Overview
Hypertension is the most common medical problem encountered during pregnancy, complicating up to 10% of pregnancies. [1] Hypertensive disorders during pregnancy are classified into 4 categories, as recommended by the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy [2] :
-
Chronic hypertension
-
Preeclampsia superimposed on chronic hypertension
-
Gestational hypertension (transient hypertension of pregnancy or chronic hypertension identified in the latter half of pregnancy). [2] This terminology is preferred over the older but widely used term "pregnancy-induced hypertension" (PIH) because it is more precise.
The Society of Obstetricians and Gynecologists of Canada (SOGC) released revised guidelines that simplified the classification of hypertension in pregnancy into four categories, pre-existing hypertension, gestational hypertension, preeclampsia, or “other hypertensive effects” on the basis of different diagnostic considerations. [3]
In 2015 and 2017, the American College of Obstetricians and Gynecologists Committee on Obstetric Practice issued updated guidelines regarding the emergency treatment of acute onset severe hypertension during pregnancy, including the following [4, 5, 6] :
-
Acute-onset, severe hypertension that is accurately measured using standard techniques and is persistent for 15 minutes or longer is considered a hypertensive emergency.
-
Intravenous (IV) labetalol and hydralazine have long been considered first-line medications for the management of acute-onset, severe hypertension in pregnant women and women in the postpartum period. Available evidence suggests that oral nifedipine also may be considered as a first-line therapy.
-
Parenteral labetalol should be avoided in women with asthma, heart disease, or congestive heart failure.
-
When urgent treatment is needed before the establishment of IV access, the oral nifedipine algorithm can be initiated as IV access is being obtained, or a 200-mg dose of labetalol can be administered orally. The latter can be repeated in 30 minutes if appropriate improvement is not observed.
-
Magnesium sulfate is not recommended as an antihypertensive agent, but magnesium sulfate remains the drug of choice for seizure prophylaxis in severe preeclampsia and for controlling seizures in eclampsia.
-
Sodium nitroprusside should be reserved for extreme emergencies and used for the shortest amount of time possible because of concerns about cyanide and thiocyanate toxicity in the mother and fetus or newborn, and increased intracranial pressure with potential worsening of cerebral edema in the mother.
-
There is a need for adoption of standardized, evidence-based clinical guidelines for managing patients with preeclampsia. Individuals and institutions should have mechanisms in place to initiate the prompt administration of medication when a patient presents with a hypertensive emergency.
Definitions
Chronic hypertension is defined as blood pressure exceeding 140/90 mm Hg before pregnancy or before 20 weeks' gestation. When hypertension is first identified during a woman's pregnancy and she is at less than 20 weeks' gestation, blood pressure elevations usually represent chronic hypertension.
In contrast, new onset of elevated blood pressure readings after 20 weeks' gestation mandates the consideration and exclusion of preeclampsia. Preeclampsia occurs in 3-6% of all pregnancies and the incidence is 1.5 to 2 times higher in first time pregnancies. [7] Hypertensive disorders in pregnancy may cause maternal and fetal morbidity, and they remain a leading source of maternal mortality.
The following is a computed tomography (CT) image of the brain in a woman who suffered an eclamptic seizure.
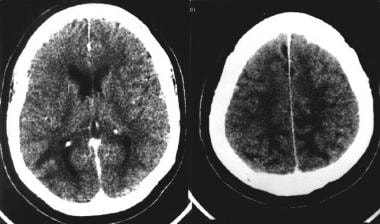 Nonenhanced computed tomography scan of a woman's brain following an eclamptic seizure, showing hypodense areas involving white matter of the occipital lobes and the high frontal/parietal lobes. Courtesy of Aashit K Shah, MD.
Nonenhanced computed tomography scan of a woman's brain following an eclamptic seizure, showing hypodense areas involving white matter of the occipital lobes and the high frontal/parietal lobes. Courtesy of Aashit K Shah, MD.
For patient education information, see Pregnancy Center, as well as High Blood Pressure.
To see complete information on Hypertension, please go to the Medscape Drugs & Diseases article by clicking here.
