Background
Mitral regurgitation (MR) (also known as mitral valve insufficiency) occurs when the mitral valve allows reversal of blood flow from the left ventricle (LV) to the left atrium. [1]
The presentation of mitral regurgitation varies and largely depends on its etiology, severity, and rate of onset. In acute severe mitral regurgitation, patients may present in heart failure or cardiogenic shock. In chronic mitral regurgitation, depending on the degree of regurgitation, patients may be asymptomatic and may remain so for many years. As the volume of regurgitation increases, the LV also increases in size. Progressive LV dilatation eventually leads to impaired contraction, increased afterload, reduced cardiac output, and, finally, left heart failure.
Major factors in management of mitral regurgitation include determining when to start therapy and what type of intervention is needed. Prognosis in patients with mitral regurgitation varies with the timing of the presentation and the severity of the associated congenital defects.
Embryology and Anatomy
Formation of the atrioventricular valve is completed early in embryologic development. The mitral valve is formed both from endocardial cushions that originate at the atrioventricular orifice and from muscular tissue of the ventricular wall. This process creates the four major components of the mitral valve, which are the mitral annulus, the mitral leaflets, the chordae tendineae, and the papillary muscles. [2]
The mitral annulus is derived from the fibrous skeleton of the heart, which is discontinuous posteriorly, thus increasing risk for posterior annular dilatation. The mitral valve leaflets (anterior and posterior) consist of collagenous fibrosa and spongiosa peripherally and mucoid myxomatous tissue centrally. The anterior leaflet is one third of the mitral valve and attaches to the mitral annulus, whereas the posterior leaflet attaches to the posterior lateral free wall of the left ventricle (LV). The chordae tendineae are a complex network of collagenous cordlike structures that extend from the free edges of the mitral valve leaflets to the papillary muscles. There are two papillary muscles; both arise from the ventricular free wall. Hence, ventricular geometry can affect the function of the papillary muscles. [3]
These four anatomic components function to allow unobstructed blood flow from the left atrium to the LV during diastole and to maintain competent closure during ventricular systole. The leaflets open fully during the early rapid-filling phase of diastole. They begin to close passively as LV pressure and volume increase. Then, the leaflets reopen briefly as atrial contraction occurs, adding additional volume to the LV. During atrial contraction, annular contraction begins, effectively decreasing the circumference of the mitral valve by 20%-30% throughout systole. Contraction of the papillary muscles serves to maintain the length of the chordae under the pressure that develops during systole. In the event that one or more of the four components is rendered nonfunctional or developmentally abnormal, mitral regurgitation (mitral valve insufficiency) results.
Pathophysiology
Although the pathophysiology resulting from mitral regurgitation (MR) (mitral valve insufficiency) is similar throughout all age groups, the specific cause of mitral regurgitation differs with age.
Normal blood flow from the left atrium to the left ventricle (LV) and, subsequently, to the systemic circulation, is altered in mitral regurgitation. In the presence of mitral regurgitation, as the blood flows antegrade from the LV into the aorta, and the regurgitant volume flows retrograde from the LV into the left atrium, this causes a proportionate increase in LV ejection volume. The regurgitant fraction reenters the LV, producing LV volume overload. The LV compensates via the Frank-Starling mechanism, resulting in a greater ventricular stroke volume. The volume of the regurgitant fraction depends on several factors, including the size of the orifice allowing regurgitation and the pressure gradient between the LV and left atrium. This volume also depends on the ventricular systolic pressure; therefore, the regurgitant volume increases in situations that increase afterload, such as hypertension or aortic stenosis.
The natural history and time course of mitral regurgitation varies, but mitral regurgitation can develop in three distinct stages (ie, acute, chronic compensated, chronic decompensated) that are clinically significant. The stages depend on acuity of onset, regurgitant volume, and compliance of the left atrium.
Acute mitral regurgitation stage
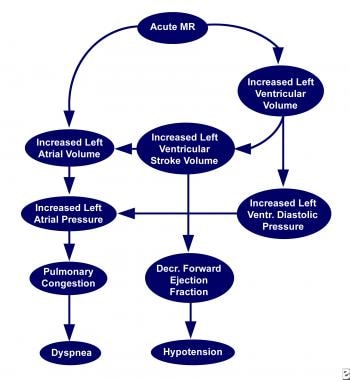
Acute mitral regurgitation causes sudden volume overload of the left atrium and LV. Initially, the undilated left atrium restricts the regurgitant volume at the expense of increase in both left atrial and LV end-diastolic pressures.
