Practice Essentials
In 1981, Palmer and Werner introduced the term triangular fibrocartilage complex (TFCC) to describe the ligamentous and cartilaginous structures that suspend the distal radius and ulnar carpus from the distal ulna (see the image below). [1] The TFCC is the major ligamentous stabilizer of the distal radioulnar joint (DRUJ) and the ulnar carpus. It is at risk for either acute or chronic degenerative injury. [2]
 Triangular fibrocartilage complex suspends distal radius and ulnar carpus from distal ulna. T=triquetrum; L=lunate; S=scaphoid. (Reprinted with permission from Palmer AK and Werner FW: The Triangular Fibrocartilage Complex of the Wrist - Anatomy and Function. J Hand Surg; 1981; 6:153)
Triangular fibrocartilage complex suspends distal radius and ulnar carpus from distal ulna. T=triquetrum; L=lunate; S=scaphoid. (Reprinted with permission from Palmer AK and Werner FW: The Triangular Fibrocartilage Complex of the Wrist - Anatomy and Function. J Hand Surg; 1981; 6:153)
Functions of the TFCC are as follows:
-
It provides a continuous gliding surface across the entire distal face of the two forearm bones for flexion-extension and translational movements (see the image below)
-
It provides a flexible mechanism for stable rotational movements of the radiocarpal unit around the ulnar axis
-
It suspends the ulnar carpus from the dorsal ulnar face of the radius
-
It cushions the forces transmitted through the ulnocarpal axis
-
It solidly connects the ulnar axis to the volar carpus
 Triangular fibrocartilage complex provides continuous gliding surface across entire distal face of radius and ulna to allow for flexion-extension and translational movements.
Triangular fibrocartilage complex provides continuous gliding surface across entire distal face of radius and ulna to allow for flexion-extension and translational movements.
Injuries to the TFCC present as ulnar-side wrist pain, frequently with clicking. Torn TFCCs constitute 35% of intra-articular fractures and 53% of extra-articular fractures. There is no correlation between ulnar styloid fractures and TFCC injuries. Patients with a torn TFCC display an average ulnar variance (radial shortening) of 4.6 mm (vs 2.5 mm for no tear) and an average dorsal angulation of 24° (vs 12° for no tear).
Since 1777, when DeSault's original dissertation first described DRUJ injuries, much has been written about this joint and the TFCC. As Palmer pointed out, [1, 3, 4] humans are differentiated from lower primates by a radiocarpal joint with a TFCC interposed between the ulna and carpus. [1] This TFCC improves wrist functional stability and allows six degrees of freedom at the wrist—flexion, extension, supination, pronation, and radial and ulnar deviation.
As interest in the TFCC evolved, open repair techniques for this structure were devised. Small-joint arthroscopy provided the opportunity for newer techniques in the debridement or repair of these structures.
Initial treatment of both symptomatic degenerative and traumatic TFCC tears consists of a period of conservative therapy (see Treatment). If a congruent reduction cannot be achieved or if the dorsal instability is unstable in 30° of supination, then arthroscopic evaluation of the TFCC is recommended with repair as needed. Repairing TFCC tears is contraindicated in the presence of infection or degeneration. Surgical options depend on the characteristics of the lesion.
Anatomy
As the name suggest, the TFCC is triangular in shape. Palmer found an inverse relation between ulnar variance and TFCC thickness of the TFCC: The TFCC is thicker in individuals who are ulnar minus. [5] Generally, the TFCC is 1-2 mm thick at its center. This may thicken to 5 mm where the TFCC inserts into the eccentric concavity of the ulnar head and projecting styloid.
The TFCC extends ulnarly to insert into the base of the ulnar styloid (see the first image below). Distally, it inserts into the lunate via the ulnolunate (UL) ligament and into the triquetrum via the ulnotriquetral (UT) ligament (see the second and third images below), the hamate, and the base of the fifth metacarpal. Radially, the TFCC arises from the ulnar margin of the lunate fossa of the radius (see the fourth image below).
