Overview
Background
In an acute resuscitation situation, after the airway is secured and adequate breathing and gas exchange are established, the next priority is to obtain vascular access. This is often difficult in infants and children. The physiologic processes of shock and hypothermia with resulting vascular constriction, which are often present in a resuscitative situation, may further complicate the problem; furthermore, the skill and experience levels of providers in caring for small children widely vary.
Intraosseous (IO) access has been used therapeutically since 1934 and has been proved to be a safe, reliable, and rapid means of introducing crystalloids, colloids, medications, and blood products into the systemic circulation. [1, 2, 3, 4, 5, 6, 7, 8, 9] The marrow cavity provides access to a noncollapsible venous plexus as blood flows from the medullary venous sinusoids into the central venous sinus and is then drained into the central venous circulation via nutrient and emissary veins.
With the development of the intravenous (IV) catheter, the IO needle fell into disuse. In the 1980s, however, IO access was rediscovered as an immediately available tool in resuscitation situations, when time is of the essence and conditions may be adverse. [10, 11] Since then, IO access has become widely accepted in pediatric settings, especially because these patients often provide a particular challenge to obtaining rapid intravascular access.
A retrospective study by Carlson et al found that in 2011, among out-of-hospital critical procedures provided for pediatric patients by emergency medical services in the United States, IO access was one of the most common. Using the National Emergency Medical Services Information System’s national data set, the investigators found that there were 865,591 emergency medical responses that year involving children. Of 616,913 procedures performed (on 246,016 pediatric cases), 11,026 were critical procedures, the most frequently administered being intubation (3599 procedures, or 6.7 per 1000 pediatric cases) and IO access (2618 procedures, or 5 per 1000 pediatric cases). [12]
Indications
Initiation of IO access is indicated in adults, children, infants, or newborns in any clinical situation where vascular access is emergently needed but not immediately available via a peripheral vein. IO access provides a means of administering medications, glucose, and fluids, as well as (potentially) a means of obtaining blood samples. Such a situation would include any resuscitation; cardiopulmonary arrest; shock, regardless of etiology; life-threatening status epilepticus; or lack of venous access resulting from burns, edema, or obesity.
In comparison with child and infant peripheral IV access, central lines, or umbilical lines, IO access is safer, is associated with fewer complications, can be implemented with less delay, and requires less skill and practice on the part of practitioners who may use the techniques only rarely. [13]
IO needle placement does not constitute definitive therapy; rather, it allows the administration of life-saving medications and fluids in a context where intravascular access is vital. Often, definitive IV access is easier to obtain once a bolus of fluids and medications has been administered via the IO needle.
IO needles may be left in place in the marrow for up to 72-96 hours; presumably, the longer the needle remains in place, the greater the risk of infection and dislodgment. In practice, the needle is usually removed as soon as another means of vascular access (either peripheral or central) is available, ideally within 6-12 hours.
Contraindications
Contraindications to IO access include the following:
-
Ipsilateral fracture of the extremity, because of resulting extravasation and risk of compartment syndrome
-
Previous placement or attempted placement in the same leg or site (eg, sternum), because of consequent extravasation into soft tissue compartments through the previous puncture site
-
Osteogenesis imperfecta, because of the likelihood that puncture of the bone may cause a fracture
-
Osteopetrosis, because of the risk of fracture
-
Obvious overlying infection at the proposed puncture site, because of the risk of seeding infection (a relative contraindication)
Periprocedural Care
Preprocedural Planning
Intraosseous (IO) access was initially thought to be less applicable in patients older than 6 years. However, historical and current data (eg, in military populations [14] ), as well as guidelines from the American Heart Association [15] and the American College of Critical Care Medicine, [16, 17] support the consideration of IO techniques in patients of any age as rapid and equally effective alternatives to intravenous (IV) peripheral lines.
Moreover, IO access is considered more appropriate than attempted placement of central lines in situations when immediate resuscitation is essential. [18, 19] In addition, IO needles provide rapid access to the central circulation, with good bioequivalence to IV infusion. [20, 21]
The particular site used (see Technique) varies as appropriate for the age of the patient, the anatomic landmarks present, and the bone density. It should be noted that the blood chemistry, drug levels, hemoglobin concentrations, blood typing, and acid-base status [22] of the blood in the marrow aspirates obtained from the IO needle have been found to be reliable predictors of the corresponding serum values (although this may not be true of blood chemistry and acid-base status in the setting of prolonged resuscitation).
Over the past decade, attitudes regarding the different settings in which IO access might be considered have changed and broadened. IO access is now part of the recommendations for emergent intravascular access in patients of all ages, not just in pediatric and neonatal patients. In addition, the literature includes reports regarding IO access use for local anesthesia and other nonemergent applications in adults, as well as case reports of nonemergent use in specific pediatric situations. [23]
Clearly, the use of IO access in a battlefield setting remains applicable; this venous route continues to be accessible even in the most hypovolemic patient, and military and trauma literature attest to its usefulness in that setting.