Chronic Hypertension
Chronic hypertension is a primary disorder in 90-95% of cases and may be either essential (90%) or secondary to some identifiable underlying disorder, such as renal parenchymal disease (eg, polycystic kidneys, glomerular or interstitial disease), renal vascular disease (eg, renal artery stenosis, fibromuscular dysplasia), endocrine disorders (eg, adrenocorticosteroid or mineralocorticoid excess, pheochromocytoma, hyperthyroidism or hypothyroidism, growth hormone excess, hyperparathyroidism), coarctation of the aorta, or oral contraceptive use. About 20-25% of women with chronic hypertension develop preeclampsia during pregnancy. [8]
Chronic hypertension occurs in up to 22% of women of childbearing age, with the prevalence varying according to age, race, and body mass index (BMI). Population-based data indicate that approximately 1% of pregnancies are complicated by chronic hypertension, 5-6% by gestational hypertension (without proteinuria), and 3-6% by preeclampsia. [9, 7]
Differential Diagnosis
Antiphospholipid Antibody Syndrome and Pregnancy
Autoimmune Thyroid Disease and Pregnancy
Common Pregnancy Complaints and Questions
Diabetes Mellitus and Pregnancy
Disseminated Intravascular Coagulation
Gastrointestinal Disease and Pregnancy
Hematologic Disease and Pregnancy
Pulmonary Disease and Pregnancy
Systemic Lupus Erythematosus and Pregnancy
Preeclampsia
Although the exact pathophysiologic mechanism is not clearly understood, preeclampsia is primarily a disorder of placental dysfunction leading to a syndrome of endothelial dysfunction with associated vasospasm. In most cases, pathology evaluation demonstrates evidence of placental insufficiency with associated abnormalities such as diffuse placental thrombosis, an inflammatory placental decidual vasculopathy, and/or abnormal trophoblastic invasion of the endometrium. These findings support abnormal placental development or placental damage from diffuse microthrombosis as being central to the development of this disorder. There is also evidence to indicate an altered maternal immune response to fetal/placental tissue may contribute to the development of preeclampsia.
The widespread endothelial dysfunction may manifest as a maternal syndrome, fetal syndrome, or both. The pregnant woman may manifest dysfunction of multiple organ systems, including the central nervous, hepatic, pulmonary, renal, and hematologic systems. Endothelial damage leads to pathologic capillary leak that can present in the mother as rapid weight gain, nondependent edema (face or hands), pulmonary edema, hemoconcentration, or a combination thereof. The diseased placenta can also affect the fetus via decreased uteroplacental blood flow. This decrease in perfusion can manifest clinically as nonreassuring fetal heart rate testing, low scores on a biophysical profile, oligohydramnios, or as fetal growth restriction.
The hypertension occurring in preeclampsia is due primarily to vasospasm, with arterial constriction and relatively reduced intravascular volume compared with that of a normal pregnancy. The vasculature of normal pregnant women typically demonstrates decreased responsiveness to vasoactive peptides such as angiotensin-II and epinephrine.
In contrast, women who develop preeclampsia typically show a hyperresponsiveness to these hormones, an alteration that may be seen even before the hypertension and other manifestations of preeclampsia become apparent. In addition, blood pressures in preeclampsia are labile, and the normal circadian blood pressure rhythms may be blunted or reversed. One study found increased arterial stiffness in women with preeclampsia, as well as in those with gestational hypertension, compared with normotensive controls; treatment with alpha methyldopa significantly improved the vascular stiffness in preeclampsia but did not normalize it. [10]
Risk factors
Preeclampsia is more common at the extremes of maternal age (< 18 y or >35 y). The increased prevalence of chronic hypertension and other comorbid medical illnesses in women older than 35 years may explain the increased frequency of preeclampsia among older gravidas. In addition, black women have higher rates of preeclampsia complicating their pregnancies compared with other racial groups, mainly because they have a greater prevalence of underlying chronic hypertension. Among women aged 30-39 years, chronic hypertension is present in 22.3% of black persons, 4.6% of non-Hispanic white persons, and 6.2% of Mexican Americans. Hispanic women generally have blood pressure levels that are the same as or lower than those of non-Hispanic white women.
