Background
Female genital cosmetic surgery (FGCS) is a growing field of plastic surgery that involves a variety of procedures designed to enhance or rejuvenate the female genitalia. This branch of cosmetic surgery includes monsplasty, vaginoplasty, hymenoplasty, labiaplasty, G-spot augmentation, clitoral hood reduction and/or lift, frenuloplasty, perineoplasty, fat injections, and combinations of these procedures. [1, 2, 3, 4]
 Severe labia minora hypertrophy. The labia minora extends 4 cm beyond the labia majora, which can cause pain with clothing and exercise.
Severe labia minora hypertrophy. The labia minora extends 4 cm beyond the labia majora, which can cause pain with clothing and exercise.
A study carried out in 2015 by Oranges et al assessed labia minora excision techniques and identified eight labiaplasty techniques: edge resection, wedge resection, deepithelialization, W-plasty, laser labiaplasty, custom flask, fenestration, and composite reduction. Good outcomes resulted from all of these procedures, with findings of high patient satisfaction and low morbidity. [5]
There are several reasons why a patient may desire FGCS, including functional and aesthetic concerns. [6] Severe labia minora hypertrophy may cause pain when wearing underwear, riding a bicycle, exercising, or having sexual intercourse. [1] Patients have reported insecurities about appearance with a sexual partner or while wearing tight-fitting clothing, such as bathing suits. [7] In the same manner that children report being teased about physical features, numerous slang terms are associated with excess labial tissue; these are often psychologically damaging and increase social anxiety. Other common concerns are related to hygiene or infection.
In addition, there is a belief that trends in pubic hair grooming have led to increased visibility of and greater focus on the labia, while images of female genitalia have increased in the media and on the Internet, including video or photographic pornography.
 Labia hypertrophy, anterior view. (Left) Heavy labia majora and a prominent clitoral hood, but no excess minora showing. (Right) Labia minora hypertrophy, with minimal majora showing.
Labia hypertrophy, anterior view. (Left) Heavy labia majora and a prominent clitoral hood, but no excess minora showing. (Right) Labia minora hypertrophy, with minimal majora showing.
According to a 2000 study of 163 labia minora reductions, 87% of patients had labiaplasty surgery for aesthetic reasons, while 64% desired surgery because of discomfort in everyday clothing. [8] In the same study, 85% had bilateral labiaplasty, compared with 15% who had asymmetrical hypertrophy of the labia minora requiring a unilateral procedure. [8]
Labia minora reductions are more common than labia majora reductions or augmentations, although both are a growing field in plastic surgery. [2, 9] The goal of these procedures is to eliminate functional problems and to create labia that are aesthetically appealing. Labiaplasty surgeries can have substantial psychological benefits for patients who are self-conscious about the appearance of their genitalia. Patients with severe cases of labial hypertrophy frequently report decreased pain or discomfort with daily activity and sexual intercourse after the procedure.
History of the Procedure
Hypertrophy, or overgrowth, of the labia was historically viewed as an inconsequential variation of the normal labia. Over time, however, there has been increasing acknowledgement and understanding of the aesthetic and functional concerns of patients with large labia. [10]
The first description of aesthetic labiaplasty was published in 1983. [11] At that time, the only technique used to reduce the labia minora was the “trim method.” [12] In the 1990s, alternative labiaplasty techniques were developed, [12, 13] including the “wedge technique” described by Dr. Gary Alter in 1998. [12] Labiaplasty has been growing in popularity over the past several years. According to statistics from the American Society for Aesthetic Plastic Surgery (ASAPS), a 23% increase in labiaplasty was reported from 2015 to 2016 among ASAPS members. [14]
This underscores the progressive social acceptance of the procedure, as well as the need for safe and effective labiaplasty techniques. Current techniques for labiaplasty can be divided into the following:
-
Amputation techniques that involve a linear trimming of the labia minora
-
A wedge technique that excises tissue along the lower edge towards the labia majora crease
-
A central labial excision as a deepithelialization that preserves the natural free edge
Relevant Anatomy
The nerve sensation to the external genitalia arises from the pudendal nerve. The nerve traverses and subsequently splits at the superficial transverse perineal muscle into the superficial and deep perineal nerves. The superficial branch progresses to become the posterior labial nerve, and the deep branch becomes the dorsal nerve of the clitoris.
