Practice Essentials
A goiter is an enlarged thyroid gland, and it may be diffuse or nodular. A goiter may extend into the retrosternal space, with or without substantial anterior enlargement. Because of the anatomic relationship of the thyroid gland to the trachea, larynx, superior and inferior laryngeal nerves, and esophagus, abnormal growth may cause a variety of compressive syndromes. Thyroid function may be normal (nontoxic goiter), [1] overactive (toxic goiter), or underactive (hypothyroid goiter). Initial screening for goiters should include thyroid-stimulating hormone (TSH).
In 1656, Thomas Wharton described the distinct nature of what he termed the thyroid gland, distinguishing it from the larynx, as this structure had been considered a laryngeal gland from the time of Andreas Vesalius in the 16th century. It was nearly 200 more years before the function of the thyroid was elucidated. The normal adult thyroid gland weighs 10-25 g and has 2 lobes connected by an isthmus. Nearly 50% of thyroid glands exhibit a pyramidal lobe arising from the center of the isthmus. Longitudinal dimensions of the lobes of the thyroid range up to 5 cm, as shown in the image below.
Signs and symptoms of goiters
A goiter may present in various ways, including the following:
-
Incidentally, as a swelling in the neck discovered by the patient or on routine physical examination
-
A finding on imaging studies performed for a related or unrelated medical evaluation
-
Local compression causing dysphagia, dyspnea, stridor, plethora, or hoarseness
-
Pain due to hemorrhage, inflammation, necrosis, or malignant transformation
-
Signs and symptoms of hyperthyroidism or hypothyroidism [2]
-
Thyroid cancer with or without metastases
Diagnosis of goiters
Initial screening should include TSH. Given the sensitive third-generation assays, in the absence of symptoms of hyperthyroidism or hypothyroidism, further testing is not required. An assessment of free thyroxine index or direct measurement of free thyroxine would be the next step in the evaluation.
Further laboratory testing is based on presentation and results of screening studies and may include thyroid antibodies (antithyroid peroxidase; formerly, the antimicrosomal antibodies and antithyroglobulin), thyroglobulin, sedimentation rate, and calcitonin in an individual at high risk for medullary carcinoma of the thyroid.
Ultrasonography can be used to establish and follow goiter size, consistency, and nodularity. [3] It can also be employed to localize nodules for ultrasonographically guided biopsy.
Computed tomography (CT) scanning is useful in determining the effect of the thyroid gland on nearby structures. It also may be helpful in the follow-up of patients with thyroid cancer that shows evidence of recurrence. Magnetic resonance imaging (MRI) has the same indications as CT scanning.
Fine-needle aspiration biopsy is employed for cytologic diagnosis. [4] Fine-needle aspiration of the thyroid is used to determine the cause of an enlarged gland. In general, the procedure is not used in the workup of autonomously functioning nodules.
Core biopsy, or large-needle biopsy, of the thyroid uses a larger-gauge needle, providing a fragment of tissue. This procedure also carries with it a higher morbidity than fine-needle aspiration biopsy. Core biopsy has the advantage of more complete sampling.
Management of goiters
Small benign euthyroid goiters do not require treatment. The effectiveness of medical treatment using thyroid hormone for benign goiters is controversial.
The size of a benign euthyroid goiter may be reduced with levothyroxine suppressive therapy. Moreover, treatment of hypothyroidism or hyperthyroidism often reduces the size of a goiter.
Goiters with primary thyroid malignancy require levothyroxine replacement after surgery and radioactive iodine ablation. Metastatic lesions to the thyroid gland require treatment of the primary malignancy. Granulomatous and infectious etiologies for goiter require specific treatment depending on the underlying cause.
Surgery is reserved for the following situations:
-
Large goiters with compression
-
Malignancy
-
When other forms of therapy are not practical or are ineffective
If it is practical, treat endemic goiters in iodine-deficient regions with iodine supplementation in the diet and avoidance of goitrogens. Treatment with iodine supplementation or levothyroxine may reduce goiter size. [5]
Pathophysiology
The thyroid gland is controlled by thyroid-stimulating hormone (TSH; also known as thyrotropin), secreted from the pituitary gland, which in turn is influenced by the thyrotropin-releasing hormone (TRH) from the hypothalamus. TSH permits growth, cellular differentiation, and thyroid hormone production and secretion by the thyroid gland. Thyrotropin acts on TSH receptors located on the thyroid gland. Thyroid hormones are synthesized from iodination of tyrosine. The iodine is transported from plasma into the thyroid cell via a sodium-iodide symporter. This is an active process resulting in an intracellular iodine level exceeding 20 times the plasma iodine level. This iodine transport activity is controlled by TSH. [6] Serum thyroid hormones levothyroxine and triiodothyronine feed back to the pituitary, regulating TSH production. Interference with this TRH-TSH thyroid hormone axis causes changes in the function and structure of the thyroid gland. Stimulation of the TSH receptors of the thyroid by TSH, TSH-receptor antibodies, or TSH receptor agonists, such as chorionic gonadotropin, may result in a diffuse goiter. When a small group of thyroid cells, inflammatory cells, or malignant cells metastatic to the thyroid is involved, a thyroid nodule may develop.
