Overview
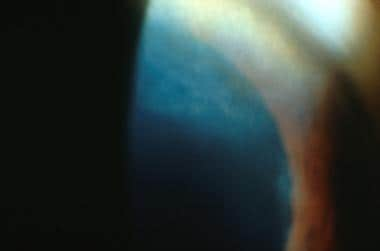
Interstitial keratitis (IK) is a broad, descriptive term that historically became synonymous with syphilitic disease. Although congenital syphilis remains the leading cause of interstitial keratitis, various bacterial, viral, parasitic, and autoimmune causes of interstitial keratitis are known. An example of interstitial keratitis associated with congenital syphilis is shown in the image below.
 This photograph depicts a child with a bilateral eye condition known as interstitial keratitis (IK), a stigma related to congenital syphilis.
This photograph depicts a child with a bilateral eye condition known as interstitial keratitis (IK), a stigma related to congenital syphilis.
Interstitial keratitis may develop in persons who have untreated syphilis, the vast majority of whom have congenital syphilis with ocular symptomatology presenting at an average age of two years. Cases reports have described interstitial keratitis in patients infected with syphilis later in life. Practitioners should attempt to determine whether a patient has been treated appropriately in the past to prevent the development of neurosyphilis.
Another important association to keep in mind is that patients with interstitial keratitis due to Cogan syndrome are more likely to have a history of systemic vasculitides, and prompt referral to a rheumatologist may be critical.
A high index of clinical suspicion is required. Remember that syphilis can mimic almost any intraocular inflammatory condition. Misdiagnosis leads to nontreatment or treatment with the wrong medication, allowing the disease to progress and potentially result in vision loss.
Intravitreal corticosteroid can modulate the immune response to intraocular syphilis; vigilance is required, particularly in high-risk patients. [1]
For further information, see Syphilis.
Pathophysiology
By definition, interstitial keratitis is a nonsuppurative inflammation, which is characterized by cellular infiltration of the corneal stroma. In general, no primary involvement of the corneal epithelium or endothelium occurs.
Inflammation may be either the direct result of an infectious process or, more commonly, secondary to an immunologic response to a specific foreign antigen. This immunologic response may take the form of antigen-antibody complex deposition, complement-mediated disease, or a delayed-type hypersensitivity reaction.
Acute interstitial keratitis may be triggered by ocular surface inflammation and following intraocular surgery. Corneal inflammation most often affects the deep stromal layers, either as multifocal infiltrates or as a diffuse process. Corneal stromal edema may result from the inflammation, resulting in the ground-glass cornea.
Variability of the extent of corneal stromal neovascularization depends on the severity of the inflammation that has been present. Typically, the neovascularization begins at the corneal limbus and may occur at any level, although it most commonly is seen in the deeper stromal layers. Stromal inflammation overlying the vessel often causes a salmon-colored patch due to the pinkish color imparted by the stromal vessels. Intrastromal hemorrhage also may occur.
Interstitial keratitis may progress to the regression phase, during which scarring of the corneal stromal and collagen remodeling occur. The superficial vessels resorb, and the deeper vessels may constrict, resulting in the ghost vessels that are seen as a late finding of syphilitic interstitial keratitis.
Epidemiology
Interstitial keratitis is generally seen in the context of syphilis and, less commonly, in the context of herpes simplex keratitis and Cogan syndrome. In various countries in which mycobacterial diseases (eg, tuberculosis, leprosy) are endemic, these and parasitic causes of interstitial keratitis may be seen with greater frequency. Congenital interstitial keratitis, which accounts for approximately 90% of all cases, commonly appears at age 6-12 years. Acquired syphilitic interstitial keratitis generally manifests in the third to fifth decade of life.
Clinical Presentation
Patient history
In the acute phase, interstitial keratitis typically causes decreased vision, photophobia, tearing, pain, and blepharospasm. Late-phase symptoms consist of decreased visual acuity in the absence of ocular discomfort.
Congenital syphilis tends to cause acute symptoms in childhood. [2] Patients may give a history of one or both eyes being red and painful for months as a child. They may remember being admitted to the hospital or confined to bed, and they may not have been allowed to go to school for many months. They may give a history of prolonged intravenous antibiotics or multiple injections as treatment.
Physical examination
Congenital interstitial keratitis, which accounts for approximately 90% of cases, commonly appears at age 6-12 years. Conjunctival hyperemia, corneal edema, and infiltrates are present with lacrimation and photophobia.
The corneal stroma exhibits areas of dense, white, stromal necrosis and vascularization, which may be either diffuse or focal. The active vascularization contributes to the pinkish color of the cornea and is termed the salmon patch of Hutchinson. The condition generally begins unilaterally and becomes bilateral in 80-90% of cases. Involvement of the contralateral eye may occur as early as 2 months or as late as 15 years after inflammation of the first eye.
