Overview
Before the advent of modern neuroimaging, EEG was the best noninvasive tool to use in searching for focal lesions. In the last few decades, with progress in imaging techniques, the role of EEG is changing; its use for localization of a brain lesion is being superseded by neuroimaging. The use of EEG outside of epilepsy has declined markedly.
The use of EEG in monitoring brain activity in the operating room and also in intensive care settings needs to be redefined and its utility reassessed. In clinical situations in which the primary question is the electrical functioning of the brain and not primarily localization, EEG remains a necessary test. EEGs are performed routinely in various clinical situations; therefore, the neurophysiologist is expected to be familiar with the EEG findings even in situations in which they are of relatively limited value.
Like most neurophysiologic tests, EEG is a test of cerebral function; hence, for the most part it is nonspecific as to etiology. Although at one time authors discussed the application of EEG in differentiating various types of lesions, this clearly has not been clinically useful in the modern era. The exercise of describing EEG abnormalities by pathology (eg, stroke, abscess, tumor, even various types of tumors), which was common in old EEG texts, is therefore not followed here. Instead, the different patterns of focal (nonepileptic) disturbances of brain function and their clinical significance are reviewed.
Waveform Descriptions
Slow activity
Abnormal slow activity is by far the most common EEG manifestation of focal brain dysfunction. The abnormality that correlates best with the presence of a structural lesion is polymorphic or arrhythmic (as opposed to monomorphic or rhythmic) delta (ie, 1-3 Hz) slowing. This is all the more reliable when it is continuous, unreactive (ie, characterized by lack of change between states, such as wake or sleep, or in response to external stimuli), of high amplitude, polymorphic, and unilateral. The localization of slow potentials follows the same rules as that of epileptiform discharges. Thus, "phase reversals" are useful to localize slow potentials and do not imply abnormality or epileptogenicity.
Amplitude asymmetry
In the classification used here, the term asymmetry refers to asymmetry of amplitude and to normal rhythms. By contrast, a focal frequency asymmetry would be classified as focal slow. [1] Finally, readers should keep in mind that amplitude asymmetries should be evaluated on referential montages, since amplitude is highly dependent on interelectrode distances.
Periodic lateralized epileptiform discharges
Described in 1964 by Chatrian et al, periodic lateralized epileptiform discharges (PLEDS) are a special type of focal abnormality. [2, 3] As implied by their name, they are periodic, lateralized, and epileptiform. Periodicity is the most characteristic feature, and the one that sets PLEDS apart from other focal abnormalities. Periodicity refers to a relatively constant interval between discharges, which varies between 0.5 and 3 seconds and most often is around 1 second. The epileptiform morphology of the discharges is not invariable, as PLEDS are often closer to slow waves than to sharp waves in morphology.
Clinical Correlation
Slow activity
Continuous focal slow activity is the only nonepileptiform focal abnormality that can be interpreted unequivocally as abnormal when it is an isolated finding. Other focal abnormalities are quite frequent but are of such low specificity that they almost never constitute an abnormality in themselves. To be interpreted as abnormal, these usually require the coexistence of a more definite abnormality such as slowing or epileptiform discharges.
As already outlined, focal slowing is nonspecific as to etiology, and in the era of neuroimaging the EEG has no role in diagnosing the nature of a lesion. Focal slowing is the most common abnormality associated with focal lesions of any type, including (but not limited to) neoplastic, vascular, subdural collections, traumatic, and infectious (see images below). It occasionally may be seen even in more subtle structural abnormalities such as mesiotemporal sclerosis or focal malformations of cortical development.
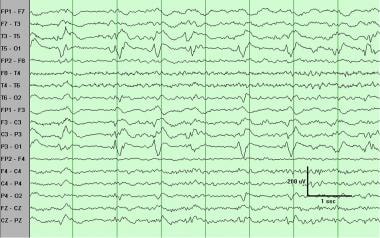
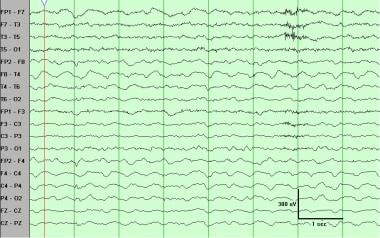 Continuous slow, lateralized right hemisphere. While "spilling over" to the left frontal region, the polymorphic delta activity is clearly predominant over the right hemisphere. This type of slowing almost invariably is associated with a structural hemispheric lesion. This patient had a large right middle cerebral artery infarct.