Women who develop preeclampsia during pregnancy have an increased risk of recurrent preeclampsia during subsequent pregnancies. The overall risk is about 18%. The risk is higher (50%) in women who develop severe early preeclampsia (ie, before 27 weeks' gestation). These women are also at increased risk for cardiovascular disease later in life. Whether the preeclampsia increases cardiovascular risk or the 2 conditions share a common underlying cause remains unclear. [11]
Maternal personal risk factors for preeclampsia
The following are maternal personal risk factors for preeclampsia:
-
First pregnancy
-
New partner/paternity
-
Age younger than 18 years or older than 35 years
-
History of preeclampsia
-
Family history of preeclampsia in a first-degree relative
-
Black race
-
Obesity (BMI ≥30)
-
Interpregnancy interval less than 2 years or longer than 10 years
Maternal medical risk factors for preeclampsia
The following are maternal medical risk factors for preeclampsia:
-
Chronic hypertension, especially when secondary to such disorders as hypercortisolism, hyperaldosteronism, pheochromocytoma, or renal artery stenosis
-
Renal disease
-
Thrombophilia
-
Use of selective serotonin uptake inhibitor antidepressants (SSRIs) beyond the first trimester [13]
Placental/fetal risk factors for preeclampsia
The following are placental/fetal risk factors for preeclampsia:
-
Multiple gestations
-
Gestational trophoblastic disease
-
Triploidy
Gestational Hypertension
Gestational hypertension refers to hypertension with onset in the latter part of pregnancy (>20 weeks' gestation) without any other features of preeclampsia, and followed by normalization of the blood pressure postpartum. Of women who initially present with apparent gestational hypertension, about one third develops the syndrome of preeclampsia. As such, these patients should be observed carefully for this progression. The pathophysiology of gestational hypertension is unknown, but in the absence of features of preeclampsia, the maternal and fetal outcomes are usually normal.
Gestational hypertension may, however, be a harbinger of chronic hypertension later in life. A prospective study by Levine et al showed that patients with hypertensive disorders of pregnancy have a 2.4-fold higher risk for the development of new hypertension 10 years later, compared with patients who do not have such a history. [14]
Hypertensive disorders in pregnancy are among the leading causes of maternal mortality, along with thromboembolism, hemorrhage and nonobstetric injuries. Between 2011 and 2013, pregnancy-induced hypertension caused 7.4% of maternal deaths in the United States. [15] Furthermore, hypertension before pregnancy or during early pregnancy is associated with a twofold increased risk of gestational diabetes mellitus [16] Transient hypertension of pregnancy (ie, the development of isolated hypertension in a woman in late pregnancy without other manifestations of preeclampsia) is associated strongly with later development of chronic hypertension.
Although maternal diastolic blood pressure (DBP) greater than 110 mm Hg is associated with an increased risk for placental abruption and fetal growth restriction, superimposed preeclamptic disorders cause most of the morbidity due to chronic hypertension during pregnancy (see Complications).
Evaluation
Determining whether elevated blood pressure identified during pregnancy is due to chronic hypertension or to preeclampsia is sometimes a challenge, especially if no recorded blood pressures from the first half of the gestation are available. Clinical characteristics obtained via history, physical examination, and certain laboratory investigations may be used to help clarify the diagnosis. See Introduction for important maternal and fetal risk factors for preeclampsia that are essential to the history.
Gestational age
Hypertension before 20 weeks' gestation is almost always due to chronic hypertension; new-onset or worsening hypertension after 20 weeks' gestation should lead to a careful evaluation for manifestations of preeclampsia. However, preeclampsia is rare before the third trimester, and the diagnosis of severe hypertension or preeclampsia in the first or early second trimester necessitates exclusion of gestational trophoblastic disease and/or molar pregnancy.
Symptoms of preeclampsia
Symptoms of preeclampsia may include visual disturbances, typically scintillations and scotomata, presumed to be due to cerebral vasospasm. The woman may describe new-onset headache that is frontal, throbbing, or similar to a migraine headache, and gastrointestinal complaints of sudden, new-onset, constant epigastric pain that may be moderate to severe in intensity and due to hepatic swelling and inflammation, with stretch of the liver capsule.
Although mild lower extremity edema is common in normal pregnancy, descriptions of rapidly increasing or nondependent edema may be a signal of developing preeclampsia; note, however, that edema is no longer included among the criteria for the diagnosis of preeclampsia. In addition, rapid weight gain is a result of edema due to capillary leak as well as renal sodium and fluid retention.
Cardiovascular findings in preeclampsia
Home and ambulatory blood pressure measurements are increasingly being used in the pregnant population. Assuming the blood pressure device is accurate (validated relative to an office measurement), the measurements may provide valuable additional data regarding hypertension severity and control during pregnancy.
In most normal pregnancies, the woman has some lower extremity edema by the third trimester. In contrast, a sudden worsening in dependent edema, edema in nondependent areas (such as the face and hands), or rapid weight gain suggest a pathologic process and warrant further evaluation for preeclampsia. Preeclampsia is a multisystem disease with various physical signs.