Although total ventricular stroke volume increases compared to normal, total forward stroke volume usually decreases, thereby lowering cardiac output. In the acute situation, rapidly increasing left atrial pressure results in elevated pulmonary venous pressure causing pulmonary congestion and, eventually, pulmonary edema (see the image below).
Chronic compensated stage
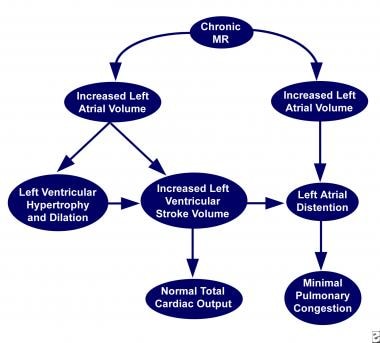
In the chronic compensated stage, the LV compensates by allowing greater diastolic filling and developing LV enlargement to augment forward stroke volume. More importantly, the left atrium dilates in response to the increased volume. Compensation for the increased volume can occur without resulting in increased pressure in the pulmonary circulation and the right heart. Left atrial compliance decreases the afterload on the LV, whereas LV dilatation and hypertrophy increases contractility. These important changes keep the overall afterload on the left heart normal or unchanged. Although the regurgitant fraction may be high, the larger stroke volume compensates, maintaining a nearly normal forward cardiac output (see the image below).
Chronic decompensated stage
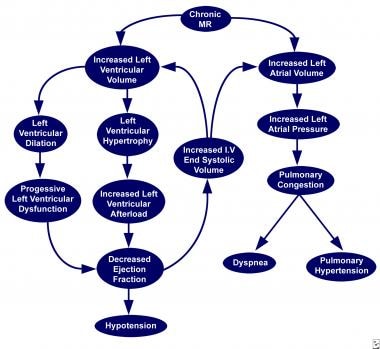
The chronic decompensated stage occurs when the LV is unable to sustain adequate forward cardiac output. As LV contractility begins to decrease, end-systolic volume gradually increases, thereby increasing LV end-diastolic pressure. The resulting increased pressure in the left atrium creates increased afterload, which further impairs LV ejection, thereby creating a repeating cycle. Whereas the end-diastolic and end-systolic volumes increase, pulmonary congestion eventually results if the cause of the mitral regurgitation is left untreated. Although the forward LV ejection fraction is reduced compared to the compensated phase, the overall ejection fraction could remain normal because of a large regurgitant flow.
As the degree of mitral regurgitation worsens, the total ejection fraction falls, indicating increasing ventricular dysfunction. Pulmonary hypertension may develop under long-standing increased pulmonary venous pressure, and, ultimately, it can lead to right heart failure (see the image below).
Prognosis
A study by Kalfa et al indicated that in infants and children with severe mitral regurgitation (MR) (mitral valve insufficiency), the mitral valve can be satisfactorily repaired using a standardized, reproducible surgical treatment strategy that includes leaflet debridement, annuloplasty, and leaflet augmentation. [4] The study, of 106 patients younger than 18 years, found that at last follow-up (mean period of 3.9 years), the rate of mortality was 4.5%; recurrent mitral regurgitation, 17%; reoperation, 23%; and valve replacement, 5.5%. The investigators also found that a regurgitation etiology associated with left ventricular outflow tract obstruction was the most important independent risk factor for recurrent regurgitation, reoperation, and valve replacement, although associated preoperative mitral stenosis and young age were also independent predictors for these. [4]
Complications
In patients with mechanical prostheses, administration of too much warfarin may result in excessive bleeding, whereas insufficient anticoagulation may lead to thromboembolism.
Patient Education
Asymptomatic children with mitral regurgitation (MR) (mitral valve insufficiency) require regular examinations because the indolent course of mitral regurgitation may be deceptive as long as the heart is able to compensate for the altered hemodynamics. Patients and families require education regarding specific medications, especially warfarin.
For patient education resources, see the Heart Health Center, as well as Mitral Valve Prolapse.
-
Acute stage of mitral regurgitation (MR) (mitral valve insufficiency).
-
Chronic compensated stage of mitral regurgitation (MR) (mitral valve insufficiency).
-
Chronic decompensated stage of mitral regurgitation (MR) (mitral valve insufficiency).
-
Dilated cardiomyopathy with significant mitral regurgitation (MR) (mitral valve insufficiency) by transthoracic echocardiogram (A) and cardiac magnetic resonance imaging (B).
-
Cleft mitral valve seen in parasternal short axis view (A) with mild mitral regurgitation (MR) (mitral valve insufficiency) in 4-chamber apical view (B).