Continuous slow, lateralized right hemisphere. While "spilling over" to the left frontal region, the polymorphic delta activity is clearly predominant over the right hemisphere. This type of slowing almost invariably is associated with a structural hemispheric lesion. This patient had a large right middle cerebral artery infarct.
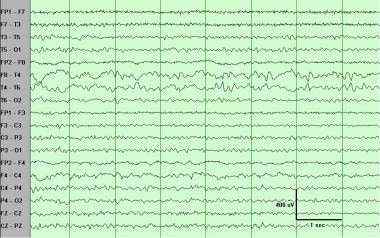
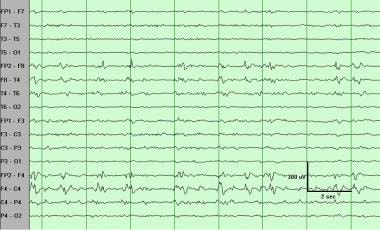
 Continuous slow, lateralized left hemisphere. This polymorphic delta activity was continuous throughout the record. This patient had a left hemisphere neoplasm.
Continuous slow, lateralized left hemisphere. This polymorphic delta activity was continuous throughout the record. This patient had a left hemisphere neoplasm.
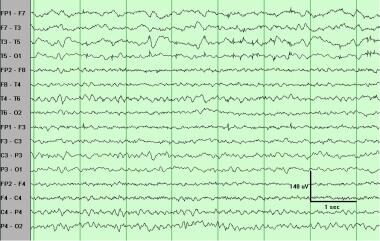
 Continuous slow, regional right temporal. This polymorphic delta activity is somewhat more focal than that shown in the first image above, with a maximum in the temporal chain. Little such activity is evident in the central chain, but enough to exclude a T4 electrode artifact. The slowing shows phase reversals at T4, indicating a maximum at that electrode.
Continuous slow, regional right temporal. This polymorphic delta activity is somewhat more focal than that shown in the first image above, with a maximum in the temporal chain. Little such activity is evident in the central chain, but enough to exclude a T4 electrode artifact. The slowing shows phase reversals at T4, indicating a maximum at that electrode.
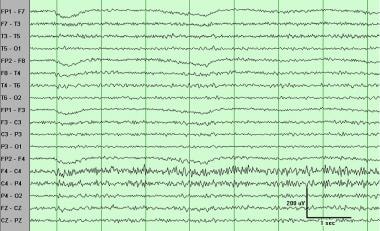
 Continuous slow, regional left temporal. This polymorphic delta activity is somewhat more focal than that in the second image above, with a maximum in the temporal chain. The phase reversals at T3 indicate a maximum at that electrode.
Continuous slow, regional left temporal. This polymorphic delta activity is somewhat more focal than that in the second image above, with a maximum in the temporal chain. The phase reversals at T3 indicate a maximum at that electrode.
The physiologic basis for focal polymorphic delta activity caused by focal cortical lesions is not fully understood. It is probably due to abnormalities in the underlying white matter rather than the cortex itself. When present, focal slow activity correlates highly with the side of the lesion, but it is not reliable for lobar localization. The likelihood of a structural lesion (ie, specificity) diminishes when the slow activity lacks these characteristics and is intermittent (see image below), in the theta rather than the delta range, and of low amplitude. This type of slowing may be normal (eg, temporal slowing of the elderly; see the article Normal EEG Variants). This is essentially the difference between focal "continuous slow" and "intermittent slow." [1]
 Intermittent slow, lateralized left hemisphere. This brief burst of delta activity is seen in the temporal and central areas. This is a much "weaker" finding than continuous slowing, and much less reliably associated with a structural lesion. This is indicative of mild dysfunction in that region.
Intermittent slow, lateralized left hemisphere. This brief burst of delta activity is seen in the temporal and central areas. This is a much "weaker" finding than continuous slowing, and much less reliably associated with a structural lesion. This is indicative of mild dysfunction in that region.
In a few situations in clinical neurology, the EEG may show clear evidence of focal dysfunction (ie, focal slow) while no structural abnormality is found. The typical cases in point are the focal epilepsies. A readily demonstrable structural lesion usually is not found on neuroimaging, typically MRI (see Localization-Related Epilepsies on EEG).