Women should be allowed to sit quietly for 5-10 minutes before each blood pressure measurement. Blood pressure should be measured in the sitting position, with the cuff at the level of the heart. Inferior vena caval compression by the gravid uterus while the patient is supine can alter readings substantially, leading to an underestimation of the blood pressure. Similarly, blood pressures measured in the left lateral position may yield falsely low values if the blood pressure is measured in the higher arm, unless the cuff is carefully maintained at the level of the heart.
Korotkoff sounds I (the first sound) and V (the disappearance of sound) should be used to denote the systolic blood pressure (SBP) and DBP, respectively. In about 5% of women, an exaggerated gap exists between the fourth (muffling) and fifth (disappearance) Korotkoff sounds, with the fifth sound approaching zero. In this setting, both the fourth and fifth sounds should be recorded (eg, 120/80/40, with sound I = 120, sound IV = 80, and sound V = 40), because the fourth sound will more closely approximate the true DBP.
Many automated blood pressure cuffs provide reasonable estimates of true blood pressure during normal pregnancy (especially those validated for pregnancy) but tend to underestimate blood pressure in preeclamptic women. Only a few automated blood pressure cuffs have been validated in preeclampsia. Manual blood pressure measurement with a mercury sphygmomanometer remains the criterion standard in this setting.
Maternal SBP greater than 160 mm Hg or DBP greater than 110 mm Hg denotes severe disease; depending on the gestational age and maternal status, delivery should be considered for sustained pressures in this range.
Ophthalmologic findings in preeclampsia
Retinal vasospasm is a severe manifestation of maternal disease; consider delivery. In addition, retinal edema is known as serous retinal detachment. This can manifest as severely impaired vision if the macula is involved. It generally reflects severe preeclampsia and should also lead to prompt consideration of delivery. The condition typically resolves upon completion of pregnancy and resolution of the hypertension and fluid retention.
Gastrointestinal findings in preeclampsia
Right upper quadrant (RUQ) abdominal tenderness stems from liver swelling and capsular stretch. Consider delivery.
Central nervous system findings in preeclampsia
Brisk, or hyperactive, reflexes are common during pregnancy. Clonus is a sign of neuromuscular irritability that usually reflects severe preeclampsia.
Signs suggesting a secondary medical cause of chronic hypertension
Centripetal obesity, "buffalo hump," and/or wide purple abdominal striae suggest glucocorticoid excess; other clinical signs may demonstrate hyperthyroidism, hypothyroidism, or growth hormone excess. In addition, a systolic bruit heard over the abdomen or in the flanks suggests renal artery stenosis, whereas radio femoral delay or diminished pulses in the lower versus upper extremities suggests coarctation of the aorta.
Signs of end-organ damage from chronic hypertension
The presence of S4 on cardiac auscultation is not a normal finding in pregnancy. It suggests left ventricular hypertrophy (LVH) or diastolic dysfunction due to preeclampsia-induced vasospasm. Furthermore, in pregnancy, and particularly in the presence of preeclampsia, any sustained cardiac gallop may be a pathologic finding and warrants further evaluation with echocardiography. However, a well-conducted phonocardiographic study of pregnant women found a soft, intermittent S3 to be common in normal pregnancy.
Carotid bruits may reflect atherosclerotic disease due to longstanding hypertension, and Retinal changes of chronic hypertension may be noted.
Diagnostic Overview
Determining whether elevated blood pressure identified during pregnancy is due to chronic hypertension or to preeclampsia is sometimes a challenge, especially if no recorded blood pressures from the first half of the gestation are available. Clinical characteristics obtained via history, physical examination, and certain laboratory investigations may be used to help clarify the diagnosis. Fetal well-being must also be considered with the workup of the mother.
Preeclampsia is rare before the third trimester, and the diagnosis of severe hypertension or preeclampsia in the first or early second trimester necessitates exclusion of gestational trophoblastic disease and/or molar pregnancy. Mild lower extremity edema is common in normal pregnancy, but rapidly increasing or nondependent edema may be a signal of developing preeclampsia. However, edema is no longer included among the criteria for the diagnosis of preeclampsia.
New seizures in pregnancy suggest preeclampsia-eclampsia, but primary neurologic disorders must be excluded.
Routine Tests
Laboratory testing to evaluate chronic hypertension (if not done previously or recently) includes testing for target organ damage, potential secondary causes of hypertension, and other risk factors.
