Overview
With the introduction of highly active antiretroviral therapy (HAART), vacuolar myelopathy (VM) has become rarer, but it remains the most common chronic myelopathy associated with HIV. VM occurs during the late stages of AIDS, when CD4+ lymphocyte counts are very low, often in conjunction with AIDS dementia complex, peripheral neuropathies, and opportunistic infections or malignancies of the central or peripheral nervous system (eg, cytomegalovirus, progressive multifocal leukoencephalopathy, lymphoma).
For patient education information, see the Immune System Center, Dementia Center, and Sexually Transmitted Diseases Center, as well as Dementia Due to HIV Infection and HIV/AIDS.
Pathophysiology
Several hypotheses have been proposed to explain the development of vacuolar myelopathy (VM). One hypothesis is infiltration by HIV-infected mononuclear cells that secrete neurotoxic factors, including cytokines, possibly in conjunction with neurotoxic astrocyte factors. Transgenic mice that express HIV gene products in oligodendrocytes develop clinical and histologic features that resemble the human disease. [1] Although direct HIV infection of astrocytes and neurons is reported in the brain and dorsal root ganglia, it is not a major feature in VM. Impaired utilization of vitamin B-12 as a source of methionine in transmethylation metabolism for myelin maintenance in the spinal cord may be a contributing factor. [2]
Epidemiology and Prognosis
Before the introduction of highly active antiretroviral therapy (HAART), vacuolar myelopathy (VM) occurred in 5–20% of adult HIV patients in clinical studies and in 25–55% of adult HIV patients in histologic studies. Since its introduction, fewer than 10% of AIDS patients develop VM.
The prognosis of VM is poor. Most patients die within 6 months of onset.
Clinical Presentation
Vacuolar myelopathy (VM) typically presents as a posterolateral spinal cord syndrome often limited to the thoracic cord. It manifests as a slowly progressive, painless spastic paraperesis with sensory loss, imbalance, and sphincter dysfunction. Relapsing-remitting courses have been described. [3]
Back pain is not prominent. Arm function is usually normal except for advanced cases.
VM is often associated with AIDS dementia complex and peripheral neuropathy. In such cases, patients have cognitive decline and distal limb pain and numbness.
Physical examination
The following may be noted:
-
Slowly progressive spastic paraparesis; signs and symptoms may be asymmetric early on
-
Hyperreflexia and extensor plantar responses
-
Dorsal column-type sensory loss
-
Ataxic gait
-
Incontinence
-
Erectile dysfunction may be an early sign
-
Rare involvement of upper extremities
A discrete sensory level is usually absent; if present, this strongly suggests other causes of myelopathy.
Diagnostic Considerations
Other problems to be considered in the differential diagnosis of HIV-related VM include the following:
-
HIV-associated transverse myelitis during seroconversion [4]
-
Herpes simplex (HSV) or zoster (VZV) virus infection
-
Cytomegalovirus (CMV) infection
-
Neurosyphilis
-
Cervical disk syndromes
-
Other HIV-associated conditions (eg, Kaposi sarcoma, lymphoma, toxoplasmosis) in the spinal canal
-
Mycobacterium tuberculosis infection
-
Compressive myelopathy (eg, tumor, abscess, herniated disc, arteriovenous malformation)
-
Human T-cell lymphotropic virus type 1 (HTLV-1/2)–associated myelopathy/tropical spastic paraparesis (can co-exist with HIV infection)
-
Spinal epidural abscess in HIV-infected parenteral drug users
-
Multiple sclerosis
-
Vitamin B-12 deficiency
-
Copper deficiency
Diagnostic Tests
Electrophysiologic tests can support a diagnosis of vacuolar myelopathy (VM). Somatosensory evoked potential (SSEP) may be a valuable tool in the diagnosis, particularly when myelopathy and peripheral neuropathy coexist. [5]
Other studies serve to identify or rule out other potential causes of myelopathy. CSF analysis can exclude infection with cytomegalovirus(CMV), varicella-zoster virus (VZV), herpes simplex virus (HSV), and HTLV-1 and 2. CSF results are usually normal in HIV-associated VM.
Serum studies candetermine B-12 and folate levels. In patients with borderline low B-12, elevated homocysteine and methylmalonic acid levels are better indicators of a deficiency. B-12 levels are usually normal in vacuolar myelopathy.
A Schilling test, hematologic studies, and CD4+ lymphocyte counts may be indicated.
CT imaging
CT scan results are often noncontributory but may reveal unsuspected coexisting conditions such as extra or intramedullary infections, neoplasms, degenerative disk or joint disease of the spine.
Magnetic Resonance Imaging
MRI scans serve two purposes.
- Like CT, to rule out alternative or coexisting conditions.
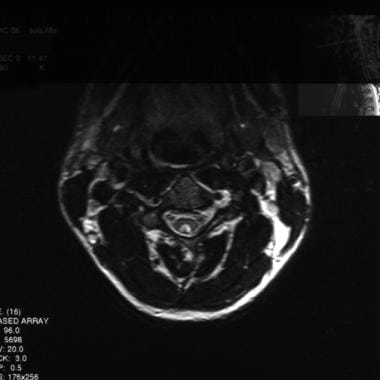
- Variably, MRI reveals abnormalities more specific to VM, ie, atrophy (most common) of the thoracic cord with or without cervical cord involvement. T2-weighted images often show symmetric non-enhancing high-signal areas present on multiple contiguous slices, usually symmetrical; these result from extensive vacuolation (hence the name). [6, 7, 8] Lesions may be confined to the posterior columns, especially the gracile tracts, or be diffuse (see images below).