The optimal duration of IO access is still the subject of controversy. On an intuitive basis, it would seem that long-term use of IO access should increase the risk of potential infection, but the infection and complication rates are actually very low, even in the most exigent circumstances. No data support the common informal recommendation that another access avenue must be obtained before transfer from the emergency department or that the IO needle should be removed as soon as possible.
Equipment
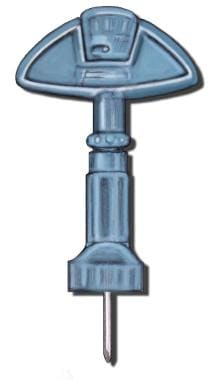
Several needle types are available (see the images below). The traditional needles are inserted manually, but powered needle insertion devices are becoming more popular.
Technique
Intraosseous Needle Insertion Methods
With the exception of neonatal settings or neonatal intensive care unit (NICU) settings, in which spinal needles are occasionally used, the intraosseous (IO) needle should have a needle stylet to reduce the likelihood of bony spicules or a clot clogging the needle. In addition, the IO needle should have some means for the operator to gauge the distance to which the needle has penetrated, either with markings on the shaft or a covering flange that prevents insertion deeper than a predetermined distance.
Once the bony cortex has been penetrated, the needle usually need not be advanced more than 1 cm to provide stability and access to the marrow cavity.
The various types of IO needles currently available in pediatric emergency department (ED) and hospital settings are placed by means of different insertion methods.
The traditional needles (Cook, Jamshidi) are placed manually; the site, force required, and depth of insertion are determined by the operator.
However, powered insertion devices are used with increasing frequency in pediatric patients in US hospitals—in emergency departments (EDs), critical care units (CCUs), and even operating rooms (ORs). [23] Since 2006, 2 devices have been approved by the US Food and Drug Administration (FDA) for use in adult and pediatric patients: the Bone Injection Gun (BIG) device (Waismed) and the EZ IO (Vidacare).
The BIG device, which is more widely used outside of the United States, has a spring-loaded handle that injects the IO needle to a preset depth, determined by the patient's age. In the United States, the EZ IO is now widely used in field and transport settings (eg, emergency medical service situations). It has a battery-powered drill handle that powers the needle insertion; the length of the needle is determined by the patient's weight in kilograms, and the depth of insertion is determined by the operator (as with the manual devices).
Both the BIG device and the EZ IO are approved for use at the following sites:
-
Proximal and distal tibia (in both pediatric and adult populations)
-
Humeral head (in adult populations)
Neither device requires special removal equipment. Training videos are available on the respective Web sites (Vidacare and Waismed).
A retrospective review from Minnesota that compared the use of a manual IO access device with the use of the EZ IO in an emergency medical services (EMS) setting found that substituting an EZ IO for a manual device did not improve the first-attempt success rate or the success-per-attempt rate, but it more than tripled the rate at which IO access was used by EMS providers. [24]
The F.A.S.T.1 system (Pyng Medical Corporation) for sternal IO needle placement in adults includes both a marker patch and a special introducer device to simplify needle placement and the depth of needle insertion. In addition, this system uses a flexible infusion tube rather than a rigid stylet after needle removal to minimize displacement. It requires the use of a removal device, which is included with the kit.
Intraosseous Needle Insertion Sites
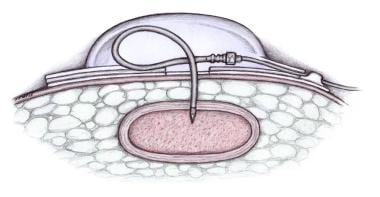
The sternum is the original site of IO access (see the image below) and is a useful site to consider in adult patients, as is the ilium. Studies suggest that IO infusion may be effective even in bones that do not contain a medullary cavity, such as the calcaneus and the radial styloid. [25, 26]
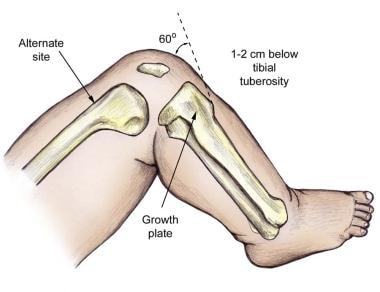
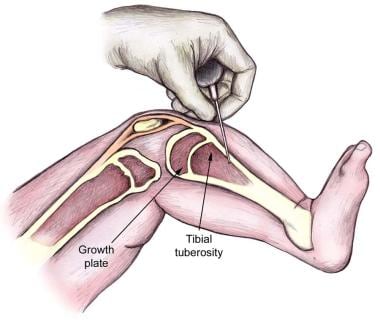
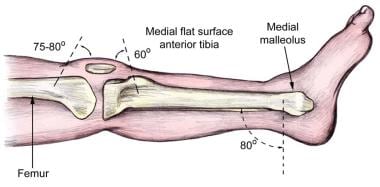
The insertion site of choice in children and infants is the proximal tibia; the distal tibia and distal femur are alternatives (see the images below). The proximal tibia provides a flat wide surface and has only a thin layer of overlying tissue, which allows easy identification of landmarks. Additionally, the proximal tibia is distant from the airway and chest, where cardiopulmonary resuscitation (CPR) is often in progress.