Blood tests to order when evaluating eclampsia include those suggested to evaluate for preeclampsia. Such studies include: urinalysis; complete blood cell (CBC) count; and serum sodium, potassium, creatinine, and glucose levels (the presence of high levels of progesterone, an aldosterone antagonist, during a normal pregnancy may mask the hypokalemia from hyperaldosteronism).
Other suggested tests include measurements of creatinine clearance, blood urea nitrogen (BUN), albumin, 24-hour urinary protein, serum calcium, uric acid, glycosylated hemoglobin, thyroid-stimulating hormone (TSH), liver enzymes and bilirubin, and a urine dip for protein.
For a woman with chronic hypertension in her first trimester, obtain the following laboratory studies (to serve as baseline values, to be referred to later in the pregnancy if a concern regarding superimposed preeclampsia arises): CBC count, electrolytes, BUN, creatinine, liver enzymes, and urine dip for protein and a 24-hour urine collection for creatinine clearance and protein excretion.
Spot urine specimens for obtaining protein/creatinine ratio can fulfill the proteinuria diagnostic criteria for pre-eclampsia. A ratio of greater than 0.3 (when each is measured as mg/dL) is an acceptable equivalent to 24 urine protein greater than 300mg/day for diagnosis of pre-eclampsia. [1]
Serum lipids (ie, total cholesterol, high-density lipoprotein [HDL], low-density lipoprotein [LDL], triglycerides) predictably increase during pregnancy, so measurement should be deferred until the postpartum period. In addition, the increase in endogenous corticosteroid levels during normal pregnancy makes it difficult to evaluate for secondary hypertension due to adrenal corticosteroid excess. Hyperaldosteronism and hypercortisolism are difficult to diagnose during pregnancy due to the high levels of progesterone and the normal increase in endogenous cortisol output.
Preeclampsia/Gestational Hypertension Screening
Researchers in the United Kingdom have developed a method for first-trimester screening to identify women at risk for the development of preeclampsia or gestational hypertension. The screening algorithm uses a combination of maternal variables, including mean arterial pressure, uterine artery pulsatility index, pregnancy-associated plasma protein-A, and placental growth factor. The algorithm proved especially effective for predicting early preeclampsia (ie, requiring delivery before 34 weeks). [17] Screening strategies for preeclampsia other than evaluating for risk factors through a detailed medical history are not currently recommended by ACOG or SMFM. [18]
A cohort study that covered over 13,000 pregnancies by Egeland et al found that gestational hypertension and preeclampsia share several preconception risk factors, some of which could be modified to reduce the risk of adverse pregnancy outcomes. The baseline risk factors shared among gestational hypertension and preeclampsia were: family history of diabetes mellitus, a women's own diabetes status prior to conception, a high total cholesterol/high-density lipoprotein cholesterol ratio (>5), overweight and obesity, and elevated blood pressure status. For preeclampsia but not gestational hypertension, a family history of myocardial infarction before 60 years of age and elevated triglyceride levels also predicted risk. [19, 20]
Hematologic Evaluation
Include a CBC count. In cases in which an incidental platelet count is less than 150,000/µL, 75% are secondary to dilutional thrombocytopenia of pregnancy, 24% are due to preeclampsia, and about 1% of cases are due to other platelet disorders not related to pregnancy. Counts less than 100,000/µL suggest preeclampsia or immune thrombocytopenic purpura (ITP). Examination of the peripheral blood smear for evidence of microangiopathic hemolysis and thrombocytopenia may reveal the presence of red blood cell (RBC) fragments. In this setting, the diagnoses of hemolytic-uremic syndrome (HUS), thrombotic thrombocytopenic purpura (TTP), and HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet [count]) should also be considered.
Hemoglobin levels greater than 13 g/dL suggest the presence of hemoconcentration. Low levels may be due to microangiopathic hemolysis or iron deficiency. Prothrombin time (PT) and/or international normalized ratio (INR) and/or activated partial prothrombin time (aPTT) results may be abnormal in consumptive coagulopathy and disseminated intravascular coagulopathy (DIC) complicating severe preeclampsia. However, checking the PT/INR/aPTT is not necessary in the absence of abnormal liver transaminases or thrombocytopenia.
Abnormal values of lactate dehydrogenase (LDH), bilirubin, haptoglobin, fibrinogen, and D-dimers may confirm the presence of hemolysis and DIC, along with coagulation testing. It is unnecessary to check levels of LDH, bilirubin, haptoglobin, fibrinogen, and D-dimers, unless the PT/INR/aPTT results are abnormal, thrombocytopenia is present, or the hemoglobin level is dropping.