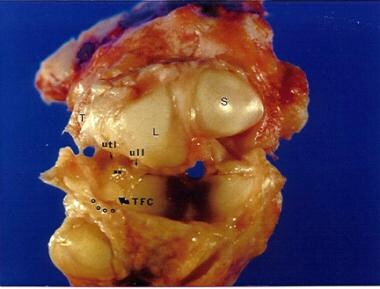 Ulnocarpal portion of triangular fibrocartilage complex (TFCC) is composed of discus articularis, ulnolunate ligament (ULL), and ulnotriquetral ligament (UTL). Distally, TFCC inserts into lunate via ULL and into triquetrum via UTL.
Ulnocarpal portion of triangular fibrocartilage complex (TFCC) is composed of discus articularis, ulnolunate ligament (ULL), and ulnotriquetral ligament (UTL). Distally, TFCC inserts into lunate via ULL and into triquetrum via UTL.
 Distally, triangular fibrocartilage complex inserts into lunate triquetrum via ulnolunate and ulnotriquetral ligaments. Triangular fibrocartilage complex solidly connects ulnar axis to volar carpus. Unlabeled arrow points to prestyloid recess. (Reprinted with permission from Palmer AK and Werner FW: The Triangular Fibrocartilage Complex of the Wrist - Anatomy and Function. J Hand Surg; 1981; 6:153)
Distally, triangular fibrocartilage complex inserts into lunate triquetrum via ulnolunate and ulnotriquetral ligaments. Triangular fibrocartilage complex solidly connects ulnar axis to volar carpus. Unlabeled arrow points to prestyloid recess. (Reprinted with permission from Palmer AK and Werner FW: The Triangular Fibrocartilage Complex of the Wrist - Anatomy and Function. J Hand Surg; 1981; 6:153)
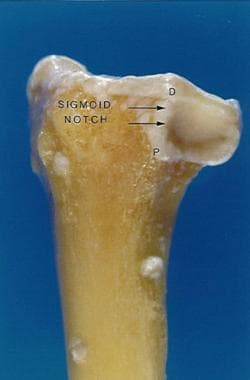 Sigmoid notch of distal radius with distinct dorsal, palmar, and distal margins and indistinct proximal margin; triangular fibrocartilage complex arises from ulnar margin of lunate fossa of radius. (Reprinted with permission from Fernandez D and Palmer AK. Fractures of the Distal Radius. In: Green's Operative Hand Surgery. Vol 1. 1999)
Sigmoid notch of distal radius with distinct dorsal, palmar, and distal margins and indistinct proximal margin; triangular fibrocartilage complex arises from ulnar margin of lunate fossa of radius. (Reprinted with permission from Fernandez D and Palmer AK. Fractures of the Distal Radius. In: Green's Operative Hand Surgery. Vol 1. 1999)
Underneath the TFCC is the ulnar head. The seat, or the convex portion of the ulnar head, articulates with the sigmoid notch of the radius (see the image below). The cartilage-covered nonarticular pole of the ulnar head is deep to the articular disk.
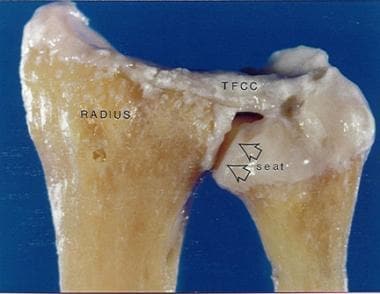 Seat of ulnar head articulates with sigmoid notch of distal radius. Radially, triangular fibrocartilage complex (TFCC) arises from ulnar margin of lunate fossa of radius. Ulnarly, TFCC inserts into base of ulnar styloid. (Reprinted with permission from Fernandez D and Palmer AK. Fractures of the Distal Radius. In: Green's Operative Hand Surgery. Vol 1. 1999)
Seat of ulnar head articulates with sigmoid notch of distal radius. Radially, triangular fibrocartilage complex (TFCC) arises from ulnar margin of lunate fossa of radius. Ulnarly, TFCC inserts into base of ulnar styloid. (Reprinted with permission from Fernandez D and Palmer AK. Fractures of the Distal Radius. In: Green's Operative Hand Surgery. Vol 1. 1999)
The ulnocarpal portion of the TFCC is composed of the discus articularis and the UL and UT ligaments (referred to by some as the disk carpal ligaments). Embryologic studies have demonstrated that these ligaments arise from the disk and are critical to the carpal suspensory function of the TFCC.