In acquired cases, active interstitial keratitis manifests as stromal inflammation, especially in the peripheral cornea. Marginal infiltrates of the anterior stroma may be present, usually in association with anterior uveitis. Evidence of stromal neovascularization just anterior to the Descemet membrane may be present.
Once the initial inflammation has resolved, which may take many months, the cornea may exhibit mild-to-severe scarring and thinning. The scarring tends to be in the middle to posterior corneal stroma. Vascular regression often leaves behind remnants known as ghost vessels. Endothelial decompensation may follow, resulting in additional central corneal edema later in life.
Other Ophthalmic Findings in Syphilis
In addition to interstitial keratitis, syphilis is associated with the following ocular disorders (also see the images below):
-
Episcleritis
-
Scleritis
-
Iritis
-
Iris papules
-
Chorioretinitis
-
Papillitis
-
Retinal vasculitis
Anterior uveitis with or without interstitial keratitis
Syphilitic anterior uveitis is unilateral in 56% of cases. One half of these cases are granulomatous, with mutton-fat keratic precipitates on the corneal endothelium, in 50% of cases.
Iris nodules with or without interstitial keratitis
In patients with syphilis, treponemal emboli in the iris blood vessels may cause vascular tortuosity and dilatation, resulting in iris nodules. These may take the following forms:
-
Iritis roseate (small, dilated collections of capillaries within the iris)
-
Iritis papulose (iritis roseata increasing in size to resemble a papule)
-
Iritis nodosa (iritis papulose increasing in size forming a yellow-red nodule)
Posterior uveitis with or without interstitial keratitis
Posterior uveitis occurs in 9-18% of cases of ocular syphilis. Panuveitis occurs in 27-47% of this group. Intravitreal inflammatory cells are typically present.
Examination may disclose any of the following:
-
Vasculitis with or without vascular occlusion
-
Macular edema
-
Stellate maculopathy
-
Disciform macular detachment
-
Serous macular/retinal detachment
-
Pseudo–retinitis pigmentosa (pseudo-RP)
-
Retinal detachment
-
Neuroretinitis
-
Papillitis
-
Diffuse chorioretinitis
-
Uveal effusion
-
Central retinal vein occlusion (CRVO)
-
Subretinal neovascular membrane (SNVM) formation
-
Acute retinal necrosis
-
Acute idiopathic big blind spot enlargement syndrome
Syphilitic posterior placoid chorioretinitis are present in HIV-positive patients. Findings include the following:
-
Large, flat, dry, yellowish, or gray mottled patterns; macular or juxtapupillary placoid lesions at the retinal pigment epithelium (RPE) layer
-
Leopard spot hypofluorescence on fluorescein angiography
Chen and Lee reported a case of acute unilateral maculopathy due to posterior placoid chorioretinitis associated with syphilis in an immunocompetent patient. [3] Ophthalmoscopy showed a unilateral yellowish placoid lesion at the macula. Positive syphilis serology confirmed active infection. No other systemic signs of syphilis were noted. Treatment with intravenous benzylpenicillin 1.2 g every 4 hours for 2 weeks resulted in resolution of the lesions.
Conjunctiva findings with or without interstitial keratitis
Conjunctival signs of syphilis include the following:
-
Chancre in primary syphilis
-
Nonspecific conjunctivitis in secondary syphilis
-
Gammas, rubbery tumorlike lesions, are associated with tertiary syphilis.
Scleritis/episcleritis with or without interstitial keratitis
Scleritis or episcleritis is usually present only in secondary syphilis. It may be nodular or diffuse.
Neuro-ophthalmic manifestations with or without interstitial keratitis
The following syphilitic neuro-ophthalmic manifestations may occur with or without syphilitic interstitial keratitis:
-
Papillitis
-
Optic neuritis
-
Optic peri neuritis
-
Papilledema
Lid and eyebrow changes with or without interstitial keratitis
Chancre of the lids or eyebrows rarely occurs in the primary stage of syphilis; however, loss of the eyebrow at its temporal aspect has been reported in secondary and tertiary syphilis. Tarsitis or lid abscess rarely occurs in the tertiary stage.
Pseudoepitheliomatous hyperplasia has also recently been reported as a rare occurrence related to the gummas of tertiary syphilis. These lesions are generally elevated, and they have an uneven surface that is either ulcerated or crusty, appearing similar to squamous cell carcinoma or basal cell carcinoma.
Cataract
Cataract has frequently been seen in patients with syphilis; however, whether the development is caused by Treponema pallidum or the uveitis associated with the disease is unknown.