 High-intensity lesion in the C2-C5 posterior spinal cord on T2-weighted sagittal MRI consistent with HIV myelopathy.
High-intensity lesion in the C2-C5 posterior spinal cord on T2-weighted sagittal MRI consistent with HIV myelopathy.
Histologic Findings
Histologic findings may indicate multifocal, occasionally asymmetric vacuolation and myelin pallor involving the dorsal and lateral tracts more than the anterior and anterolateral tracts and involving the cervical and thoracic segments more than the lumbar segments or the brainstem, accompanied by astrogliosis. (See the images below.)
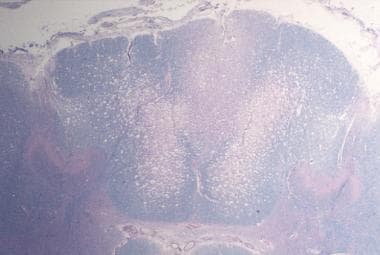 Spinal cord from patient with vacuolar myelopathy that shows extensive spongiform changes in the white matter (Luxol fast blue stain) (contributed by Dr. Beth Levy, Saint Louis University School of Medicine, St. Louis, MO).
Spinal cord from patient with vacuolar myelopathy that shows extensive spongiform changes in the white matter (Luxol fast blue stain) (contributed by Dr. Beth Levy, Saint Louis University School of Medicine, St. Louis, MO).
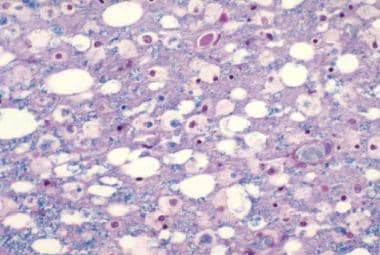 Marked vacuolation is apparent in this Luxol fast blue stained photomicrograph (contributed by Dr. Beth Levy, Saint Louis University School of Medicine, St. Louis, MO).
Marked vacuolation is apparent in this Luxol fast blue stained photomicrograph (contributed by Dr. Beth Levy, Saint Louis University School of Medicine, St. Louis, MO).
HIV-infected, activated, lipid-laden macrophages and microglia expressing interleukin-1 and/or tumor necrosis factor-alpha may be seen. [9, 10] On electron microscopy, intramyelinic or periaxonal vacuoles and, rarely, disrupted axons may be seen.
The histology resembles subacute combined degeneration from vitamin B-12 deficiency. [11]
Treatment & Management
Care for patients with HIV-associated vacuolar myelopathy (VM) is primarily supportive. Although no specific treatment is currently approved for this syndrome, viral control tailored to the individual patient's medical and viral history is important, as clinical and radiologic improvement with highly active retroviral therapy (HAART) have been described. [12, 13, 14, 5]
A pilot study showed improvement in patients treated with L-methionine. [15] However, a randomized, double-blind, placebo-controlled study of 56 patients showed no benefit. [16]
Symptomatic management relies on antispasmodics such as baclofen or tizanidine and intramuscular botulinum toxin to manage spasticity, pain management, and anticholinergic drugs to improve bladder function. [17]
Refer the patient to a physical medicine specialist for spinal cord treatment and follow-up care.
Questions & Answers
Overview
What is HIV-associated vacuolar myelopathy (VM)?
What is the pathophysiology of HIV-associated vacuolar myelopathy (VM)?
What is the prevalence of HIV-associated vacuolar myelopathy (VM)?
What is the prognosis of HIV-associated vacuolar myelopathy (VM)?
Which clinical history findings are characteristic of HIV-associated vacuolar myelopathy (VM)?
Which physical findings are characteristic of HIV-associated vacuolar myelopathy (VM)?
Which diagnostic tests are performed in the workup of HIV-associated vacuolar myelopathy (VM)?
What is the role of CT imaging in the workup of HIV-associated vacuolar myelopathy (VM)?
What is the role of MRI in the workup of HIV-associated vacuolar myelopathy (VM)?
Which histologic findings are characteristic of HIV-associated vacuolar myelopathy (VM)?
How is HIV-associated vacuolar myelopathy (VM) treated?
-
Spinal cord from patient with vacuolar myelopathy that shows extensive spongiform changes in the white matter (Luxol fast blue stain) (contributed by Dr. Beth Levy, Saint Louis University School of Medicine, St. Louis, MO).
-
Marked vacuolation is apparent in this Luxol fast blue stained photomicrograph (contributed by Dr. Beth Levy, Saint Louis University School of Medicine, St. Louis, MO).
-
High-intensity lesion in the C2-C5 posterior spinal cord on T2-weighted sagittal MRI consistent with HIV myelopathy.
-
High-intensity lesion in the posterior cervical cord on T2-weighted axial MRI consistent with HIV myelopathy.