The dorsal and palmar branches of the anterior interosseous artery and dorsal and palmar radiocarpal branches from the ulnar artery supply blood to the periphery of the TFCC. These vessels supply the TFCC in a radial fashion, with histologic sections demonstrating that the vessels penetrate the peripheral 10-40% of the disk. The central portion and radial attachment are avascular.
Mikic demonstrated that the percentage of the peripheral disk that is vascularized is reduced from one third in a young patient to one fourth in patients of advanced age. [6]
Because the periphery of the TFCC has a good blood supply, tears in this region can be repaired. By contrast, tears in the central avascular area must be debrided because they have no potential for healing.
The richly vascularized dorsal radioulnar (DRU) ligament and palmar radioulnar (PRU) ligament are composed of thick, longitudinally oriented collagen fiber bundles that blend in with the central avascular fibrocartilaginous portion.
When the TFCC is viewed during wrist arthroscopy, the styloid attachment appears folded. Some of the blood vessels to the TFCC enter between these folds. This fold, combined with the vascular hilum, is termed the ligamentum subcruentum, which actually is the confluence of the TFCC and the V-shaped ligament (disk ligament) as it extends from the hilar area of the styloid to its twin insertions on the lunate and triquetrum.
From a distal perspective, the TFCC has two distinct insertions into the ulna—a superficial portion and a deep portion. The superficial components, the DRU and PRU ligaments, insert into the base of the styloid. The deep portion, the ligamentum subcruentum, inserts into the fovea near the axis of forearm rotation.
Controversy exists concerning the biomechanical changes of the TFCC during pronation and supination. A number of authors claim that the DRU ligament tightens during pronation and relaxes with supination; other authors claim the exact opposite.
Nakamura et al may have solved this question by using a custom-made surface coil allowing complete freedom of wrist motion. From magnetic resonance imaging (MRI) of the wrist in coronal and sagittal planes at maximal pronation and neutral and maximal supination, they showed that during pronation and supination, the TFCC twists at its origin. [7] This should result in friction between the proximal side of the disk proper and the ulnar head during rotation. The friction may increase in ulnocarpal abutment syndrome because of ulnar variance, potentially explaining the degeneration seen in Palmer class 2 TFCC tears (see Pathophysiology).
Pathophysiology
Palmer and Werner looked at the axial load distribution through the distal radius and ulna [8] and demonstrated that with normal axial loading, 20% of the force is transmitted through the ulna and 80% through the radius. Their data also illustrated that small changes in relative ulnar length can significantly alter load patterns across the wrist. For example, with a distal radius fracture that settles 2.5 mm, an increase in ulnar axial load of approximately 40% can be expected.
Palmer, Werner, Glisson, and Murphy demonstrated that the percentage of axial force transmitted through the ulna decreases by sequential removal of the horizontal portion of the TFCC. [5] This percentage decrease is accentuated with more positive ulnar variance.
In a cadaver study, Adams demonstrated that no significant kinematic or structural changes resulted from an excision that did not violate the peripheral 2 mm of the disk and that constituted less than two thirds of the disk area. [9]
TFCC tears are associated with a positive ulnar variance. Ulnar variance increases with pronation and grip and decreases with supination.
