS in patients with idiopathic MP than it was in controls. Using high-resolution ultrasonography, the investigators determined that among the study’s 28 patients with MP, the mean distance of the LFCN from the ASIS was 0.52 cm, compared with 1.79 cm in the 15 controls. [12]
Nerve entrapment can occur at 3 potential sites, including (1) beside the spinal column, (2) within the abdominal cavity as the nerve courses along the pelvis, and (3) as the nerve exits the pelvis. The last site is the most common; there, nerve entrapment may involve the sartorius muscle, or it may be caused by simple compression superficially near the iliac crest and ASIS by tight clothing or trauma.
The angulation of the LFCN across the iliac crest results in varying compressive forces with postural repositioning. One opinion is that fibrous bands within the fascia subject the LFCN to deleterious tensile forces. The relatively superficial trajectory of the LFCN as it enters the thigh compartment makes it extremely prone to injury due to compression against underlying bone.
The LFCN is subject to systemic processes that can detrimentally affect any peripheral nerve. Diabetes mellitus, for example, can result in diffuse or focal neuropathies, especially in nerves, such as the LFCN, that are subject to excessive compressive forces.
Movement of the hip changes angulation and tension of the nerve, which can affect symptoms. For example, hip extension may increase angulation and tension on the LFCN, and flexion can decrease these forces.
A Brazilian study involving 14 patients with meralgia paresthetica (MP) and 14 control subjects found evidence that not only are the large myelinated nerve fibers of the LFCN affected in MP, but the small fibers may be as well, with the small fibers suffering a partial loss of function and causing painful symptoms. [13] The investigators suggested that this is particularly true in individuals who have had MP for a longer period of time.
Epidemiology
Frequency
United States
Considered uncommon but not rare, meralgia paresthetica (MP) is probably underrecognized. Notably, 3 cases are reported per 10,000 general clinic patients. Also, it occurs in an estimated 7-35% of patients referred for leg discomfort. Up to 20% of patients with MP have bilateral symptoms.
Mortality/Morbidity
Isolated meralgia paresthetica (MP) secondary to compression or injury of the nerve unrelated to major trauma or to systemic or malignant processes is not associated with mortality or significant morbidity.
Sex
Meralgia paresthetica is more common in males than in females.
Age
Meralgia paresthetica is observed in all age groups, but the condition most commonly occurs in middle-aged adults.
-
Basic anatomy of the lateral femoral cutaneous sensory nerve. The blue region over the anterolateral thigh outlines the area of cutaneous innervation.








