Background
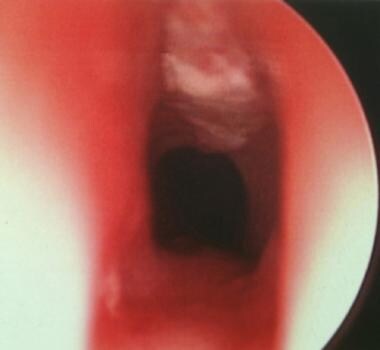
Subglottic stenosis (SGS) is a narrowing of the subglottic airway (see the image below). The subglottis is defined as the airway directly below the level of the vocal folds and encased in the cricoid cartilage. The subglottic airway is the narrowest area of the airway because it is encased in a complete, nonexpandable, and nonpliable ring. In contrast, the trachea has a posterior membranous section, and the larynx has a posterior muscular section.
The term SGS implies a narrowing of the subglottic airway that is either congenital or acquired in etiology, though the term is applied to both congenital lesions of the cricoid ring and acquired SGS.
Acquired SGS is the most common acquired anomaly of the larynx in children and the most common abnormality requiring tracheotomy in children younger than 1 year. Correction of this abnormality requires expanding the lumen of the cricoid area to increase airflow and decrease obstructive breathing. Surgical correction of SGS has been performed with various techniques over the years.
Early in the 20th century, acquired SGS was usually related to trauma or infection from syphilis, tuberculosis, typhoid fever, or diphtheria. Often, the treatment itself for SGS at this time, a tracheostomy, led to further damage to the airway
The incidence of acquired SGS increased in the late 1960s through the 1970s, after McDonald and Stocks introduced long-term intubation as a treatment method for neonates in need of prolonged ventilation. [1] The increased incidence of SGS focused new attention on the pediatric larynx, as well as the need for development of novel treatment modalities.
Pathophysiology
The exact pathophysiology of congenital SGS is unknown, though there is a known association of SGS with syndromes such as Down syndrome.
Acquired SGS, on the other hand, is most freqently associated with intubation or airway trauma. Mechanical trauma from an endotracheal tube, as it passes through or remains for long periods in the narrowed neonatal and subglottic airway, can lead to mucosal edema and hyperemia. These conditions then can progress to pressure necrosis of the mucosa. These changes have been observed within a few hours of intubation and may progress to expose the perichondrium of the cricoid cartilage. Infection of the perichondrium can result in a subglottic scar.
This series of events can be hastened if an oversized endotracheal tube is used. Always check for an air leak after placing an endotracheal tube because of the risk of necrosis of the mucosa, even in short surgical procedures. Usually, the pressure of the air leak should be less than 20 cm H2O, so that no additional pressure necrosis occurs in the mucosa of the subglottis.
Etiology
The exact etiology of congenital SGS is unknown.
The etiology of acquired SGS is related to trauma of the subglottic mucosa. Injury can be caused by infection or mechanical trauma, usually from endotracheal intubation but also from blunt, penetrating, or other trauma. Historically, acquired SGS has been related to infections such as tuberculosis and diphtheria. Over the past 40 years, the condition has typically been related to mechanical trauma.
Factors implicated in the development of SGS include the size of the endotracheal tube relative to the child's larynx, the duration of intubation, the motion of the tube, and repeated intubations. Additional factors that affect wound healing include systemic illness, malnutrition, anemia, and hypoxia. [2]
Local bacterial infection may play an important role in the development of SGS. Gastroesophageal reflux (GER) may play an adjuvant role in the development of SGS because it causes the subglottis to be continually bathed in acid, which irritates and inflames the area and prevents it from correctly healing. A systemic or gastrointestinal (GI) allergy may cause the airway to be more reactive, creating a greater chance of developing stenosis.
Epidemiology
United States statistics
No known frequency has been reported for congenital SGS; the incidence of acquired SGS has greatly decreased over the past 40 years. In the late 1960s, when endotracheal intubation and long-term ventilation for premature infants began, the incidence of acquired SGS was as high as 24% in patients who required such care. In the 1970s and 1980s, estimates of the incidence of SGS were 1-8%.
In 2000, Choi reported that the incidence of SGS had remained constant at the Children's National Medical Center in Washington DC, accounting for approximately 1-2% of the children who had graduated from the neonatal intensive care unit (NICU). [3]
Walner reported that of 504 neonates who were admitted to the level III NICU at the University of Chicago in 1997, 281 were intubated for an average of 11 days; over a 3-year period, no patients developed SGS. [4]
International statistics
International frequency is the same as that of the United States.