Glaucoma
Glaucoma in patients with syphilitic interstitial keratitis is almost always associated with uveitic inflammation. In congenital syphilis, interstitial keratitis is associated with adult secondary glaucoma in 15-20% of patients. The glaucoma develops an average of 27 years after the initial episode of interstitial keratitis has subsided.
This may be a deep-chamber, open-angle type and a shallow-chamber, narrow-angle type, usually associated with peripheral anterior synechiae. Both types occur with equal frequency and have characteristic changes of congenital syphilis, such as corneal scarring with ghost vessels and chorioretinal atrophy.
Nonocular Findings
Nonocular findings of congenital syphilis may be helpful in establishing the diagnosis of syphilis. These include dental abnormalities (Hutchinson teeth), facial asymmetry, saddle-nose deformity, saber shins, deafness, and intellectual disability.
Complications of Interstitial Keratitis
Paroxysmal cold hemoglobinemia (PCH) is a rare type of autoimmune hemolytic anemia, primarily occurring in children. PCH manifests as massive intravascular hemolysis with anemia and hemoglobinuria, usually of abrupt onset in the setting of an infectious disease. Synonyms of PCH include Donath-Landsteiner syndrome and immune hemolytic anemia. Most cases of PCH recorded in the early medical literature were associated with congenital syphilis or late syphilis. Today, because of syphilis treatment regimens, syphilitic PCH is extremely rare. Currently, PCH is almost always encountered as an acute transient syndrome in young children with a recent history of a viral illness, and a relationship to cold exposure is rare.
Etiology of Interstitial Keratitis
Interstitial keratitis may be attributed to several systemic illnesses, including bacterial, viral, and parasitic infections, as well as Cogan syndrome, which can be associated with various systemic vasculitides.
Syphilis
Interstitial keratitis in syphilis may be due to an immune-mediated reaction to an unknown treponemal antigen. Interstitial keratitis may be seen in both congenital and acquired syphilis.
Mycobacterial infections
Tuberculosis and leprosy are 2 mycobacterial infections that may be causative agents in the pathogenesis of interstitial keratitis.
Internationally, tuberculosis remains an important public health issue, and in the United States, tuberculosis has become a relevant topic due to increased immigration from endemic areas, development of resistant strains of Mycobacteria, and human immunodeficiency virus (HIV) infection.
Although primary tuberculosis infection of the eye is extremely rare, interstitial keratitis may be associated with pulmonary tuberculosis. Even in this setting, it is extremely rare and, when present, usually is unilateral. In keeping with the other types of interstitial keratitis, the pathogenesis seems to be an immune reaction to tuberculous antigens within the cornea. Clinical findings are similar to interstitial keratitis due to other disorders.
Leprosy is caused by Mycobacterium leprae and characteristically infects the skin and peripheral nerves. Two forms of leprosy are noted, tuberculous and lepromatous. Interstitial keratitis may also be an ocular finding of leprosy (Hansen disease), and, in contrast to that seen in tuberculosis, lepromatous interstitial keratitis is usually bilateral.
Another distinguishing characteristic of lepromatous interstitial keratitis is that the organisms have been found throughout the stroma, implying that a direct infectious etiology may occur, in contrast to an immunologic etiology. Clinical findings of interstitial keratitis are like that in tuberculous interstitial keratitis. Prognosis for maintenance of vision is poor owing to the widespread involvement of the corneal nerves in lepromatous interstitial keratitis.
Lyme disease
Lyme disease is a systemic infectious disease caused by the bacterium Borrelia burgdorferi and is transmitted to humans through the bite of infected black-legged ticks. Clinically, it is distinguished by 3 stages, and ocular involvement typically occurs in stage 2 and stage 3. [4] Stage 1 represents the viral prodrome with a flulike illness and the typical bull's eye lesions on the skin, erythema chronicum migrans. Stage 2 is characterized by neuro-ophthalmologic manifestations. Keratitis, along with uveitis and vasculitis, may rarely occur in stage 3.
Interstitial keratitis in patients with Lyme disease does not commonly feature stromal edema, but it is otherwise similar to interstitial keratitis due to other causes. Lyme keratitis also can appear as large nummular infiltrates in various levels of the stroma in the absence of corneal neovascularization.
Parasitic infections
Parasitic infections are rare causes of interstitial keratitis in the United States.
Acanthamoeba is a free-living amoeba, which may cause a severe keratitis, especially in patients with a history of contact lens wear and more typically contact lens abuse. In prior decades, the use of homemade saline solutions was found to be a cause of Acanthamoeba keratitis. The use of contact lenses while swimming, typically in a freshwater body of water in a warm climate, is another risk factor.