The floor of the extensor carpi ulnaris (ECU) tendon sheath broadly connects with the TFCC. After release of the TFCC from its distal ulna attachment, Tang demonstrated a 30% increase in ECU tendon excursion during wrist extension. [10] This suggests the following:
-
The TFCC is an important pulley for the ECU tendon
-
Disruption of the normal ECU excursion may contribute to abnormal loading and force transmission through the ulnar wrist and TFCC
Palmer classification of TFCC abnormalities
The Palmer classification divides TFCC abnormalities into two main classes, which are then further divided into several subtypes.
Palmer class 1 (traumatic) TFCC abnormalities are divided into the following subtypes:
-
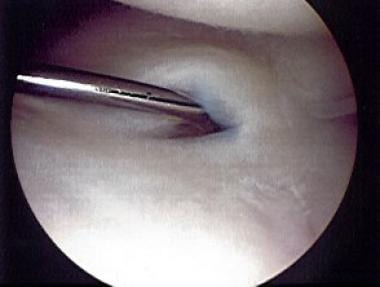
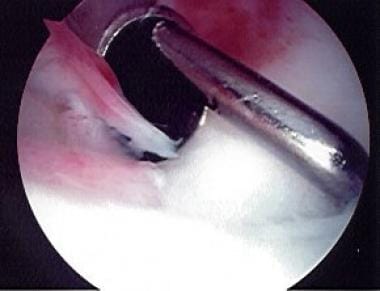
A - Central perforation (see the first, second, and third images below)
-
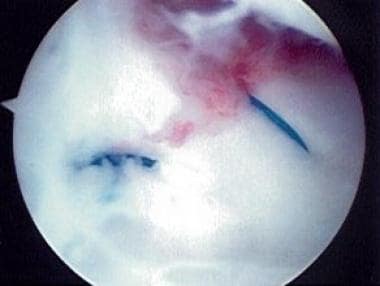
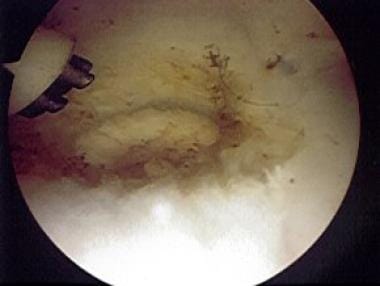
B - Ulnar avulsion (see the fourth, fifth, and sixth images below) with or without distal ulnar fracture
-
C - Distal avulsion
-
D - Radial avulsion with or without sigmoid notch fracture
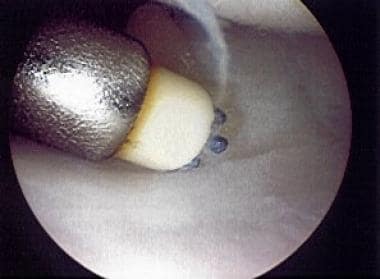 Palmer class 1A tear of triangular fibrocartilage complex after debridement, being treated with electrothermal wand.
Palmer class 1A tear of triangular fibrocartilage complex after debridement, being treated with electrothermal wand.
 Palmer class 1A tear of triangular fibrocartilage complex after debridement with shaver and thermal treatment.
Palmer class 1A tear of triangular fibrocartilage complex after debridement with shaver and thermal treatment.
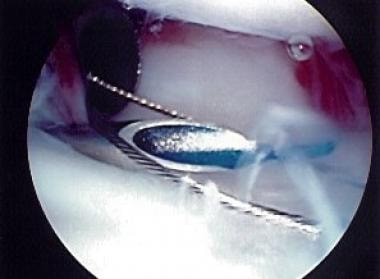 Palmer class 1B tear of triangular fibrocartilage complex treated with outside-in technique using 2-0 polydioxanone sutures and wire loop.
Palmer class 1B tear of triangular fibrocartilage complex treated with outside-in technique using 2-0 polydioxanone sutures and wire loop.