A deficiency in thyroid hormone synthesis or intake leads to increased TSH production. Increased TSH causes increased cellularity and hyperplasia of the thyroid gland in an attempt to normalize thyroid hormone levels. If this process is sustained, a goiter is established. Causes of thyroid hormone deficiency include inborn errors of thyroid hormone synthesis, iodine deficiency, [5] and goitrogens.
A goiter may result from a number of TSH receptor agonists. TSH receptor stimulators include TSH receptor antibodies, pituitary resistance to thyroid hormone, adenomas of the hypothalamus or pituitary gland, and tumors producing human chorionic gonadotropin.
Epidemiology
Frequency
United States
Autopsy studies suggest a frequency of greater than 50% for thyroid nodules; with high-resolution ultrasonography, the value approaches 40% of patients with nonthyroidal illness. In the Framingham study, ultrasonography revealed that 3% of men older than 60 years had thyroid nodules, while 36% of women aged 49-58 years had thyroid nodules. [7] In the United States, most goiters are due to autoimmune thyroiditis (ie, Hashimoto disease).
International
Worldwide, the most common cause of goiter is iodine deficiency. [5] It is estimated that goiters affect as many as 200 million of the 800 million people who have a diet deficient in iodine. In the Wickham study from the United Kingdom, 16% of the population had a goiter. [8]
In a German study, 635 people underwent ultrasonographic thyroid screening, as well as basal TSH measurement, during a preventive-health checkup. [3] Thyroid nodules were detected in 432 (68%) of the persons screened; in a previous German study, ultrasonographic screening of more than 90,000 people detected thyroid nodules in 33% of the normal population. The authors of the latter report attributed this difference to the fact that patients in their study were screened using 13 MHz ultrasonographic scanners, which were more sensitive than the 7.5 MHz scanners used in the previous study. According to the investigators, their results indicated that the question of routine iodine supplementation requires renewed attention.
The incidence of thyroid cancer has been rising worldwide. The reasons are unclear, but this trend may be related to better detection and diagnostic methods. [9]
Mortality/Morbidity
Most goiters are benign, causing only cosmetic disfigurement. Morbidity or mortality may result from compression of surrounding structures, thyroid cancer, hyperthyroidism, or hypothyroidism.
Race
No racial predilection exists.
Sex
The female-to-male ratio is 4:1.
-
In the Wickham study, 26% of women had a goiter, compared to 7% of men. [8]
-
Thyroid nodules are less frequent in men than in women, but when found, they are more likely to be malignant.
Age
The frequency of goiters decreases with advancing age. The decrease in frequency differs from the incidence of thyroid nodules, which increases with advancing age.
Prognosis
Benign goiters have a good prognosis. However, all goiters should be monitored by examination and biopsy for possible malignant transformation, which may be signaled by a sudden change in size, pain, or consistency. Fortunately, the risk of this is low. In patients exposed to low levels of radiation the risk rises.
Based on the Wickham study, a few of the goiters increased in size. [8]
A small percentage of multinodular goiters do cause hyperthyroidism. Lifelong surveillance is necessary.
Patients with chronic lymphocytic thyroiditis generally have glands that become atrophic.
A study by Sorensen et al found that patients with symptomatic benign nodular goiter who underwent thyroidectomy experienced improvements in tracheal anatomy, inspiratory flow, and health-related quality of life. The investigators found a median 26% improvement in tracheal narrowing and 33% diminishment in tracheal deviation, at 6 months postsurgery. The study also reported a 1% improvement in tracheal narrowing for each 10% reduction in goiter volume. In addition, forced inspiratory flow at 50% of forced vital capacity showed a small improvement. With regard to quality of life, the Impaired Daily Life scale from the Thyroid-Specific Patient-Reported Outcome Measure (ThyPRO) improved by 0.33-points for every 1% reduction in tracheal narrowing. [10, 11]
A study by Chaves et al using the ThyPRO questionnaire indicated that multiple aspects of health-related quality of life improve following surgery in patients with benign non-toxic goiter. Particular improvement was found with regard to overall quality of life, goiter symptoms, and tiredness. [12]
Patient Education
Educate a patient about potential etiologies, eg, adequate dietary iodine intake, avoidance of goitrogens, regular personal neck examination, and physician examination.
For patients on medical therapy, reinforce the need to take medications on a regular basis. Review symptoms of hyperthyroidism.
For excellent patient education resources, visit eMedicineHealth's Thyroid and Metabolism Center. Also, see eMedicineHealth's patient education article Thyroid Problems.
-
Patient with a goiter. Prominent side-view outline.
-
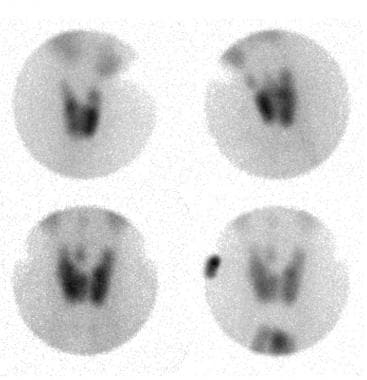
Thyroid nuclear scan of a patient with a euthyroid goiter showing different projections.