Acanthamoeba keratitis may have various presenting characteristics, but the most significant symptom is pain out of proportion to clinical findings. Although epitheliopathy may also be noted, primary stromal involvement, including inflammatory edema, may be seen, which can resemble interstitial keratitis. In typical Acanthamoeba keratitis, stromal neovascularization is not an early finding.
Onchocerciasis (river blindness) is the result of infection by the nematode Onchocerca volvulus. Ocular involvement is the result of the migration of the microfilariae to the ocular tissues. Onchocerciasis occurs principally in Africa, but isolated foci also exist in Yemen and parts of Central and South America.
Interstitial keratitis caused by onchocerciasis has been described as beginning in the peripheral cornea, followed by progressive spread centripetally. Vascularization and complete opacification of the cornea may result, but corneal thinning is not a significant feature in this condition.
Leishmania is a protozoan agent commonly seen in Asia, Africa, and South America. It is carried by the sand fly vector and is divided into cutaneous and visceral forms. Typically, 2 types of keratitis are seen. Necrotizing keratitis may progress to corneal necrosis and perforation. However, a second presentation is that of typical interstitial keratitis with late corneal scarring and thinning.
Trypanosoma cruzi is responsible for Chagas disease in the Americas, and Trypanosoma brucei is responsible for trypanosomiasis in Africa, also known as African sleeping sickness. Interstitial keratitis may be seen in the African form.
Microsporidia are small intracellular protozoans that have been primarily isolated from patients with acquired immunodeficiency syndrome (AIDS) who had developed superficial keratoconjunctivitis. They also rarely cause keratitis in immunocompetent individuals.
Viral infections
Infections of the cornea by herpes simplex virus produces myriad clinical findings. A complete discussion is beyond the scope of this section. Herpetic stromal disease may take the form of interstitial keratitis and represents an important entity in the differential diagnosis. Typical findings of interstitial keratitis may be present along with an immune ring, which may be diagnostic.
Epstein-Barr virus and herpes zoster/varicella are other viruses that may have variable presentation in corneal disease. Unilateral or bilateral, multifocal or discrete infiltrates may be present, which may benefit from topical corticosteroids.
Mumps caused by Rubulavirus typically causes lacrimal gland inflammation, but cornea involvement may also occur. The presentation ranges from punctate epithelial keratopathy to nummular keratitis.
Corneal involvement in measles (rubeola) is typically a superficial keratitis and is generally self-limiting. However, measles in patients with malnutrition-related vitamin A deficiency are susceptible to stromal infiltration and perforation.
A single case of interstitial keraritis presumed due to the COVID-19 virus has been reported. [5]
Cogan syndrome
The acquired triad of nonsyphilitic interstitial keratitis, vestibuloauditory disease, and associated autoimmune vasculitis is known as Cogan syndrome and was first described in 1945. [6] In this condition, a sudden onset of vestibuloauditory symptoms (eg, tinnitus, vertigo, nausea, vomiting) occurs, together with corneal inflammation and often accompanied by autoimmune disorders (eg, polyarteritis nodosa, Wegener granulomatosis, rheumatoid arthritis).
In contrast to the deafness associated with syphilitic interstitial keratitis, the hearing loss in Cogan syndrome also has the vestibular symptoms described above. Although the exact pathogenesis is unknown, the disease process probably represents an immune reaction against the common antigen found in the cornea and in the inner ear.
Corneal findings are very similar to those seen in syphilitic interstitial keratitis, with lymphocytic infiltration of the deep stroma with variable neovascularization.
Differential Diagnosis
The differential diagnosis of interstitial keratitis includes the following:
-
Corneal manifestations of HIV infection
Other problems to be considered include the following:
-
Corneal dystrophies
-
Metabolic corneal disorders
Laboratory Studies
Laboratory testing in interstitial keratitis is directed toward diagnosis of the underlying etiology. Typically, this will be syphilis, but testing for tuberculosis or other entities may be indicated, depending on the clinical presentation.
Syphilis testing
A diagnosis of syphilitic interstitial keratitis is often based on the clinical findings and by serologic testing. Serologic tests for syphilis include treponemal and nontreponemal tests.
Serologic nontreponemal tests for syphilis include Venereal Disease Research Laboratory (VDRL) and rapid plasma reagin (RPR). Nontreponemal testing detects antibodies directed against cardiolipin (lecithin) cholesterol antigens. It is simple and convenient for routine screening at the local level. It is a frequent local requirement for premarital and prenatal serology. The false-positive rate for pregnant women is 1-2%.
A minimum of 1-3 weeks must pass from the onset of primary syphilis infection for the test to turn positive. The results are usually positive in primary syphilis and are invariably positive in secondary syphilis.