The anatomy of the clitoral hood has received a somewhat variable description in the literature. Anatomists refer to this as being the free edge of the prepuce. Many aesthetic surgeons, however, consider the clitoral hood to incorporate the skin superior to the free edge, extending to the anterior labial commissure and laterally including the prepuce. The frenulum inferiorly extends upwards to the clitoris and inferolaterally to the labia minora. This is an important landmark to mark out and identify, as clitoral hood deformity can result if it is not addressed adequately. The extent of the hood is variable in patients and will be determined by the overall size of the clitoris itself, the thickness being dependent on the underlying subcutaneous tissue.
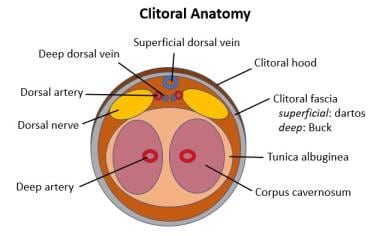
Diagrams of vulvar and clitoral anatomy are shown below.
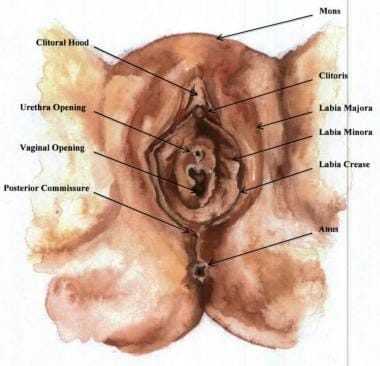 Anatomical diagram of the vulva. The typical external female genitalia include the labia majora, labia minora, clitoris, clitoral hood, mons pubis, labial commissure, urethra opening, and vaginal opening. Collectively, the external female genitalia are referred to as the vulva. Female genital plastic surgery can be performed on the labia minora, labia majora, mons pubis, vagina, and clitoral hood. The labia minora are 2 mucocutaneous folds that lie between the labia majora and surround the opening to the vagina and urethra. The labial folds extend from the rectum to the mons pubis. The labia minora extend anterior to the clitoral hood.
Anatomical diagram of the vulva. The typical external female genitalia include the labia majora, labia minora, clitoris, clitoral hood, mons pubis, labial commissure, urethra opening, and vaginal opening. Collectively, the external female genitalia are referred to as the vulva. Female genital plastic surgery can be performed on the labia minora, labia majora, mons pubis, vagina, and clitoral hood. The labia minora are 2 mucocutaneous folds that lie between the labia majora and surround the opening to the vagina and urethra. The labial folds extend from the rectum to the mons pubis. The labia minora extend anterior to the clitoral hood.
Problem
Labial hypertrophy is the increased growth of either the labia minora in relation to the labia majora or vice versa. Although labial hypertrophy is not yet strictly defined as a pathologic condition, patients who have aesthetic or functional concerns may benefit from labial reductions. [8] A key consideration is determination of the nature of the patient's concerns. Is the concern related to the patient's own wish or that of a partner? How long has this been a concern for the patient?
Significant hypertrophy of the labia can cause pain, irritation, and discomfort with clothing. Moreover, the psychological problem of not feeling “normal” in comparison with the perceived anatomic ideal must not be underestimated. [2] It is quite important to ensure that the patient understands that although she may not feel normal, her anatomy is normal. Specifically, while the labia may be enlarged or asymmetrical, this does not make it abnormal, as there many variations in labial anatomy.