Focal brain dysfunction without structural abnormalities has been observed in transient ischemic attacks (TIA), migraine, and postictal states. Polymorphic delta activity in these cases may be indistinguishable from that caused by a structural lesion, except that it is short-lived (ie, it disappears over time). The postictal state is the most common cause of nonstructural polymorphic delta activity, but the activity disappears within minutes to hours after the ictal event. Patients with ongoing TIAs or migraine rarely undergo an EEG during the symptomatic period, so clinical data are scarce.
Amplitude asymmetry
Destructive lesions clearly can attenuate the amplitude of normal rhythms. However, normal rhythms are never perfectly symmetric in amplitude, therefore which asymmetries to consider significant is not always clear. (Some have proposed a greater than 50% side-to-side difference as abnormal.)
A good rule of thumb is that, with very few exceptions, significant focal asymmetries are associated with slowing. The authors recommend that any amplitude asymmetry associated with slowing of frequency be considered significant.
Amplitude asymmetry or suppression of normal rhythms is somewhat more likely to be seen in structural abnormalities that increase the distance or interfere with the conduction of the electrical signal between the cortex and the recording scalp electrodes. Examples include subdural collections (eg, hematoma, empyema), epidural collections (eg, hematoma, abscess), subgaleal collections, and calcifications such as those seen in Sturge-Weber syndrome.
Amplitude asymmetry also may be more common than slowing in subdural hematomas. However, caution must be exercised before considering isolated nonepileptiform focal findings other than slowing as abnormal. In general, as with other types of focal EEG abnormalities such as slowing, amplitude asymmetry is nonspecific as to etiology.
Although asymmetry in amplitude is usually indicative of dysfunction on the side of depressed amplitude, one notable exception to this rule is the so-called breach rhythm (see image below). This is caused by a skull defect, which attenuates the high-frequency filter function of the intact skull. As a result, faster frequencies (eg, alpha, spindles, beta) are of higher amplitude on the side of the defect. Since morphology often is sharply contoured, determining the epileptogenicity of these discharges can be extremely difficult, and in this situation erring on the conservative side, by not interpreting them as epileptiform, is clearly preferable. Because of a cancellation effect between frontopolar (Fp1/Fp2) and frontal (F3/F4), eye movements often are not increased on the side of a skull defect and may indeed be of lesser amplitude on that side.
 Asymmetry, increased beta, regional right frontocentral. The beta activity is increased in amplitude in the right frontocentral region. This is a "breach rhythm" and is caused most often by a skull defect (in this case a burr hole).
Asymmetry, increased beta, regional right frontocentral. The beta activity is increased in amplitude in the right frontocentral region. This is a "breach rhythm" and is caused most often by a skull defect (in this case a burr hole).
Periodic lateralized epileptiform discharges
PLEDS are caused by acute destructive focal lesions and are a transitory phenomenon: they tend to disappear in weeks, even if the causal lesion persists. [4] Over time, the record takes on a less specific focal slow appearance, which is more likely to persist. By far the most common etiology is an acute cerebrovascular event [5] ; second most common is focal encephalitis such as that caused by herpes. In a clinical context suggestive of viral encephalitis, the EEG can be of great value for diagnosis and can guide tissue biopsy. Though most often associated with an acute destructive lesion, PLEDS, like other EEG findings, are not specific as to etiology and have been described in almost all types of structural lesions, including subdural hematoma and chronic lesions, especially in the presence of a superimposed systemic disturbance. [6]
In keeping with their epileptiform morphology, PLEDS have a close association with clinical seizures, and on average about 80% of patients with PLEDS have clinical seizures.
 Periodic lateralized epileptiform discharges (PLEDS), regional left centrotemporal. The repetitive discharges occur with a periodicity of about 1 second. Polymorphic delta activity is seen over the left hemisphere, but the classification as PLEDS already implies severe focal dysfunction. In addition, it indicates an acute destructive process and very high (80%) risk of seizures.
Periodic lateralized epileptiform discharges (PLEDS), regional left centrotemporal. The repetitive discharges occur with a periodicity of about 1 second. Polymorphic delta activity is seen over the left hemisphere, but the classification as PLEDS already implies severe focal dysfunction. In addition, it indicates an acute destructive process and very high (80%) risk of seizures.