A high titer (>1:16) usually indicates active disease. Biologic false-positive tests (usually < 1:8) occur in intravenous drug users, in many acute infections (eg, infectious mononucleosis, mycoplasmal infection, malaria, leprosy), in various chronic disorders (eg, systemic lupus erythematosus), and possibly pregnancy.
The VDRL titer reflects the systemic activity of the disease. Its major value is in monitoring the response to treatment. Quantification of VDRL always should be performed before onset of treatment. A persistent fall in VDRL titers after treatment provides essential evidence of an adequate response to therapy. Nontreponemal test titers should decrease by 4-fold within 3 months of adequate treatment of primary or secondary disease, and they should decrease by 8-fold within 6 months following therapy for early latent disease.
Reactive and weakly reactive nontreponemal test results should be confirmed with treponemal serological testing of antibody absorption (FTA-ABS).
Serologic treponemal tests include micro-hemagglutination T pallidum (MHA-TP), FTA-ABS, T pallidum particle agglutination (TPA). Their greatest value is in distinguishing false-positive from true-positive reagin test results and in diagnosing late syphilis when blood and CSF reagin test results may be negative. These are highly sensitive and specific tests. Titers are not correlated with clinical activity.
The FTA-ABS test is not useful in monitoring response to therapy because it typically remains positive for life. The FTA-ABS test is 98% sensitive, even in latent syphilis. FTA-ABS test and TPA test are preferred over MHA-TP.
Other syphilis tests include dark-field immunofluorescence microscopy (direct technique). In this test, fluorescein-labeled anti-T pallidum antibodies are used in an immunofluorescence analysis of exudate or samples are taken from a lesion suggestive of syphilis. The antibody attaches to syphilitic organisms displaying a motile apple-green, corkscrew-shaped T pallidum.
On electron microscopy, T pallidum organisms can be seen in interstitial and perivascular spaces. Ganzfeld electroretinogram (ERG) was markedly reduced in a case of acute syphilitic posterior placoid chorioretinitis; multifocal ERG in the affected area was not recordable.
Indocyanine green (ICG) angiography may be a valuable tool in the assessment of patients with active ocular syphilis. ICG angiography can help identify retinal and choroidal vascular anomalies that would otherwise go undetected by funduscopy and/or fluorescein angiography. ICG angiography can also be useful in monitoring antitreponemal therapy. Late-phase scattered hyperfluorescent spots and persistent staining of retinal vessels were observed
Testing for other diseases
To diagnose latent tuberculosis, a purified protein derivative (PPD) test should be performed. Diagnosis of active tuberculosis requires sputum testing for acid-fast bacteria.
Lyme titers and enzyme-linked immunosorbent assay (ELISA) may be helpful in establishing the diagnosis of Lyme disease.
Serologic testing for anti-Hsp70 antibodies may assist in the diagnosis of Cogan syndrome, although this remains largely a diagnosis of exclusion. Lymphocytosis and an elevated erythrocyte sedimentation rate (ESR) have been described in those patients with an active systemic vasculitis. Human leukocyte antigen B17 (HLA-B17) may also be more prevalent in patients with Cogan syndrome, although the results are equivocal.
HIV testing
Patients with ocular syphilis should be evaluated for HIV and vice versa. Reports indicate that young adult patients who are HIV positive often have ocular syphilis.
HIV-infected patients HIV may experience an aggressive course of syphilis, rendering standard therapy for primary and secondary syphilis inadequate.
Lumbar Puncture
Lumbar puncture is used in the evaluation for asymptomatic neurosyphilis. Patients with positive syphilitic serologic test results and neurological symptoms should have their CSF examined for VDRL titers, total protein, and cell counts, including a differential count. An elevated WBC count with a predominance of lymphocytes in the CSF or an elevated total protein level, even without a positive CSF VDRL test, is indicative of neurologic involvement, and the patient should be treated for neurosyphilis.
Polymerase Chain Reaction
PCR has a diagnostic role in unusual or atypical ocular inflammation. It can be used on aqueous or vitreous specimens
Histologic Findings
The organisms can often be seen in superficially infected corneal epithelial lesions. A diffuse or focal lymphocytic infiltration is characteristic, particularly perivascularly. The tissue reaction is notable for stenosing intimal fibroplasia of small arteries and arterioles (eg, onion-skinning, obliterative endarteritis), as well as perivascular plasma infiltrate with some lymphocytes and macrophages. It may be found in the iris, ciliary body, or choroid.
Chronic granulomatous inflammation containing epithelioid histiocytes and multinucleated giant cells is present. Overlying epidermal changes in skin can be hyperplastic (eg, condylomata lata) or ulcerating (eg, chancre). In tertiary disease, gummas are present (ie, areas of coagulative necrosis surrounded by lymphocytes, plasma cells, and possibly giant cells), and organisms are more abundant. Warthin-Starry silver stain, a specialized direct staining technique, is sometimes used.
