Background
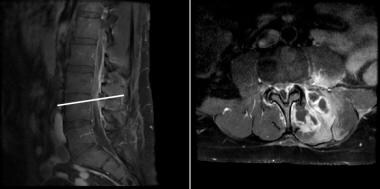
A spinal epidural abscess (see image below) is a loculated purulent collection that may cause spinal cord injury via compression or vascular compromise (thrombophlebitis). If left untreated, an expanding suppurative infection in the spinal epidural space can impinge upon the spinal cord, producing sensory symptoms, weakness/motor dysfunction, and, ultimately, paralysis and even death. Frequently, diagnosis is delayed because the initial presentation are non-specific (ie, only nonspecific back pain without any "red flag" symptoms). Half of all cases of spinal epidural abscess are estimated to be misdiagnosed or have a delayed diagnosis. [1] Early identification and timely surgical intervention may result in improved outcomes and preservation of neurological function.
Pathophysiology
Risk factors for epidural spinal abscesses include intravenous drug use and immunosuppression from a variety of sources including HIV/AIDS and chronic steroid use as well as poorly controlled diabetes. Most commonly, hematogenous spread with seeding of the epidural space with bacteria is the most common mechanism via which spinal epidural abscesses form. Reported sources of infection are numerous and include bacterial endocarditis, infected indwelling catheters, urinary tract infection, peritoneal and retroperitoneal infections, and others. However, direct extension from nearby anatomic structures such as the vertebral bodies, intervertebral disk spaces, or psoas muscles can also give rise to an infection within the epidural space. In rare instances, infections can occur as a result of direct inoculation (eg, epidural steroid injections).
The anatomy of the spinal epidural space makes it conducive to harboring infections. Posteriorly, the epidural space contains fat, small arteries, and a rich venous plexus. Anteriorly, the epidural space is a potential space with the dura tightly adherent to the vertebral bodies and ligaments. As such, abscesses occur more frequently in the larger, more densely vascular posterior epidural space. Some series suggest that dorsal spinal epidural abscesses are much more likely to present with weakness and severe neurologic deficit than ventral spinal epidural abscesses. [2]
The more clinically significant effects of the epidural abscess may be from involvement of the vascular supply to the spinal cord and subsequent venous infarction rather than direct compression. The development of symptoms is the result of meningeal irritation from the infection, structural instability from local tissue and ligamentous destruction, and neurological symptoms arising as a consequence of spinal cord compression and hypoxia from vascular compromise due to thrombophlebitis.
Epidemiology
The incidence of spinal epidural abscess presenting to large tertiary care centers is estimated to be about 0.2-2.8 cases per 10,000 admissions. However, the incidence is suspected to be increasing in relation to an escalating rates of intravenous drug abuse (IVDU), with reported incidences as high as 5.1 cases per 10,000 admissions. [3] Although there is a reported male predominance, and higher prevalence in the fifth to seventh decade of life, a wide range of demographic distribution amongst all ages is seen, concordant with patients' risk factors. [4] Cervical spine epidural abscesses are less common than those found in the thoracic and lumbar spine, although the former is associated with a higher risk of morbidity and mortality. [5]
Staphylococcus aureus is the most commonly reported pathogen, [6] though many other bacteria have been implicated, including Staphylococcus and Pseudomonas species, Escherichia coli, Brucella, and Mycobacterium tuberculosis. Methicillin-resistant S. aureus (MRSA) is increasingly reported, particularly in patients with a history of MRSA abscesses, spinal surgery, or implanted devices. [7] Immunosuppressed patients may have infections from unusual bacterial or fungal organisms.
Prognosis
Prognosis in general is related to the duration of spinal cord dysfunction and the degree of cord impairment at the time of diagnosis. Patients who present with neurological deficits are more likely to have a prolonged hospital and rehabilitation course compared to those who present neurologically intact. Cervical and thoracic abscesses appear to carry an increased risk of worse morbidity and overall functional recovery when compared with lumbar abscesses.
Patient Education
For patient education resources, see the Infections Center and Brain and Nervous System Center.
-
Cervical epidural abscess with spinal cord compression and spinal cord edema.
-
Spinal epidural abscess lumbar area.
-
An MRI of the lumbar spine (T1-weighted, post-contrast) shows a spinal epidural abscess at the level of L3-L4, with an associated left paraspinal muscle abscess.