Background
Purtscher retinopathy is a hemorrhagic and vasoocclusive vasculopathy, which, in 1912, was first described as a syndrome of sudden blindness associated with severe head trauma. These patients had findings of multiple white retinal patches and retinal hemorrhages that were associated with severe vision loss. [1, 2, 3]
Since its original description, Purtscher retinopathy has been associated with traumatic injury, primarily blunt thoracic trauma and head trauma, and numerous nontraumatic diseases.
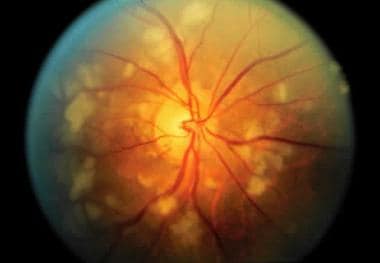 Characteristic fundus findings of Purtscher retinopathy. Multiple cotton-wool spots surround the optic nerve after blunt thoracic trauma.
Characteristic fundus findings of Purtscher retinopathy. Multiple cotton-wool spots surround the optic nerve after blunt thoracic trauma.
Purtscher-like retinopathy is seen in diverse conditions, including acute pancreatitis; fat embolization; amniotic fluid embolization; preeclampsia; hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome; and vasculitic diseases, such as lupus.
Pathophysiology
The original findings of white lesions in the retina associated with intraretinal and preretinal hemorrhages and papillitis were believed to be caused by lymphatic extravasation from trauma. These lesions are known as Purtscher flecken (larger infarcts of the retinal capillary bed) and cotton-wool spots (small retinal microinfarcts at the level of the nerve fiber layer). Fluorescein leakage in Purtscher retinopathy suggests that an acute endothelial cell injury is caused by trauma, possibly predisposing the retinal vessels to occlusion. [4, 5, 6]
The exact pathophysiology remains somewhat controversial, and different mechanisms have been proposed. The condition has been associated with various vasculopathies, including cryoglobulinemia, iron-deficiency anemia, thrombotic thrombocytopenic purpura, and drug-induced hypersensitivity, among others. [7, 8, 9, 10]
The most accepted mechanism is leukoembolization that causes arterial occlusion and infarction of the microvascular bed. Leukocyte aggregation, which is induced by complement C5a, is believed to be the most likely mechanism of embolization because of its known association with trauma, acute pancreatitis, and vasculitic diseases. Recent OCT findings in cases of Purtscher-like retinopathy also support the microembolization hypothesis.
Other possible sources of emboli include fat emboli in cases of long bone fractures and perhaps pancreatitis from enzymatic digestion of omental fat, amniotic fluid embolization during childbirth and postpartum, air emboli from traumatic chest compression, and granulocyte aggregation resulting from complement activation.
Other proposed mechanisms of vascular occlusion include angiospasm resulting from an acute rise in venous pressure from compressive chest injuries or possibly acute head injuries and endothelial cell damage resulting from acutely increased intraluminal pressure. A recent paper modeling shear stress in the retina suggests that Purtscher retinopathy may be a rheological event at a retinal posterior pole foci of vascular endothelial dysregulation, followed by downstream endothelin-induced vasculopathy. [11]
Epidemiology
Frequency
United States
Not reported
International
Not reported
Mortality/Morbidity
Bilateral manifestations are seen most commonly, but unilateral findings have been reported.
Decreased vision occurs in the affected eyes, generally in the range of 20/200 to counting fingers. Vision often improves over several months to a range of 20/30 to 20/200, depending on the severity of the retinal findings. Case reports of Purtscher retinopathy associated with preeclampsia have demonstrated poor visual outcomes in more than one half of these patients. [12]
Race
Not reported
Sex
Not reported
Age
Not reported
Prognosis
Visual prognosis is guarded, although initially decreased vision may improve over a period of months. [13]
The most important prognostic finding that is associated with a poor visual prognosis is central macular infarction.
Patient Education
Educate patients regarding the mandatory use of seat belts in cases of blunt trauma.
-
Characteristic fundus findings of Purtscher retinopathy. Multiple cotton-wool spots surround the optic nerve after blunt thoracic trauma.
-
Mild Purtscher retinopathy in a patient after blunt chest compression as an unrestrained driver in a motor vehicle accident. This patient presented with visual loss in the left eye and had unilateral disease. The fundus photograph shows a large cotton-wool spot along the inferotemporal arcade and more subtle microvascular injury between the disc and fovea in the central macula. Whitening of the central fovea is present. Visual acuity was 20/200 but returned to 20/30 after 6 weeks.
-
Fluorescein angiogram of a patient who sustained blunt chest compression as an unrestrained driver in a motor vehicle accident shows focal microvascular occlusion in the area of the cotton-wool spot. Mild venous leakage and staining is seen in the perifoveal capillary bed just beneath the central fovea. A small amount of fluorescein leakage is also seen beneath the fovea.
-
Purtscher-like retinopathy in a patient with systemic lupus erythematosus with microvascular encephalopathy and retinopathy. Multiple cotton-wool spots of varying sizes and ages surround the optic nerve. A branch arterial occlusion is present along the supertemporal arcade with retinal whitening between the major artery and vein. Multiple occlusions are seen in arterial and venous trees with disruption of the blood columns.
-
Patient perception of visual deficits in an eye with Purtscher retinopathy