Epidemiology
Frequency
Labiaplasty surgeries are expected to continue rising in frequency as the techniques and procedures become more defined. Popularity of the procedure is also expected to grow as knowledge of the benefits increase. As previously stated, statistics from the ASAPS revealed a 23% increase in labiaplasty from 2015 to 2016 among the society's members. [14]
It is also proposed that increases in hair removal or changing hair patterns have affected the frequency of labiaplasty surgeries. [2, 9] A 2009 study analyzing the media’s influence on FGCS showed that 84% of younger women remove pubic hair, compared with only 36% of older women. Of all women who removed pubic hair, only 50% were happy with the appearance of their labia. [15]
Etiology
The exact cause of hypertrophy of the labia minora is unknown, but a multifactorial etiology is purposed. [16] Genetic factors and hormones can lead to hypertrophy of the labia early in life, while mechanical irritation from bicycling, sexual intercourse, genital piercing, horseback riding, and other factors can cause hypertrophy in later years. [16] Infection is also associated with the condition.
Pregnancy and weight gain can increase the fat accumulation and ptosis of female genitalia, predominantly the labia majora. [1] Therefore, after childbirth or significant weight loss, a patient may desire to have the wrinkled appearance or increased size of her labia addressed. Also during pregnancy, pressure can increase and a feeling of heaviness ensue as a result of increased blood flow to the genital region. [17] On the other hand, a significant association between labial hypertrophy and multiparity has not been shown. [5]
In addition, weight loss and changes in the appearance of the labia majora can accentuate the size of the labia minora.
Pathophysiology
The medical community has not defined a singular grading system for hypertrophy of the labia. Past surgeons have defined hypertrophy of the labia minora as ranging from 3-5 cm. [10, 8, 7] In 1983, hypertrophy was defined as 5 cm, while in current practice, labia minora longer than 3-4 cm are considered hypertrophic. [9]
In 2013, Chang et al suggested the following simplified classification system to measure labial hypertrophy [7] :
-
Class 1 - Equal minora and majora
-
Class 2 - Minora extending beyond the majora
-
Class 3 - Hypertrophy involving the clitoral hood
-
Class 4 - Hypertrophy of the minora extending to the perineum
The following grading system, by Davison and West, to objectively measure labia minora hypertrophy has been used clinically [18] :
-
None - The labia minora extends no farther than the labia majora
-
Mild/moderate - The labia minora extends 1-4 cm beyond the labia major (see the image below)
-
Severe - The labia minora extends more than 4 cm beyond the labia majora
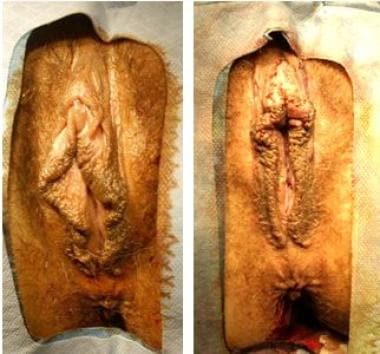 Moderate labia hypertrophy. A moderate labia hypertrophy before resection (left) and intraoperative results after resection (right).
Moderate labia hypertrophy. A moderate labia hypertrophy before resection (left) and intraoperative results after resection (right).
Banwell classified labia minora morphologically as follows, "according to the distance from the most lateral prominence of the labium minus to the vaginal introitus" [19, 20] :
-
Type 1 - Upper third prominence
-
Type 2 - Middle third prominence
-
Type 3 - Lower third prominence
According to the Motakef classification, labial protrusions are placed into class 1 (0 - 2 cm), class 2 (2-4 cm), or class 3 (>4 cm). [19, 20]
Presentation
There are several thoughts and opinions as to why the request for genital cosmetic surgery has seen a huge upward trend. Initially, many indicators pointed towards a desire for a standardized appearance that is essentially prepubescent and is sometimes referred to as the “Barbie" look. This gives the appearance of the vaginal opening being quite tight and the labia minora narrow. [21] In the author's practice, this has been far from the truth. The majority of patients that are consulted have felt that this was something that bothered them throughout puberty, with the problem having more to do with excess skin and less of the tucked-in look that the majority prefer. Almost every patient asks for a "normal-looking" labia. This is something very important to discuss. The author spends a considerable amount of time showing before and after pictures and highlighting the fact that there is no true “normal” labial appearance but that there is instead a great amount of variation.