Renal and Hepatic Evaluation
Kidneys
Urinalysis may be used as a screen for proteinuria. Trace levels to +1 proteinuria are acceptable, but levels of +2 or greater are abnormal and should be quantified with a 24-hour urine collection or spot urine protein-creatinine ratio.
In a 24-hour urine collection, the reference range for protein excretion in pregnancy is up to 300 mg/d. Higher levels are abnormal and may reflect renal involvement in preeclampsia. Creatinine clearance increases approximately 50% during pregnancy, and levels less than 100 mL/min suggest renal dysfunction that is either chronic or due to preeclampsia.
Serum creatinine is usually less than 0.8 mg/dL during pregnancy; higher levels suggest intravascular volume contraction or renal involvement in preeclampsia. A serum uric acid level greater than 5 mg/dL is abnormal; this is a sensitive but nonspecific marker of tubular dysfunction in preeclampsia.
Liver
Elevated levels of hepatic transaminases may reflect hepatic involvement in preeclampsia; these increased values may occur in the absence of epigastric/RUQ pain.
Chest Radiography
Imaging studies should not be performed in an unstable patient, and they should not delay rapid facilitated delivery in a woman thought to have severe preeclampsia or eclampsia.
Obtain chest radiographs to evaluate for pulmonary edema in the setting of dyspnea or hypoxia occurring in a woman with preeclampsia, as shown in the following image.
 Noncardiogenic pulmonary edema in a patient with preeclampsia. This is due to a capillary leak that can be a primary component of preeclampsia. The radiograph demonstrates a diffuse increase in lung markings without the cephalization or vascular redistribution that is seen in patients with pulmonary edema from systolic dysfunction. This patient had rapid clinical improvement after only 10 mg of intravenous furosemide.
Noncardiogenic pulmonary edema in a patient with preeclampsia. This is due to a capillary leak that can be a primary component of preeclampsia. The radiograph demonstrates a diffuse increase in lung markings without the cephalization or vascular redistribution that is seen in patients with pulmonary edema from systolic dysfunction. This patient had rapid clinical improvement after only 10 mg of intravenous furosemide.
The fetal ionizing radiation exposure of one maternal chest radiograph with abdominal shielding is only 0.001 rads. Although no dose of ionizing radiation is absolutely safe during pregnancy, a commonly held acceptable cumulative dose is 5 rads during pregnancy (approximately 5000 maternal chest radiographs could be performed before reaching this safety threshold).
CT Scanning of the Brain and Liver
Brain
Perform a CT scan of the brain to exclude cerebral hemorrhage in the setting of seizures, severe headache, or altered level of consciousness, as depicted in the image below. The fetal radiation exposure with abdominal shielding is well under the permissible 5 rads. CT scan can also be used to exclude mass lesion.
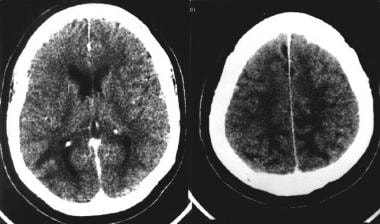 Nonenhanced computed tomography scan of a woman's brain following an eclamptic seizure, showing hypodense areas involving white matter of the occipital lobes and the high frontal/parietal lobes. Courtesy of Aashit K Shah, MD.
Nonenhanced computed tomography scan of a woman's brain following an eclamptic seizure, showing hypodense areas involving white matter of the occipital lobes and the high frontal/parietal lobes. Courtesy of Aashit K Shah, MD.
Findings in women with preeclampsia may include bilateral hypodense areas, called venous infarcts or posterior reversible leukoencephalopathy, in the occipital and parietal regions. They represent focal and reversible areas of edema that are the result of capillary leak or focal areas of impaired venous flow. Generally, these areas resolve as the preeclamptic process reverses.
Liver
Ultrasonography or CT scan of the liver may be used to evaluate for subcapsular hemorrhage or infarction in the setting of persistent severe RUQ pain or markedly elevated hepatic transaminases.
Magnetic Resonance Studies of the Brain
MRI
An MRI may be performed to evaluate for abnormalities of the cerebral cortex (ie, edema, infarction, hemorrhage) in preeclamptic women with severe visual disturbance, seizures, or altered mental status, as seen in the image below. An MRI is more sensitive than a CT scan for detecting cerebral cortical abnormalities but less useful in detecting cerebral hemorrhage.