Palmer class 2 (degenerative [ulnocarpal abutment syndrome] stage) TFCC abnormalities are divided into the following subtypes:
-
A - TFCC wear
-
B - TFCC wear with lunate and/or ulnar chondromalacia
-
C - TFCC perforation with lunate and/or ulnar chondromalacia
-
D - TFCC perforation with lunate and/or ulnar chondromalacia and lunotriquetral (LT) ligament perforation
-
E - TFCC perforation with lunate and/or ulnar chondromalacia, LT ligament perforation, and ulnocarpal arthritis
In a small series, Nance et al described eight patients who were presumed to have solitary TFCC tears but were found on wrist arthroscopy to have a combination of 1A and 1B injuries. [11] They suggested that this combined pattern, which is not currently categorized in the Palmer classification system and is not reliably diagnosed preoperatively, might usefully be considered a new subtype in this system.
In 2022, Schmitt et al proposed a new CUP (central, ulnar, peripheral) classification for TFCC injuries, arguing that current classifications have significant drawbacks. [12]
Etiology
Causative conditions for TFCC injuries include the following:
-
Falls onto pronated hyperextended wrist
-
Power-drill injuries in which the drill binds and rotates the wrist instead of the bit
-
Distraction force applied to the volar forearm or wrist
Epidemiology
Mikic looked at 180 wrist joints in 100 cadavers, ranging in age from fetuses to 94 years. [6] He demonstrated that degeneration of the TFCC begins in the third decade of life and progressively increases in frequency and severity in subsequent decades. After the fifth decade of life, he noted no normal-appearing TFCCs. Viegas and Ballantyne found similar results. [13]
Prognosis
McNamara et al performed a systematic review and meta-analysis of 43 studies that addressed the outcomes of different treatment approaches for symptomatic Palmer type 1 TFCC injuries. [14] Patients who underwent debridement for any Palmer type 1 injury returned to work at a rate of 92%, but only 44% were free of pain. Of patients with 1B lesions that were repaired, 68.3% were able to return to work, and 41% had persistent pain. The 1D lesions were treated with both repair and debridement, and results were similar. Data for types 1A and 1C were limited. Patients with 1A lesions treated with debridement still had high rates of being unable to return to work.
Arthroscopic repair
A review by de Araujo et al of 17 patients (average age, 33 y) after arthroscopic repair of Palmer class 1B tears showed that at 8 months' follow-up, 16 patients (48%) were satisfied or very satisfied; one patient was not satisfied. [15] At 16-24 months' follow-up, 70% of the patients were satisfied.
Reiter et al performed a retrospective study of 46 patients who underwent arthroscopic repair of Palmer class IB tears to determine patients' functional and subjective outcomes, as well as whether clinical outcomes were related to ulnar length. [16] Good-to-excellent results were achieved in 63% of the patients, including increased range of motion (ROM) and grip strength and pain relief. Neutral or positive ulnar variance was not a contraindication for repair and did not necessitate simultaneous ulnar shortening.
Sagerman and Short reviewed 12 patients after arthroscopic repair of Palmer class 1D tears (average follow-up, 17 mo) and found good or excellent results in 67% of patients. [17]
Trumble et al reviewed 24 patients (average age, 31 y) after arthroscopic repair of Palmer classes 1B, 1C, and 1D tears. [18] Treatment occurred within 4 months after injury, with a follow-up of 34 months. Postoperative ROM was 89%, and grip strength was 85%. Thirteen of 19 patients returned to their original jobs or sports. Follow-up studies demonstrated that the TFCC was intact in 12 of 15 patients.
Corso et al reviewed 44 patients (average age, 32.5 y) and 45 wrists with zone-specific repair and follow-up of 37 months and found excellent results in 29 patients, good results in 12, fair results in one, and poor results in three. [19]
In a study of 16 competitive athletes with wrist TFCC, McAdams et al found that arthroscopic debridement or repair of TFCC injury provided pain relief and allowed patients to return to play, with slower recovery in patients with concomitant ulnar-side wrist injuries. [9] .