The idea that genital appearance is culturally dependent and affected by the development of Internet pornography is also considered to be linked to patient requests for surgery. However, not one patient that the author has seen has wanted a labial procedure due to what the individual had viewed online. Nonetheless, in some cases, when the patient's partner has mentioned appearance, the comment is likely associated with perceptions that the partner formed from seeing pornographic images.
Indications
The primary indicators for labiaplasty are as follows:
-
Hypertrophy of the labia minora with aesthetic or functional impairment
-
Labial asymmetry
Patients who report functional and/or aesthetic concerns about hypertrophic labia may be considered candidates for surgery. However, individuals who focus on pain or sexual inadequacy as reasons for the procedure may need more preoperative assessment, including a psychological evaluation, prior to undergoing labiaplasty. For example, many patients have discomfort during intercourse due to the labial lips being caught, but other possible causes of dyspareunia need to be investigated as well. Moreover, concerns over sexual inadequacy may not be improved through surgery.
Patients who experience pain while exercising, especially with repeated trauma, may also be good candidates for the operation (see image below). The grading systems described in Pathophysiology should be used as a guide but not as an absolute indication for surgical candidacy.
Contraindications
Absolute contraindications
There are no absolute contraindications to labiaplasty. Any patient who is in good health and has symptomatic or aesthetic concerns should be properly evaluated. If the consulting surgeon believes that a surgical intervention can alleviate the symptom or improve the appearance, then an operation is reasonable.
Not all physicians consider young age to be a contraindication for labia minora reduction. Some patients have been operated on during adolescence or even before (age 10 years). [9, 22, 23] The author disagrees with surgery in these cases, however, because in many patients the labia can continue to develop beyond puberty into early adulthood. The author's own preference is to defer surgery until a minimum age of 18 years. This will ensure that the patient has completed development and can give consent for the procedure herself.
Surgery on a pregnant patient should also ideally be deferred, and patients should be educated with regard to the way in which the labial area will change during pregnancy. The labia can enlarge due to pregnancy-related hormones, and they can darken, stretch, and even tear during delivery. Therefore, it is more reasonable to suggest surgery following completion of the family.
Although menstruation is not a direct contraindication, surgery may be avoided while the patient is menstruating. The local anesthetic is generally more uncomfortable, and patients find the experience far more distressing, during this time. However, the author has carried out surgery in patients who have been menstruating and found no issues with wound dehiscence, wound infection, or heightened pain during the procedure.
It is important to distinguish elective female genital surgery, such as labiaplasty, from genital mutilation. Female genital mutilation (FGM) is practiced in a variety of cultures and involves young women and girls who have procedures performed on the vulva against their will. Whether or not a person agrees with the performance of labiaplasty is of the greatest importance in determining if a patient is seeking out and consenting to the procedure of her own volition. Surgery is never performed at the request or under the duress of an individual other than the patient.
The World Health Organization (WHO) highlights these facts regarding FGM [24] :
-
In FGM, the external female genitalia is partially or totally removed or other injury is visited upon the female genital organs, for nonmedical reasons
-
No health benefits are derived for girls or women from FGM
-
FGM can cause severe bleeding and problems with urination, along with cysts, infections, and complications in childbirth, with increased risk for newborn deaths
-
More than 200 million girls and women alive today have undergone FGM in 30 countries in Africa, the Middle East, and Asia, where the practice is concentrated
-
Girls between infancy and age 15 years are the most frequent targets of FGM
-
FGM represents a human rights violation
-
WHO opposes FGM in all of its forms and opposes performance of FGM by healthcare providers (medicalization of FGM)
-
In 27 high-prevalence countries, the cost of treating the health complications of FGM comes to $1.4 billion (USD) annually
Relative contraindications
Minimal relative contraindications to labiaplasty exist. Patients with gynecologic disease are not good candidates for the surgery. As with most operations, patients who smoke increase their risk for poor healing, particularly raising the chance of wound dehiscence. [8] Other factors that contribute to increased risk of wound dehiscence, such as collagen disorders, should be considered when planning for labiaplasty.