In 1996, a report from France also described no incidence of SGS in the neonatal population who were intubated with very small endotracheal tubes (2.5 mm internal diameter) in attempts to prevent trauma to the airway.
Age-, sex-, and race-related demographics
SGS is observed more often in premature infants because they may require mechanical ventilation for other system or pulmonary problems secondary to their prematurity. The mechanical ventilation can result in airway trauma and, potentially, SGS.
Equal sex distribution is noted. No racial predilection is noted.
Prognosis
The symptoms and prognosis of SGS can be highly variable, mostly depending on the severity of the SGS. Difficulty in breathing and exercise intolerance can occur with mild, moderate, or severe SGS. In moderate-to-severe cases of SGS, respiratory insufficiency can lead to failure to thrive, acute life threatening events (ALTE), and even death.
The outcome of laryngotracheal reconstruction depends on its grade and the procedure performed. Most authors report success rates of 80-90% when the patient has undergone successful preoperative evaluation and when the appropriate operation has been performed (see the images below).
 A 3-month postoperative subglottic view of the patient with congenital and acquired vertical subglottic stenosis, who underwent anterior and posterior costal cartilage grafting with successful decannulation showing open subglottis with some very mild damage to the anterior wall and the suprastomal area where the tracheostomy tube had been placed.
A 3-month postoperative subglottic view of the patient with congenital and acquired vertical subglottic stenosis, who underwent anterior and posterior costal cartilage grafting with successful decannulation showing open subglottis with some very mild damage to the anterior wall and the suprastomal area where the tracheostomy tube had been placed.
 A 1-week postoperative subglottic view of the surgical repair with an anterior graft of a congential elliptical subglottic stenosis. The white areas to the left and right are the true vocal cords. The graft is seen at the superior and mid area.
A 1-week postoperative subglottic view of the surgical repair with an anterior graft of a congential elliptical subglottic stenosis. The white areas to the left and right are the true vocal cords. The graft is seen at the superior and mid area.
The presence of acute or chronic respiratory illness, GER, or a reactive larynx may decrease the success rate. Choi and Zalzal showed that age can affect success rates; scars are more likely to recur in children younger than 2 years than in others. [5] Success is more likely with localized SGS than with extensive SGS. [6]
Zalzal noted that in any child with voice abnormalities before surgery, those abnormalities persisted after surgery. [7] Subglottic pressure is required to produce a strong voice. If the narrowed subglottic airway is expanded, subglottic airflow and pressure increase, and the voice usually is stronger (see the images below). Voice therapy may help relieve nonsevere glottic stenosis over time.
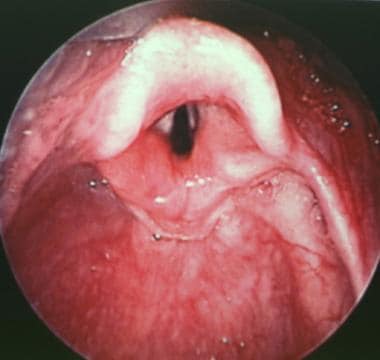
 Preoperative view of glottic stenosis and small glottic chink in a 2-year-old child who underwent anterior and posterior grafting. The child's glottic narrowing is tight, and scarring of the right arytenoid has occurred.
Preoperative view of glottic stenosis and small glottic chink in a 2-year-old child who underwent anterior and posterior grafting. The child's glottic narrowing is tight, and scarring of the right arytenoid has occurred.
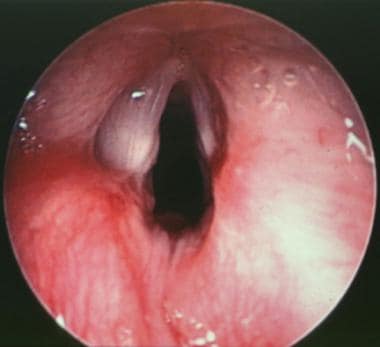
 Preoperative endoscopic subglottic view of a 2-year-old patient with congenital and acquired vertical subglottic stenosis.
Preoperative endoscopic subglottic view of a 2-year-old patient with congenital and acquired vertical subglottic stenosis.
 Postoperative view of the glottic larynx in a child who underwent anterior and posterior grafting for subglottic stenosis. The child had glottic narrowing that is more open and in neutral position after the surgery. The scarring of the right true vocal cord appears improved, and her voice is more normal.
