Background
Trematodes of the Paragonimus genus cause paragonimiasis, a parasitic disease that strikes carnivores, causing a subacute to chronic inflammatory disease of the lung. Of the 10 or more Paragonimus species that are human pathogens, only 8 cause significant infections in humans.
The first case described in humans was at autopsy in Taiwan in 1879, when adult flukes were found in the lung. [1] The most common is the Oriental lung fluke, Paragonimus westermani. The adult trematode is reddish-brown and ovoid. Adults have 2 muscular suckers, an oral sucker situated anteriorly and a ventral sucker at mid body on the ventral surface. The eggs, golden brown and asymmetrically ovoid, have a thick shell with an operculum.
See the image below.
 This micrograph depicts an egg from the trematode parasite Paragonimus westermani. Eggs range in size from 68-118 µm x 39-67 µm. They are yellow-brown and ovoidal or elongated, with a thick shell. They are often asymmetrical, with one end slightly flattened. At the large end, the operculum (ie, lid or covering) is visible. Photo courtesy of The Centers for Disease Control and Prevention.
This micrograph depicts an egg from the trematode parasite Paragonimus westermani. Eggs range in size from 68-118 µm x 39-67 µm. They are yellow-brown and ovoidal or elongated, with a thick shell. They are often asymmetrical, with one end slightly flattened. At the large end, the operculum (ie, lid or covering) is visible. Photo courtesy of The Centers for Disease Control and Prevention.
Pathophysiology
The life cycle of these flukes involves 2 intermediate hosts plus humans. Its complex life cycle involves 7 distinct phases: egg, miracidium, sporocyst, redia, cercaria, metacercaria, and adult. Adult flukes live in human lungs and deposit eggs into the bronchi. Eggs are expelled either by coughing or by being swallowed and passed in human feces. Eggs then develop in water for 2-3 weeks and ultimately release miracidia, which invade the first intermediate host (ie, a specific species of fresh water snail). These miracidia develop through sporocyst and rediae stages into cercariae. The cercariae emerge and invade the second intermediate host (ie, a crustacean such as crabs or crayfish), in which they become metacercariae.
See the image below.
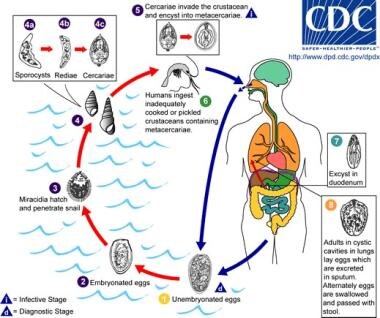 This is an illustration of the life cycle of Paragonimus westermani, one of the causal agents of paragonimiasis. Photo courtesy of The Centers for Disease Control and Prevention.
This is an illustration of the life cycle of Paragonimus westermani, one of the causal agents of paragonimiasis. Photo courtesy of The Centers for Disease Control and Prevention.
When humans ingest raw infected crustaceans, larval flukes develop in the small intestine and penetrate the intestinal wall into the peritoneal cavity 30 minutes to 48 hours after excysting. They then migrate into the abdominal wall or liver, where they undergo further development. Approximately 1 week later, adult flukes reenter from the abdominal cavity and penetrate the diaphragm to reach the pleural space and lungs. The eggs may then be expectorated or swallowed. If these eggs reach a water source, the life cycle will start over again. [2] Flukes mature, a fibrous cyst wall develops around them, and then egg deposition starts 5-6 weeks after infection. Lung flukes may live 20 years or more. In Japan, transmission has also occurred following human ingestion of raw pork from wild pigs that contained the juvenile stages of Paragonimus species.
Etiology
Factors that facilitate the life cycle of the flukes and subsequent transmission of infection to humans include the following:
-
Large numbers of reservoir and intermediate hosts
-
Behaviors such as spitting
-
Culinary habits
In Asia, raw and undercooked crab or crayfish are popular foods. In Korea and Japan, raw crayfish are used to treat measles, diarrhea, and skin conditions. Some tribes in Africa eat raw crustaceans to cure infertility. Peruvians eat raw crab with vegetables and lemon juice. Paragonimiasis may also be acquired by consuming raw meat from a paratenic host that contains young flukes (eg, wild boar as "sashimi"). Raw crawfish is also popular in the Mississippi Basin. [3] Infection may also be transmitted via contaminated kitchen utensils (eg, cutting boards, knives) or from cloths used to squeeze and strain juices from crabs for the preparation of soup.
Epidemiology
Frequency
United States
Generally, small numbers of cases have occurred in immigrants from endemic areas; however, the first case of paragonimiasis was reported in the United States in 1986 in a nonimmigrant adult. It is an important infection to consider in Southeast Asians who have settled in various areas of the United States. [4, 5]
International
Paragonimus species are endemic to Southeast Asia, Latin America (most commonly in Peru), and Africa (most commonly in Nigeria). Paragonimiasis is less commonly found in West Africa and Central and South America. [2] An estimated 22 million people are infected worldwide. Prevalence of infection in endemic areas ranges from 0.1-23.75%.
Race
Paragonimiasis is most common in Asians, Africans, and Hispanics.
Sex
Prevalence of infection is higher among females. An increase in infection in men, most notably those who are middle aged, because of their traditional culinary habits, has been observed in Japan.
Age
Prevalence reportedly increases with age and peaks in older adolescents and young adults; prevalence then declines progressively with age. By the sixth decade of life, prevalence is less than 25% of its peak in young adulthood.
Prognosis
The prognosis is good, with therapeutic cure rates of 90-100%. Symptoms resolve rapidly, and eggs disappear from the sputum in a few weeks following treatment. (Pulmonary paragonimiasis may be self-limited, with lesions resolving in 5-10 years in light infections.)
Death may occur during the acute phase of infection. For those who survive the acute phase, spontaneous recovery usually occurs within 1-2 months, but symptoms may recur intermittently over several years. Complications of untreated heavy infection include interstitial pneumonia, bronchitis, and bronchiectasis. Secondary complications may include bronchopneumonia, lung abscess, pleural effusion, or empyema. Untreated cerebral paragonimiasis has a mortality rate of approximately 5%. Cerebral infections may be associated with persistent seizures.
Resolution of abnormalities on chest radiographs may take several months, depending on the chronicity of the disease.
Patient Education
Safe food preparation and consumption must be emphasized.
-
This micrograph depicts an egg from the trematode parasite Paragonimus westermani. Eggs range in size from 68-118 µm x 39-67 µm. They are yellow-brown and ovoidal or elongated, with a thick shell. They are often asymmetrical, with one end slightly flattened. At the large end, the operculum (ie, lid or covering) is visible. Photo courtesy of The Centers for Disease Control and Prevention.
-
This is an illustration of the life cycle of Paragonimus westermani, one of the causal agents of paragonimiasis. Photo courtesy of The Centers for Disease Control and Prevention.