Yao et al compared an all-arthroscopic TFCC repair technique with an outside-in technique in 10 matched pairs of fresh-frozen cadaveric wrists and found that the all-arthroscopic technique resulted in decreases in operating time, postoperative immobilizations, and irritation from suture knots below the skin. [20, 21]
In a study of 75 patients who underwent TFCC repair by arthroscopic (n = 36) or open technique (n = 39), Anderson et al found that there was no statistical difference in clinical outcome for the two approaches to TFCC repair. [22] They did note an increased rate of postoperative superficial ulnar pain in patients who underwent open repair (14/39) as compared with those who underwent arthroscopic repair (8/36). Females had a higher rate of reoperation.
In a cadaveric study comparing the biomechanical strength of knotless suture anchor repair and the traditional outside-in repair of peripheral TFCC tears, Desai et al concluded that the all-arthroscopic suture anchor TFCC repair was biomechanically stronger than the outside-in repair and that the former allowed repair of both superficial and deep layers of the articular disk directly to bone, thereby restoring native TFCC anatomy. [23] They suggested that the absence of knots might prevent irritation to the surrounding soft tissues.
Arthroscopic debridement
Minami et al reviewed 16 patients (average age, 30 y) with a follow-up of 35 months. Palmer class 1 tears were found in 11 patients, and Palmer class 2 tears were found in five. [24] Of the 16 patients, 13 returned to their previous jobs. Positive ulnar variance and LT tears were associated with a poor outcome; Palmer class 1 tears were associated with excellent results; and Palmer class 2 tears were associated with poor results.
Westkaemper et al reviewed 28 patients (average age, 30 y) with a follow-up of 15.4 months. Excellent results were found in 13 patients, with good results in eight, fair results in two, and poor results in five. [25]
De Smet et al conducted a retrospective survey of 46 patients who underwent debridement with or without wafer distal ulna resection. [26] Patients were sent a questionnaire on pain, disability, and time off from work. Mean scores on the Disabilities of the Arm, Shoulder, and Hand (DASH) scale decreased from 42 to 28. The pain was considered severe in 12 patients; 32 patients were satisfied. There were significant differences in the outcome between use of debridement only and use of debridement with wafer resection of the distal ulna.
Ulnar shortening
Minami and Kato reviewed 25 patients (average age, 32 y) with follow-up of 35 months. [27] Ulnar variance averaged more than 3.5 mm. Ulnar-shortening osteotomies of 3 mm, fixed with a 6-hole 3.5-mm dynamic compression plate (DCP), were performed. Twenty-three patients also had arthroscopy. Palmer class 1 tears were found in 15 patients; only the flap was removed. Palmer class 2 tears were found in eight; no debridement was performed.
Complete relief or only occasional mild pain was found in 23 patients. [27] Of the 25 patients, 23 returned to their original work. Osteotomies healed at an average of 7 weeks. This research suggests that ulnar shortening is indicated in both traumatic and degenerative tears associated with ulnar positive variance.
Trumble et al reviewed 21 patients with treatment delays longer than 6 months and follow-up of 29 months. [28] Palmer class 1 tears were repaired. Ulnar-shortening osteotomies of 2-3 mm fixed with 6-hole 3.5-mm DCPs were performed. Complete pain relief was found in 19 of 21 patients. Grip strength was 83%; ROM was 81% of normal. Treatment delays longer than 6 months from the time of injury resulted in a higher recurrence of symptoms; in these situations, the authors recommended combining arthroscopic repair with ulnar shortening.