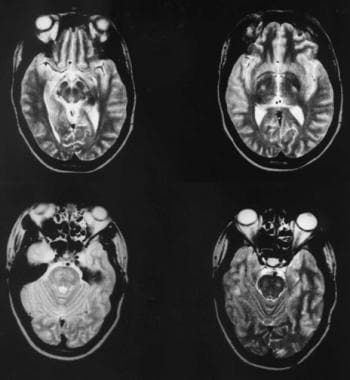 Axial T2-weighted magnetic resonance images of the brain of a woman with eclampsia, showing abnormal areas (hyperintense lesions) affecting the pons, cerebral peduncles, and internal capsules. Courtesy of Aashit K Shah, MD.
Axial T2-weighted magnetic resonance images of the brain of a woman with eclampsia, showing abnormal areas (hyperintense lesions) affecting the pons, cerebral peduncles, and internal capsules. Courtesy of Aashit K Shah, MD.
The classic finding of preeclampsia on T2-weighted images is bilateral occipital bright spots that represent focal edema. This is also known as posterior reversible leukoencephalopathy syndrome, and it is similar to the changes observed when a nonpregnant patient has hypertensive encephalopathy.
Magnetic resonance venography
Magnetic resonance venography may also be performed to exclude cerebral venous sinus thrombosis.
Ultrasonography
Ultrasonography or CT scanning of the liver may be used to evaluate for subcapsular hemorrhage or infarction in the setting of persistent severe RUQ pain or markedly elevated hepatic transaminases.
Echocardiography and Electrocardiography
Limited echocardiography may be performed to evaluate for LVH in chronic hypertension and to exclude cardiomyopathy or occult valvular disease in pregnant women with pulmonary edema.
Perform a 12-lead electrocardiogram (ECG) to evaluate for LVH in women with chronic hypertension.
Electroencephalography
An electroencephalogram (EEG) may be indicated to evaluate recurrent seizure activity, persistent altered level of consciousness, or altered mental status. Following eclampsia, the EEG may reveal epileptiform activity. More commonly, the test shows nonspecific diffuse slowing that may persist for several weeks after delivery.
Renal Scanning
Although not absolutely contraindicated, renal captopril scans involve radioactive isotopes and usually are deferred to the postpartum period.
Fetal Monitoring
Close fetal monitoring under the direction of an obstetrician is essential in pregnant women with preeclampsia. Preeclampsia is a disease of the placenta. When the placenta is severely affected, subtle hypoperfusion of the fetus can occur, which may initially manifest as a decrease in the amniotic fluid level (oligohydramnios), fetal growth restriction, and intrauterine fetal death as a consequence of placental insufficiency. If these problems with the fetus occur, they may be an indication for delivery. Monitoring usually consists of monthly ultrasounds to assess fetal growth after viability and fetal surveillance by biophysical profile weekly or non-stress test twice weekly.
Histologic Findings
Endothelial dysfunction and vasospasm observed in preeclampsia affect multiple regions of the body, including the maternal brain, kidneys, liver, lungs, heart, and placenta. Pathology demonstrates areas of edema, microinfarctions, and microhemorrhage in the affected organs.
The placenta typically shows in situ thrombosis and decidual vasculopathy/incomplete decidualization of the spiral arterioles, which may be part of the pathogenesis of preeclampsia. This can affect the fetus via decreased uteroplacental blood flow. The decrease in flow can manifest clinically as nonreassuring fetal heart rate testing, low score on a biophysical profile, oligohydramnios, and fetal growth restriction.
The kidneys may reveal glomerular endotheliosis that is associated with proteinuria greater than 300 mg in 24 hours or, more rarely, acute tubular necrosis (ATN) or cortical necrosis.
Medical Therapy
Treatment of acute hypertension in pregnancy
Acute severe hypertension in pregnancy is a medical emergency requiring treatment to lower blood pressures within 30 minutes of confirmation to reduce risk of maternal stroke. According to the February 2015 ACOG Committee Opinion #623 “Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Post-Partum Period,” first line options for treatment include oral immediate-release nifedipine, IV labetalol, and IV hydralazine. [4]
Bedrest and hospitalization
Women with worsening hypertension during pregnancy often are placed on bed rest or restricted activity, although no scientific evidence demonstrates that this is beneficial in prolonging gestation or reducing maternal or fetal morbidity/mortality.