Treatment & Management
Treatment of syphilis
It is critical to remember that congenital syphilis is a preventable disease but continues to impose significant global health and economic burdens. Early syphilis can be completely eliminated with a single injection of penicillin, and treating pregnant women with penicillin is 98% effective at preventing congenital syphilis. Universal prenatal screening is the most effective way to prevent syphilis-associated morbidity and mortality.
In the first four years of acquiring syphilis, untreated women have a 70% chance of transmitting the infection to their fetus.
Treatment of interstitial keratitis depends on the specific underlying disorder.
The use of topical corticosteroids has markedly changed the natural history of interstitial keratitis due to congenital syphilis. Without the use of these anti-inflammatory modifiers, the typical scenario was permanent corneal opacity with variable visual outcome. Due to their anti-inflammatory properties, topical corticosteroids reduce inflammation and neovascularization and often result in better visual acuity than if the condition were left untreated.
Ocular therapy is concentrated on reducing the local inflammatory reaction, as well as controlling the other sequelae of the inflammation, most commonly elevated intraocular pressure. Although the corneal inflammation associated with interstitial keratitis resolves spontaneously, the use of topical corticosteroids shortens the duration and the severity of the corneal inflammation. Intravitreal corticosteroid can modulate the immune response to intraocular syphilis; vigilance is required, particularly in high-risk patients. [1]
Studies have shown that recurrences are fewer and visual outcomes better in patients who are treated with topical corticosteroids in a tapering fashion over a long period of time. The usual antiglaucoma medications may be used as needed to control intraocular pressure.
Patients with ocular syphilis should be treated similarly to patients with neurosyphilis. The treatment regimen is the same even without cerebrospinal fluid (CSF) evidence of neurosyphilis. The blood-ocular barrier is similar to the blood-brain barrier in terms of decreasing the penetration of drugs. Patients with syphilitic ocular inflammation may have CNS syphilis without a Venereal Disease Research Laboratory (VDRL)-positive CSF.
Treatment of syphilitic interstitial keratitis includes antibiotic therapy for untreated syphilis cases. Parenteral penicillin is the drug of choice for all stages of syphilis. T pallidum is extremely sensitive to penicillin. T pallidum resistance to penicillin has not surfaced. The need for alternative drugs in treating syphilis is reserved for penicillin-allergic cases.
Doxycycline, erythromycin, or tetracycline has been suggested for patients allergic to penicillin. Nonpenicillin regimen has been shown to be less effective in the treatment of neurosyphilis; therefore, attempts at penicillin desensitization may be worthwhile.
Treatment of neurosyphilis
According to the Centers for Disease Control and Prevention, the treatment of neurosyphilis is intravenous aqueous crystalline penicillin G 2-4 million U IV q4h for 10-14 days. [3] If outpatient therapy is preferred, give procaine penicillin intramuscularly (IM) every day plus probenecid, 500 mg orally 4 times daily, both for 10-14 days.
Treatment of syphilis in pregnancy
The penicillin treatment regimen is appropriate for pregnant patients with syphilis. The optimal treatment of penicillin-allergic pregnant patients is controversial. Penicillin skin testing, and, if necessary, desensitization are recommended. An alternate therapy is erythromycin. Avoid doxycycline because of its potential adverse effects on both the mother and the fetus.
Treatment of syphilis in infants and children
Treatment of infants is indicated in the following circumstances:
-
The mother has untreated syphilis
-
The infant has clinical syphilis
-
The infant’s VDRL or RPR result is 4 times that of the mother
-
The infant has a reactive CSF VDRL test or positive FTA-ABS immunoglobulin M test
Evaluate infants for congenital syphilis when the mother has been treated for syphilis prior to pregnancy.
Perform a nontreponemal serologic test on the infant's sera and a CSF test for cells, protein, and VDRL. Perform an antitreponemal testing on the infant and cord or placenta. Perform long bone radiographs and other tests, as clinically indicated.
Suspect child abuse and/or molestation in a pediatric patient exhibiting primary syphilitic lesions.
Treatment of syphilis in HIV-infected patients
Treat syphilis in patients who are infected with HIV aggressively with a course sufficient for neurosyphilis, regardless of the CNS examination. In most patients with HIV infection, serologic tests for syphilis are accurate, although there are reports of false-negative test results and delayed seroconversion. Anecdotal evidence suggests that patients infected with HIV are at an increased risk of developing neurosyphilis and have higher treatment failure rates. Do not standardize the treatment of patients who are infected with HIV.