Postoperative view of the glottic larynx in a child who underwent anterior and posterior grafting for subglottic stenosis. The child had glottic narrowing that is more open and in neutral position after the surgery. The scarring of the right true vocal cord appears improved, and her voice is more normal.
 Postoperative close-up view of the true vocal cords in the patient with congenital and acquired vertical subglottic stenosis.
Postoperative close-up view of the true vocal cords in the patient with congenital and acquired vertical subglottic stenosis.
 A 3-month postoperative subglottic view of the patient with congenital and acquired vertical subglottic stenosis, who underwent anterior and posterior costal cartilage grafting with successful decannulation showing open subglottis with some very mild damage to the anterior wall and the suprastomal area where the tracheostomy tube had been placed.
A 3-month postoperative subglottic view of the patient with congenital and acquired vertical subglottic stenosis, who underwent anterior and posterior costal cartilage grafting with successful decannulation showing open subglottis with some very mild damage to the anterior wall and the suprastomal area where the tracheostomy tube had been placed.
The voice of a patient with SGS, especially those who require reconstruction, may never return to its preoperative state, because the following are possible:
-
Glottic stenosis
-
Imperfect closure of a laryngofissure through the anterior commissure
-
Potential vocal cord weakness or tension caused by other laryngeal pathologic conditions
Because reconstructive techniques have improved over the past few decades, the focus of attention in patients with SGS who require reconstruction has switched from decannulation to decannulation with improved voice outcome.
Avelino et al reported a 100% success rate with balloon laryngoplasty in children with acute subglottic stenosis, though they found the procedure to be less successful in chronic subglottic stenosis. [8] Factors that predicted a good outcome were as follows:
-
Acute stenosis
-
Less severe grades of stenosis
-
Younger patient age
-
Absence of tracheotomy
Patient Education
Teaching parents life-saving maneuvers for a child with a tracheotomy or airway stent following laryngotracheal reconstruction is critical. It is also important to teach parents cardiopulmonary resuscitation (CPR) before their child leaves the hospital.
For further information, see Subglottic Stenosis in Children. For patient education resources, see Bronchoscopy.
-
Intraoperative endoscopic view of a normal subglottis.
-
A glottic and subglottic view of a grade III subglottic stenosis in an 18-year-old patient following a motor vehicle accident. The true vocal cords are seen in the foreground. Subglottic stenosis is seen in the center of the picture.
-
Endoscopic view of the true vocal cords in the foreground and the elliptical congenital subglottic stenosis (SGS) in the center of the picture.
-
Endoscopic subglottic view of congenital elliptical subglottic stenosis, a close-up of subglottic stenosis.
-
An intraoperative view of a split cricoid in a patient with elliptical congenital subglottic stenosis. The open airway can be seen in the center of the picture. The wound extends to the inferior one third of the thyroid cartilage. The first 2 tracheal rings also are divided.
-
Rib graft for reconstruction of subglottic stenosis carved in boat type anterior graft. The diamond-shaped internal intraluminal component with perichondrium still present is seen on the top section of the rib and the shape of the rib is seen on the backside of the carved out diamond shape.
-
An intraoperative aerial view of an anterior cartilage graft in place over the wound. Note external component of the graft still looks like a portion of the rib. The internal component has been carved in a diamond shape. This is an intraoperative photo of the patient with elliptical congenital subglottic stenosis. The cartilage graft (rib graft for reconstruction of subglottic stenosis carved in boat type anterior graft) was used in this patient for reconstruction.
-
An intraoperative side view of the neck with cartilage graft (rib graft for reconstruction of subglottic stenosis carved in boat type anterior graft) to be placed into the posterior cricoid suspended and having all sutures in position, ready to be tied. All the sutures are placed prior to lowering the graft into position. Then, the sutures are tied.
-
A 1-week postoperative subglottic view of the surgical repair with an anterior graft of a congential elliptical subglottic stenosis. The white areas to the left and right are the true vocal cords. The graft is seen at the superior and mid area.
-
Subglottic view of very mild congenital subglottic stenosis. Laterally, the area looks only slightly narrow. When endotracheal tubes were used to determine its size, it was found to be 30% narrowed.
-
An intraoperative view of granular subglottic stenosis in a 3-month-old infant who was born premature, weighing 800 g. The area is still granular following cricoid split. This patient required tracheotomy and eventual reconstruction at age 3 years. True vocal cords are shown in the foreground (slightly blurry).
-
Intraoperative laryngeal view of the true vocal cords of a 9-year-old boy. Under the vocal cords, a spiraling subglottic stenosis can be seen.