The anterolateral proximal humerus is another site that is often used in adults. As powered devices become more widely available and IO access becomes more commonly used in the prehospital setting and in adults, this site will become increasingly relevant.
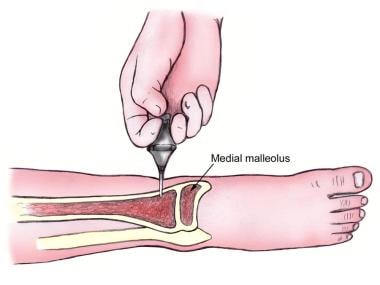
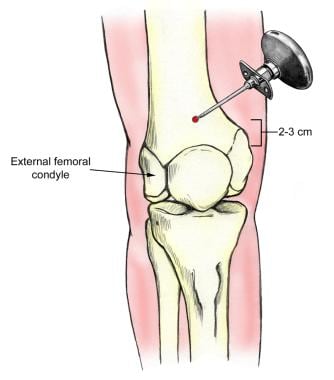
With increasing age, the cortical thickness of long bones, particularly the tibia, increases, making penetration more difficult and forceful; thus, in older children and adults, using the distal tibia or the proximal humerus may be advantageous because it also provides reliable and evident landmarks, has a relatively thin cortex, and is distant from ongoing CPR (see the images below).
The distal femur (see the image below) may also be used for IO access, but it generally has much denser covering layers of fat, muscle, and soft tissue, which make identification of landmarks and bony penetration more difficult.
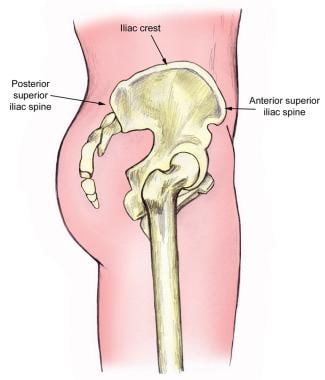
In adults, other insertion sites have included several different iliac sites (see the image below), the sternum, the distal radius or ulna, and, as mentioned above, the humerus.
Complications of Intraosseous Needle Placement
Complications of intraosseous (IO) needle placement are rare, especially if the correct techniques are followed and frequent subsequent evaluations of the needle's position within the bone are carried out. [27] In a review that examined the use of IO catheters in trauma resuscitation, Tyler et al found that the insertion success rate was 95% and the incidence of complications was 0.9%. [28]
Failure to achieve effective IO placement may be the result of 1 or more of the following:
-
Incorrect identification of landmarks
-
A bent needle, which is more common with longer needles or spinal needles
-
Clogging of the needle with marrow, clot, or bone spicules, which can be avoided by frequent flushing of the needle or by continuous infusion
-
Through-and-through penetration of both anterior and posterior cortices caused by excess force after the needle has penetrated the cortex, which renders the punctures useless because of fluid extravasation and which may cause a compartment syndrome
-
Subcutaneous or subperiosteal infiltration, caused by incomplete placement of needle or by a dislodged needle
-
Fractures caused by excess force or by fragile bones (eg, marked osteoporosis or osteopenia, osteopetrosis, or osteogenesis imperfecta), which allows leakage, extravasation, and potential compartment syndrome to occur
-
Penetration of the mediastinal structures or space with the potential for pneumothorax, vascular injury, lung injury, in the case of a sternal needle
Complications even after effective placement and timely removal are rare but may include the following:
-
Local infection (cellulitis and osteomyelitis are quite rare) - The incidence was less than 0.6% in a literature review of 4000 cases over 35 years (though it was found that the rate may increase with prolonged placement) and less than 3% in another large review
-
Compartment syndrome secondary to fluid extravasation
-
Local hematoma
-
Pain
-
Potential for growth plate injuries (though this has not been reported in animals or humans [29] )
-
Fat embolus - This is rarely reported in adult patients and has not been reported when an IO needle is placed in the tibia rather than in other sites, such as the ilium or sternum
-
Bone embolus (though this has not been reported in humans)
-
Mediastinitis after sternal IO puncture
-
Intraosseous needle insertion sites in infant or small child.
-
Intraosseous needle insertion sites in older child, adolescent, or adult.
-
Alternative intraosseous needle insertion site: ilium.
-
Sternal needle: F.A.S.T.1 system (Pyng Medical Corporation).
-
Cook-type intraosseous needle.
-
Cook-type screw-tip intraosseous needle (Sur-Fast needle).
-
Jamshidi intraosseous needle.
-
Illinois sternal iliac intraosseous needle.
-
Shown are 3 different sizes of intraosseous needles for use in EZ IO (Vidacare). Appropriate size is determined by patient weight and size.
-
Bone Injection Gun (BIG) spring-loaded intraosseous insertion device (Waismed).
-
Proximal tibia intraosseous needle insertion site.
-
Distal tibia intraosseous needle insertion site.
-
Distal femur intraosseous needle insertion site.
-
Sternal intraosseous needle insertion.