Practice Essentials
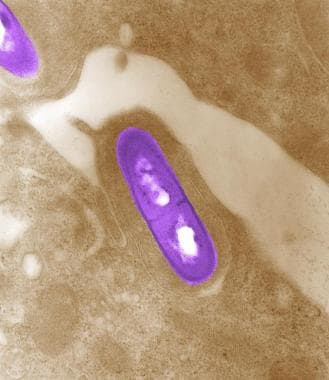
Listeriosis is an infection caused by the gram-positive motile bacterium Listeria monocytogenes. [1, 2, 3] Listeriosis is relatively rare and occurs primarily in newborn infants, elderly patients, and patients who are immunocompromised. [4, 5] See the image below.
Etiology
L monocytogenes is acquired via the ingestion of contaminated food products. Newborns acquire Listeria transplacentally, by ascending infection via ruptured amniotic membranes or upon exposure during vaginal delivery. [5]
Pathophysiology
L monocytogenes is a gram-positive, motile, rod-shaped bacterium that is ubiquitous in the environment. L monocytogenes can be isolated in soil, wood, and decaying matter in the natural environment; however, the principal route of acquisition of Listeria is through the ingestion of contaminated food products. Listeria has been isolated from prepared meat (eg, hot dogs, deli meat), dairy products, unwashed raw vegetables, and seafood. Soft cheeses and unpasteurized milk have been the most frequently incriminated dairy products. [6, 7, 8, 9, 10, 11, 12]
Ingestion of Listeria by pregnant women can result in nausea, vomiting, diarrhea, fever, malaise, back pain, and headache. [13] Many pregnant women can carry Listeria asymptomatically in their GI tract or vagina. Maternal infection with Listeria can result in chorioamnionitis, premature labor, spontaneous abortion, or stillbirth. Fetal infection can occur via transplacental transmission. Vertical transmission can also occur from mother to infant via passage through an infected birth canal or ascending infection through ruptured amniotic membranes. [14, 15] Nosocomial outbreaks from one infected infant to others in the same nursery are rare but have been reported.
Two clinical presentations of neonatal infections occur: early onset (< 5 d) and late onset (>5 d). Early onset neonatal listeriosis is usually associated with sepsis or meningitis. Late-onset neonatal listeriosis frequently presents with purulent meningitis. [16] Listeriosis often involves many organs with microabscesses or granulomas. A disseminated rash with small, pale, granulomatous nodules is histologically characteristic of granulomatosis infantisepticum. Beyond the neonatal period, most children with Listeria infections have an underlying immunodeficiency or are immunocompromised. Older children with Listeria infections frequently develop meningitis. [17, 18, 19]
Epidemiology
United States statistics
The estimated annual incidence of listeriosis is approximately 2-3 cases per million population. In the United States, an estimated 1600 people contract listeriosis every year. [20] Pregnant women account for 27% of all cases, and most occur during the third trimester. [5]
In a study of reported listeria cases from 2009-2011, the CDC reported a case fatality rate of 21%. Almost all cases occurred in high-risk groups, including older adults, pregnant women, and people who were immunocompromised. [21]
International statistics
The estimated annual incidence of listeriosis is approximately 4 cases per million population in Canada. Surveillance of listeria infections in Europe reported an incidence varying between 0.3 (Greece) and 7.5 (Sweden) cases per year. [22] After years of decreasing incidence, recent trends throughout Europe, in particular France and Scandinavia, show an increasing incidence. [23, 24, 25, 26, 27, 28, 29, 30, 31, 32] This trend is accounted for by increased cases in the population older than 60 years. Neonatal and maternal incidence remains stable. [33, 34]
Age-related demographics
Listeria infections occur most often in newborns and elderly patients. Neonatal infections can be subdivided into early onset and late-onset disease.
-
Early onset neonatal infections (< 5 d) begin at a mean age of 1.5 days.
-
Late-onset neonatal infections (>5 d) begin at a mean age of 14 days.
-
Postnatal infections usually occur in immunocompromised children and are less common than neonatal infections.
Prognosis
Prognosis is guarded and depends on whether meningitis or shock is present. [35]
Hydrocephalus, intellectual disability, and other CNS sequelae have been reported following meningitis.
Morbidity/mortality
Early onset neonatal listeriosis has a 20-40% mortality rate. [33] Late-onset neonatal listeriosis has a 0-20% mortality rate. The mortality rate in older children is less than 10%. Hydrocephalus, intellectual disability, and other CNS sequelae have been reported in survivors of Listeria meningitis.
Of all pregnancy-related cases, 22% resulted in fetal loss or neonatal death, but the mothers usually survived. [5]
A French nationwide prospective study by Charlier et al that included 818 listeriosis cases reported that the strongest mortality predictors in both bacteremia and neurolisteriosis were ongoing cancer, multi-organ failure, aggravation of any preexisting organ dysfunction, and monocytopenia. Blood-culture positive patients and those receiving adjunctive dexamethasone had higher neurolisteriosis mortality. [36]
Complications
Rhombencephalitis (brainstem encephalitis) is a well-recognized complication of CNS listeriosis. [37] Cranial nerve involvement has been reported in an immunocompetent toddler with novel H1N1 influenza. [38]
-
Electron micrograph of an artificially-colored Listeria bacterium in tissue.