Patients need to be counseled with regard to body dysmorphia disorder (BDD), and most importantly, a patient must have realistic expectations prior to surgery and be advised appropriately. There is a general consensus that BDD should be considered a contraindication to cosmetic treatments. Clinicians should use a multidisciplinary approach in the management of patients seeking labiaplasty, including cooperation among specialists in psychiatry, cosmetic surgery, family practice, and other specialties. This will ensure the best outcome for the patient.
Patient Education
Patient education is one of the most important aspects of the surgical consultation. The author routinely gives out before-care and aftercare instructions to the patient, which highlight the procedure itself, as well as risks and complications and frequently asked questions. The information below is based on the author's personal information pack.
Why do patients request this procedure?
The vaginal opening is flanked by the labia majora (the outer labia) and the labia minora (the inner labia). In some individuals, the labia minora may hang down, or "stick out"; this can become bothersome during exercise or when using cosmetics or may lead to an increased frequency of infections and to issues with sexual intercourse. A labiaplasty helps to correct these issues by surgically reducing the labia minora so that they do not hang below the labia majora. This operation may be performed under local anesthesia, under local anesthetic with oral sedation, or with general anesthesia, while the minora are artistically trimmed and sutured.
The author’s own practice primarily involves local anesthetic cases; he routinely performs labiaplasties alone or in combination with labia majora and clitoral hood reduction, with no detriment to patients' outcomes or results.
Am I an ideal candidate for a labiaplasty?
The ideal candidate for a labiaplasty is a female older than age 18 years with excess labia minora who seeks minora reduction due to physical or emotional complaints. The patient needs to be fully informed and of sound judgment prior to proceeding with this operation.
Frequently asked questions
These include the following:
- Will I have a scar? Any time an incision is placed, a scar will form. The incisions normally heal very well and are hidden. The scar will initially appear red and raised, but as it progresses through scar maturation, it will eventually become pale. This process takes around 6-9 months. The surgical technique used will also determine how visible the scar will be.
- Is the surgery painful? This is a difficult question to answer. Pain symptoms are related to the area of surgery and also to the patient's own ability to address the pain. Some patients have a very high pain tolerance and do not find the surgery very uncomfortable. Others find the surgery quite painful. Painkillers should be given following the surgery and are advised for a minimum of 48 hours regularly postoperatively. Thereafter, continuation of painkillers depends on the patient's tolerance for pain.
- Will sutures need to be removed after surgery? Most surgeons use absorbable stitches. These will usually dissolve over the course of 1 week. Sutures usually do not need to be removed after the surgery.
- When can I resume intercourse/sexual activity? It is best to avoid sexual activity (intercourse/masturbation) for at least 4 weeks. This will give the area time to heal. Any aggressive manipulation/stimulation during this time can result in wounds breaking down and can possibly lead to infection.
- How long will I be swollen? Swelling will persist for 2 weeks or longer. This is because the region of surgery is such that the swelling is working against gravity.
- How long will I be out of work? Individuals can normally return to work in 1-2 weeks. This depends on the type of work that the individual performs. Most desk-related jobs are easier to return to.
- How long before I can exercise? The author suggests avoiding strenuous exercise for the first 2 weeks, with no heavy lifting or bending. However, the author does suggest walking around; otherwise, there is a tendency not to move, and in the author's experience, the majority of patients who have had a difficult postoperative recovery have been those who did very little in the immediate postoperative period. Regular, short walks around the house are suggested. This will help to reduce the swelling and consequently decrease pain in the area. Following this, very light exercise can be performed from 2-4 weeks. After 4 weeks, patients can resume physical and sexual activity. By 6 weeks, most patients are back to their normal routine.