Hulsizer et al reviewed 97 patients (average age, 34 y; average ulnar variance, 0.4 mm) with central or nondetached ulnar peripheral tears initially treated with debridement. [29] Persistent pain more than 3 months after surgery was reported by 13 patients. A 2-mm ulnar-shortening osteotomy, fixed with a 6-hole 3.5-mm DCP, was performed on these 13 patients. Complete pain relief at 2.3-year follow-up was reported by 12 patients. An ulnar-shortening osteotomy of 2 mm was recommended for patients in whom arthroscopic debridement failed.
In a retrospective study (N = 256), Yamanaka et al compared preoperative and postoperative TFCC thickness and TFCC angle, using MRI to quantitatively evaluate the effect of ulnar-shortening osteotomy on disk regeneration and the suspension effect on the TFCC. [30] They found that ulnar-shortening osteotomy yielded a high residual potential for regeneration in the disk proper. There was no correlation between disk regeneration or the suspension effect on the TFCC and the Mayo wrist score.
Seo et al assessed the results of arthroscopic peripheral repair (n = 15) against those of arthroscopic debridement (n = 16) for treatment of chronic unstable TFCC tears in 31 ulnar-positive patients undergoing ulnar-shortening osteotomy (minimum follow-up, 24 mo). [31] Improvements were noted in both groups; however, grip strength, DASH, and Patient-Rated Wrist Evaluation (PRWE) scores were better in the repair group than in the debridement group. Recovery from DRUJ instability noted during preoperative evaluation was superior in the repair group as well.
-
Triangular fibrocartilage complex suspends distal radius and ulnar carpus from distal ulna. T=triquetrum; L=lunate; S=scaphoid. (Reprinted with permission from Palmer AK and Werner FW: The Triangular Fibrocartilage Complex of the Wrist - Anatomy and Function. J Hand Surg; 1981; 6:153)
-
Triangular fibrocartilage complex provides continuous gliding surface across entire distal face of radius and ulna to allow for flexion-extension and translational movements.
-
Distally, triangular fibrocartilage complex inserts into lunate triquetrum via ulnolunate and ulnotriquetral ligaments. Triangular fibrocartilage complex solidly connects ulnar axis to volar carpus. Unlabeled arrow points to prestyloid recess. (Reprinted with permission from Palmer AK and Werner FW: The Triangular Fibrocartilage Complex of the Wrist - Anatomy and Function. J Hand Surg; 1981; 6:153)
-
Relation of triangular fibrocartilage complex to distal radius and ulnar styloid.
-
Ulnocarpal portion of triangular fibrocartilage complex (TFCC) is composed of discus articularis, ulnolunate ligament (ULL), and ulnotriquetral ligament (UTL). Distally, TFCC inserts into lunate via ULL and into triquetrum via UTL.
-
Sigmoid notch of distal radius with distinct dorsal, palmar, and distal margins and indistinct proximal margin; triangular fibrocartilage complex arises from ulnar margin of lunate fossa of radius. (Reprinted with permission from Fernandez D and Palmer AK. Fractures of the Distal Radius. In: Green's Operative Hand Surgery. Vol 1. 1999)
-
Seat of ulnar head articulates with sigmoid notch of distal radius. Radially, triangular fibrocartilage complex (TFCC) arises from ulnar margin of lunate fossa of radius. Ulnarly, TFCC inserts into base of ulnar styloid. (Reprinted with permission from Fernandez D and Palmer AK. Fractures of the Distal Radius. In: Green's Operative Hand Surgery. Vol 1. 1999)
-
Palmer class 1A tear of triangular fibrocartilage complex that is being probed.
-
Palmer class 1A tear of triangular fibrocartilage complex after debridement, being treated with electrothermal wand.
-
Palmer class 1A tear of triangular fibrocartilage complex after debridement with shaver and thermal treatment.
-
Traumatic ulnar-side Palmer class 1B tear of triangular fibrocartilage complex.
-
Palmer class 1B tear of triangular fibrocartilage complex treated with outside-in technique using 2-0 polydioxanone sutures and wire loop.
-
Completion of outside-in repair for Palmer class 1B tear of triangular fibrocartilage complex.