Penicillin allergy
Penicillin is the preferred treatment for all types of syphilis. Penicillin allergy is not necessarily a contraindication to penicillin treatment. When challenged with penicillin, most individuals with a history of penicillin allergy do not manifest symptoms, or the symptoms are mild and affect the skin. Treatment guidelines recommend provocative testing and desensitization, if necessary.
Treatment of sexual partners
Partners of infected patients should be evaluated clinically and serologically. Partners of patients with primary, secondary, or latent syphilis should be treated presumptively if they have had sexual contact with the patient within the preceding 90 days.
One third of persons so exposed will contract syphilis in 10-90 days. If the 90-day period has elapsed and the partner is reliable, treatment can be dictated by the clinical and serologic evaluation. Presumptive treatment is warranted if follow-up care is in doubt.
Treatment of tuberculosis
Tuberculous interstitial keratitis also responds well to topical corticosteroid treatment. Systemic therapy is indicated using the recommended multidrug regimens.
Treatment of leprosy
For patients with lepromatous interstitial keratitis, in addition to systemic treatment using dapsone, clofazimine, and rifampin, local treatment with topical corticosteroids may be cautiously used owing to its potentially deleterious effect on the corneal epithelium and wound healing in patients with neurotrophic disease due to leprosy.
Treatment of Lyme disease
Treatment of Lyme disease includes the appropriate systemic antibiotic therapy, which is based on the stage of the illness. Topical anti-inflammatory medications (eg, corticosteroids) reduce the local morbidity, as in the other forms of interstitial keratitis.
Treatment of amoebic disease
Treatment of Acanthamoeba keratitis includes discontinuation of infected contact lenses, as well as using various antibiotic, antifungal, and antiparasitic topical and systemic medications. The medications may need to be continued for a significant length of time, and, typically, Acanthamoeba remains a very difficult infection to treat.
Treatment of parasitic disease
The various parasitic causes of interstitial keratitis are treated with systemic antiparasitic therapy. In cases of onchocerciasis, systemic treatment with ivermectin is the accepted standard of care.
Leishmania requires systemic treatment with sodium stibogluconate, or meglumine antimonate may be combined with the same medications topically to treat keratitis.
Treatment of interstitial keratitis due to trypanosomiasis is via the systemic antiprotozoal agents (eg, suramin, nifurtimox).
Treatment of Microsporidia
Microsporidia remains a very rare cause of interstitial keratitis, and treatment options vary from systemic antiparasitic agents to surgical reconstruction with penetrating keratoplasty.
Treatment of herpes simplex keratitis
Treatment of herpetic stromal disease has been described as part of the Herpetic Eye Disease Study (HEDS). Topical steroids were found to be beneficial when combined with topical antiviral agents in the treatment of herpetic stromal disease, but oral acyclovir was not found to have any additional benefit when combined with topical corticosteroids and topical antiviral agents (eg, trifluridine). Oral acyclovir does appear to reduce the likelihood of recurrent herpetic disease.
Treatment of neurotrophic keratitis in association with interstitial keratitis
Neurotrophic keratitis is a degenerative disease resulting from a reduction in corneal sensation. This loss of corneal sensation impairs corneal health causing progressive damage to the top layer of the cornea and can rarely produce an interstitial keratitis. The FDA has recently approved the first drug for the treatment of neurotrophic keratitis, an eye drop containing cenegermin with the trade name of Oxervate.
Surgical treatment
In cases of permanent corneal opacity of any etiology, corneal transplantation is an option for visual rehabilitation, but it should be performed only when the ocular inflammation has become quiescent to prevent postoperative complications, such as rejection and graft failure.
Consultations
Collaboration with an infectious disease specialist is ideal in cases of suggestive of syphilis or suspected parasitic keratitis. An allergy consult may be warranted in cases of penicillin allergy. Rheumatologic and ear, nose, and throat (ENT) consultations should be obtained in suspected cases of Cogan syndrome, especially in patients with a history of systemic vasculitides. Both an obstetrician and a pediatric infectious disease specialist should be invited into the management team of a pregnant patient with syphilis.
Further inpatient care
Following treatment of ocular syphilis, monitor serologic titers for evidence of response or treatment failure. A 4-fold decrease in antibody titers should be evident. The decline in antibody titers is slower in late latent and neurosyphilis.
Further outpatient care
Topical steroids are tapered slowly in patients with interstitial keratitis, over weeks to months, depending on the clinical response.
In patients with syphilis, repeat serum and cerebrospinal fluid (CSF) Venereal Disease Research Laboratory (VDRL) titers to monitor adequacy of treatment. Clinical manifestations often improve after effective treatment. Seroconversion or stable low titers of nontreponemal tests also indicate effective treatment. A 4-fold and 8-fold decrease in nontreponemal titers should occur in 3 and 6 months, respectively.