 Periodic lateralized epileptiform discharges (PLEDS), lateralized right hemisphere. The repetitive discharges occur with a periodicity of 2-4 seconds. PLEDS are associated with severe focal dysfunction and with acute destructive processes and very high (80%) risk of seizures.
Periodic lateralized epileptiform discharges (PLEDS), lateralized right hemisphere. The repetitive discharges occur with a periodicity of 2-4 seconds. PLEDS are associated with severe focal dysfunction and with acute destructive processes and very high (80%) risk of seizures.
The transition between PLEDS and a clear ictal seizure pattern is very gradual, illustrating the hypothesis that PLEDS may represent a subclinical ictal pattern. In clinical practice, however, PLEDS usually are managed as interictal discharges (ie, spikes or sharp waves). They indicate a high risk for focal seizures, [7] but usually are not treated with antiepileptic drugs unless clinical evidence for seizures is noted. This position is endorsed by the authors and others. This is somewhat controversial, however, and some advocate antiepileptic treatment in all patients with PLEDS.
Periodic patterns in Creutzfeldt-Jakob disease usually are generalized and bisynchronous but occasionally, especially early in the course, they may be unilateral or markedly asymmetric, and thus take on the appearance of PLEDS. [8]
Other less common focal patterns
An abnormal response to photic stimulation can be seen in focal lesions. Normal photic driving has long been known to be potentially reduced on the side of a lesion. Posterior destructive lesions are particularly likely to attenuate the driving response, but some reports have described an enhanced photic response on the side of dysfunction. However, since the normal driving response can be quite asymmetric, such a finding should be accompanied by a more reliable abnormality such as slowing of the waveform frequency in order to be interpreted as abnormal.
The Bancaud phenomenon refers to the unilateral loss of reactivity of a normal rhythm and initially was described in the context of the alpha rhythm. It should be considered a pathological finding only when associated with other more definite abnormalities, such as slowing.
Questions & Answers
Overview
What is the role of EEG in focal lesion imaging?
What is abnormal slow activity on EEG of focal lesions?
What is amplitude asymmetry on EEG of focal lesions?
What are periodic lateralized epileptiform discharges on EEG of focal lesions?
How is an EEG finding of slow activity interpreted?
How is an EEG finding of amplitude asymmetry interpreted?
How is an EEG finding of periodic lateralized epileptiform interpreted?
What are less common focal patterns on EEG?
-
Continuous slow, lateralized right hemisphere. While "spilling over" to the left frontal region, the polymorphic delta activity is clearly predominant over the right hemisphere. This type of slowing almost invariably is associated with a structural hemispheric lesion. This patient had a large right middle cerebral artery infarct.
-
Continuous slow, lateralized left hemisphere. This polymorphic delta activity was continuous throughout the record. This patient had a left hemisphere neoplasm.
-
Continuous slow, regional right temporal. This polymorphic delta activity is somewhat more focal than that shown in the first image above, with a maximum in the temporal chain. Little such activity is evident in the central chain, but enough to exclude a T4 electrode artifact. The slowing shows phase reversals at T4, indicating a maximum at that electrode.
-
Continuous slow, regional left temporal. This polymorphic delta activity is somewhat more focal than that in the second image above, with a maximum in the temporal chain. The phase reversals at T3 indicate a maximum at that electrode.
-
Intermittent slow, lateralized left hemisphere. This brief burst of delta activity is seen in the temporal and central areas. This is a much "weaker" finding than continuous slowing, and much less reliably associated with a structural lesion. This is indicative of mild dysfunction in that region.
-
Asymmetry, increased beta, regional right frontocentral. The beta activity is increased in amplitude in the right frontocentral region. This is a "breach rhythm" and is caused most often by a skull defect (in this case a burr hole).
-
Periodic lateralized epileptiform discharges (PLEDS), regional left centrotemporal. The repetitive discharges occur with a periodicity of about 1 second. Polymorphic delta activity is seen over the left hemisphere, but the classification as PLEDS already implies severe focal dysfunction. In addition, it indicates an acute destructive process and very high (80%) risk of seizures.
-
Periodic lateralized epileptiform discharges (PLEDS), lateralized right hemisphere. The repetitive discharges occur with a periodicity of 2-4 seconds. PLEDS are associated with severe focal dysfunction and with acute destructive processes and very high (80%) risk of seizures.