-
A close-up view of the stenosis in a 9-year-old boy with spiraling subglottic stenosis. This spiraling subglottic stenosis is not complete circumferentially. Laser therapy was the treatment choice and was successful after 2 laser treatments.
-
Continued lasering of the subglottic stenosis in a 9-year-old boy with spiraling subglottic stenosis. The reflected red light is the aiming beam for the CO2 laser.
-
Endoscopic view of the same patient (9-year-old boy with spiraling subglottic stenosis) two months after surgery. Some mild residual posterior subglottic stenosis remains, but the child is asymptomatic and the airway is open overall.
-
Preoperative view of a 4-month-old infant with acquired grade III subglottic stenosis from intubation. Vocal cords are in the foreground.
-
An endoscopic subglottic view of a 4-month-old with grade III subglottic stenosis born premature at 26 weeks' gestation and intubated for 3 months.
-
Postoperative view in a 4-month-old infant with acquired grade III subglottic stenosis from intubation. Following cricoid split, the patient had been intubated for 1 week and extubated for 1 week.
-
A subglottic view of the same patient (a 4-month-old infant with acquired grade III subglottic stenosis from intubation) following dilation with an endotracheal tube to lyse the thin web of scar and a short course (5-day) treatment with oral steroids.
-
Postoperative view of the same patient (a 4-month-old infant with subglottic stenosis following cricoid split). This picture is 2 weeks after lysis of scar and steroids. Notice very mild recurrence of scaring at the site of previous scar. Overall, the airway is open and patent. The anterior superior area can be seen, with a small area of fibrosis where the cricoid split previously healed.
-
Anterior rib graft with a diamond shape. Note it measures approximately 1.7 mm in length. Intraluminal site is facing up. Flanges of rib are carved to remain on the outside of the trachea to prevent prolapse into the trachea.
-
Representative (noninclusive) sample of varying sizes of Aboulker stents (range of 3-15 mm). These stents are hollow and coated in Teflon.
-
A glottic endoscopic view of the top of Aboulker stent in the larynx protruding through and above the true and false vocal cords. The arytenoids and epiglottic folds are seen.
-
Diagram of a long Aboulker stent wired to a metal Jackson tracheotomy tube.
-
A Jackson tracheotomy tube wired to a long Aboulker stent.
-
A 7-mm Montgomery tracheotomy tube with caps
-
A subglottic endoscopic view of granulation tissue (superior center portion of the picture) that occurred at the graft site 10 days following a laryngotracheal reconstruction performed with an anterior graft. Granulation tissue is at the superior center portion of the picture.
-
Intraoperative suspended view through a subglottoscope of the subglottis, showing the granulation tissue just prior to removal with cup forceps and laser. This was taken in a patient who developed granulation tissue that occurred at the graft site 10 days following a laryngotracheal reconstruction performed with an anterior graft.
-
Postexcision view of granulation tissue through the subglottoscope. This was taken in a patient who developed granulation tissue that occurred at the graft site 10 days following a laryngotracheal reconstruction performed with an anterior graft.
-
Preoperative view of glottic stenosis and small glottic chink in a 2-year-old child who underwent anterior and posterior grafting. The child's glottic narrowing is tight, and scarring of the right arytenoid has occurred.
-
Preoperative endoscopic subglottic view of a 2-year-old patient with congenital and acquired vertical subglottic stenosis.
-
Postoperative view of the glottic larynx in a child who underwent anterior and posterior grafting for subglottic stenosis. The child had glottic narrowing that is more open and in neutral position after the surgery. The scarring of the right true vocal cord appears improved, and her voice is more normal.
-
Postoperative close-up view of the true vocal cords in the patient with congenital and acquired vertical subglottic stenosis.
-
A 3-month postoperative subglottic view of the patient with congenital and acquired vertical subglottic stenosis, who underwent anterior and posterior costal cartilage grafting with successful decannulation showing open subglottis with some very mild damage to the anterior wall and the suprastomal area where the tracheostomy tube had been placed.
-
End view of an Aboulker stent showing the central opening. These stents are hollow and coated in Teflon.
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Treatment
- Approach Considerations
- Medical Care
- Endoscopic Procedures
- Options for Open Reconstruction
- Anterior Cricoid Split
- Single-Stage Laryngotracheoplasty With Cartilage Expansion
- Multistage Procedure With Anterior and Posterior Grafting
- Partial Cricotracheal Resection
- Complications
- Prevention
- Consultations
- Long-Term Monitoring
- Show All
- Medication
- Media Gallery
- References