Patients with neurosyphilis should be monitored with CSF examination every 6 months for decreasing cell count. If no decrease occurs in 6 months, or if the cell count does not return to normal in 2 years, retreatment should be considered.
Complications
Complications related to interstitial keratitis generally are due to corneal thinning and perforation. Although these occur rarely, perforations of the cornea may be treated urgently with conventional penetrating keratoplasty.
The Jarisch-Herxheimer reaction is the release of endotoxin when a large number of organisms are killed by antibiotics. The Jarisch-Herxheimer reaction is not a dose-related phenomenon; administering a smaller dose is of no value.
This reaction occurs about 8 hours after the first injection of antibiotic; usually consists of mild fever, malaise, and headache; and lasts a few hours. It occurs in 50% of patients with primary syphilis and in 90% of patients with secondary syphilis; it is rarely seen in quaternary syphilis, a disease beyond the immune tertiary stage, which, owing to suppressed immunity, such as in coexistent HIV infection, becomes an organism-laden stage of fulminant anergic necrotizing encephalitis.
Prognosis
With appropriate treatment, visual acuity in interstitial keratitis generally can be preserved. In case of permanent corneal scarring, surgical therapy often is successful provided that the underlying cause of inflammation is controlled.
Ocular syphilis, if clinically diagnosed and appropriately treated early in its course, usually results in full visual recovery. If syphilitic intraocular inflammation is left untreated, chronic progressive intraocular inflammation may ensue. Inflammation leads to secondary glaucoma, chronic vitritis, retinal necrosis, and optic atrophy.
Patient Education
For patient education information, see the Sexually Transmitted Diseases Center and Eye and Vision Center, as well as Sexually Transmitted Diseases, Syphilis, Anatomy of the Eye, and Iritis.
Advise patients to practice safe sex. Advise patients against sharing needles. Encourage patients to consider premarital and perinatal screenings.
-
This photograph depicts a child with a bilateral eye condition known as interstitial keratitis (IK), a stigma related to congenital syphilis.
-
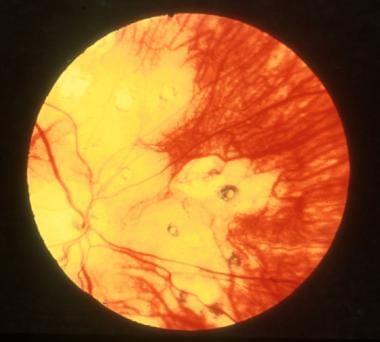
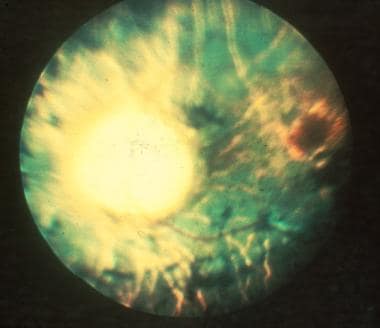
Interstitial keratitis in a patient with ocular syphilis.
-
Interstitial keratitis in a patient with ocular syphilis.
-
Syphilis chorioretinitis in a 30-year-old patient with intellectual disability.
-
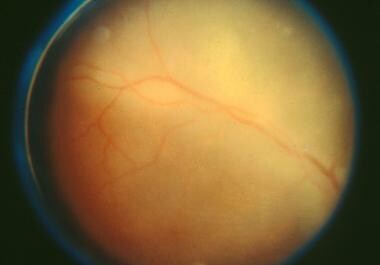
A 73-year-old woman with syphilis. Note the optic atrophy, arteriolar narrowing, pigment loss, and clumping.
-
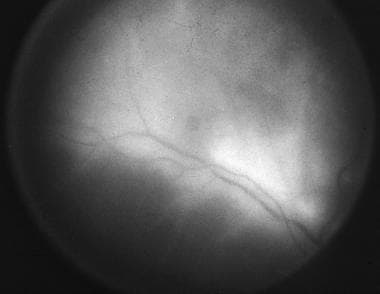
Retinal vasculitis in a patient with ocular syphilis.
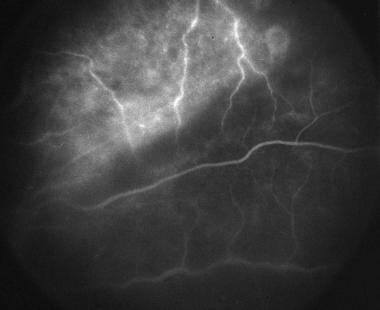
-
Fluorescein angiography of same patient as above demonstrating active retinal vasculitis.
-
Chorioretinitis of ocular syphilis.
-
Active retinal vasculitis of ocular syphilis as seen on fluorescein angiography.