- When can I shower? The author asks patients to shower the next day. There are various regimens given; the author prefers that patients wash the surgical area but without the soap directly contacting the incision line. Cleaning the area reduces the chance of infection. It also removes the dried blood and generally helps patients to feel more comfortable. However, there most be no submersion in a bath or swimming for a minimum of 2 weeks, to allow the superficial wound to heal.
- When can I drive a car? This depends on a number of factors. If patients are taking strong painkillers, then it is suggested that they avoid driving until they have stopped the medication. Patients also need to be able to perform an emergency stop. This may be quite difficult during the first week following surgery. The author also highlights to patients that although they may feel well enough to drive, their car insurance may be nullified if they drive on the day of surgery, and so they should check to see what their insurance policy states.
- Can I become pregnant afterwards? This surgery will not affect the ability to become pregnant.
- How long does the operation take? This varies from patient to patient. However, the operation normally takes 1 hour to complete, although this depends on whether the procedure is combined with labia majora and/or clitoral hood reduction.
- Does someone have to stay with me after surgery? The author always advises that patients have someone with them following the surgery to help them get home and also to have someone stay with them. Most patients tolerate the operation without any problems, but due to the location of the surgery, individuals can be quite uncomfortable and therefore may require help with everyday activities for the first week.
-
Severe labia minora hypertrophy. The labia minora extends 4 cm beyond the labia majora, which can cause pain with clothing and exercise.
-
Moderate labia hypertrophy. A moderate labia hypertrophy before resection (left) and intraoperative results after resection (right).
-
Labia hypertrophy, anterior view. (Left) Heavy labia majora and a prominent clitoral hood, but no excess minora showing. (Right) Labia minora hypertrophy, with minimal majora showing.
-
Increased labia majora due to ptosis, which can interfere with daily activities such as exercise and increase insecurities when wearing tight clothing.
-
Anatomical diagram of the vulva. The typical external female genitalia include the labia majora, labia minora, clitoris, clitoral hood, mons pubis, labial commissure, urethra opening, and vaginal opening. Collectively, the external female genitalia are referred to as the vulva. Female genital plastic surgery can be performed on the labia minora, labia majora, mons pubis, vagina, and clitoral hood. The labia minora are 2 mucocutaneous folds that lie between the labia majora and surround the opening to the vagina and urethra. The labial folds extend from the rectum to the mons pubis. The labia minora extend anterior to the clitoral hood.
-
This unilateral hypertrophy of the left labia minora can be addressed with the labiaplasty amputation technique.
-
Diagram of amputation technique.
-
Wedge excision results. Before (left) and 3 months after (right) a wedge excision labiaplasty for moderate labia hypertrophy, allowing for preservation of the natural edge.
-
Central wedge technique.
-
Anterior wedge technique with labial crease extension.
-
Anterior wedge technique. (Left) The dog ear is extended into the labial crease. (Center) The labia is approximated centrally. (Right) The dog ear is closed anteriorly.
-
Posterior wedge technique.
-
Deepithelialization technique.
-
Central deepithelialization technique. The patterns drawn out on the mucosa and skin sides of the labia illustrate the central deepithelialization technique. The tristar excision as a deepithelialization maximizes nerve and vascular supply to the edge while minimizing dog-ears.
-
Clitoral unhooding Y-to-V technique.
-
Labia majora reduction technique with ellipse wedge.
-
Labiaplasty results. Before (left) and 1 year after (right) a successful labiaplasty with wedge technique, labia majora reduction, clitoral unhooding, and posterior fornix release. If desired by the patient, the amputation technique can be used on the left labia minora to enhance the results and create color symmetry.
-
Smoking predisposes patients to dehiscence. This labia minora reduction patient (left) was a smoker. She smoked during the 2 preoperative and postoperative weeks, causing dehiscence to the left labial crease (center). The dehiscence had no long-term complications on the result (right).
-
A transverse section through the clitoral body. The cross section is similar to that of the penis.
-
Labiaplasty resection markings.