Women with hypertension and suspected preeclampsia are typically admitted to a hospital for close observation and investigation. Those with established preeclampsia must be observed very closely, either in hospital or in a comprehensive home monitoring program under the care of an obstetrician.
Pharmacologic considerations
Although the primary risk of chronic hypertension in pregnancy is development of superimposed preeclampsia, no evidence suggests that pharmacologic treatment of mild hypertension reduces the incidence of preeclampsia in this population. [21] A study by Magee et al that analyzed 987 women at 14 to 34 weeks gestation to test the outcomes of less-tight vs. tight control of hypertension found that although primary-outcome rates were similar, severe hypertension (≥160/110 mm Hg) developed at a higher frequency in the less-tight control group (40.6% vs. 27.5%). [22]
In normal pregnancy, women's mean arterial pressure drops 10-15 mm Hg over the first half of pregnancy. Most women with mild chronic hypertension (ie, SBP 140-160 mm Hg, DBP 90-100 mm Hg) have a similar decrease in blood pressures and may not require any medication during this period. Conversely, DBP greater than 110 mm Hg has been associated with an increased risk of placental abruption and intrauterine growth restriction, and SBP greater than 160 mm Hg increases the risk of maternal intracerebral hemorrhage. Therefore, pregnant patients should be started on antihypertensive therapy if the SBP is greater than 160 mm Hg or the DBP is greater than 100-105 mmHg.
ACOG recommends a threshold blood pressure of 140/90 mm Hg for initiation or titration of medical therapy for chronic hypertension in pregnancy, instead of the previously used threshold of 160/110 mm Hg. This recommendation is based on the results of the Chronic Hypertension and Pregnancy (CHAP) Study, which showed that pregnant people who received antihypertensive therapy at a threshold of 140/90 mm Hg had better outcomes than those who received therapy at 160/105 mm Hg or higher. [23]
The goal of pharmacologic treatment should be a DBP of less than 100-105 mm Hg and an SBP less than 160 mm Hg. Women with preexisting end- organ damage from chronic hypertension should have a lower threshold for starting antihypertensive medication (ie, >139/89) and a lower target blood pressure (< 140/90). [3]
If a pregnant woman's blood pressure is sustained greater than 160 mm Hg systolic and/or 110 mm Hg diastolic at any time, lowering the blood pressure quickly with rapid-acting agents is indicated for maternal safety. [4] Anticonvulsant therapy may be undertaken in the setting of severe preeclampsia (primary prophylaxis) or in the setting of eclamptic seizures (secondary prophylaxis). The most effective agent is IV magnesium sulfate; phenytoin is an alternative, although less effective, therapy.
Methyldopa has an established safety record, but it is a mild antihypertensive with a slow onset of action, and associated fatigue may limit patient tolerability of this medication.
Labetalol has a more rapid onset of action, may be given orally or parenterally, and is generally preferred as a first-line agent. [24] One retrospective case-control propensity-score matched study evaluated the association between late trimester exposure to beta-adrenergic blockade with labetalol, metoprolol, and atenolol. and neonatal bradycardia or hypoglycemia. There was a small association between labetalol and neonatal hypoglycemia, the absolute rate in the exposed group was 4.3% versus 1.2% in the nonexposed propensity-score matched group. Labetalol is an effective well tolerated medication that can still be considered a first line agent, and as with any maternal medication, maternal medications should be reviewed by the pediatrician to determine proper neonatal monitoring. [25]
The association between these medications and neonatal hypoglycemia is limited by higher respective prevalences of preexisting and gestational diabetes in the exposed vs. unexposed groups (13.9% vs. 3.8% and 20.6% vs. 8.3%). In spite of a sensitivity analysis, women with diabetes are more likely to have their infants screened for hypoglycemia, so a detection bias cannot be totally excluded. [25]
Should other beta-blocking agents be required for the treatment of hypertension for cardiac conditions, nadolol and metoprolol are reasonable options.
Nifedipine (Long Acting) is a reasonable medication to treat chronic hypertension.
ACE inhibitors should be avoided during pregnancy, as they are associated with fetal renal dysgenesis or death when used in the second and third trimesters, as well as with increased risk of cardiovascular and central nervous system malformations when used in the first trimester. [26] In a retrospective cohort study, Li et al found that during the first trimester, the risk of malformations with the use of ACE inhibitors is similar to the use of other antihypertensives but that the apparent increased risk of malformations is due more to the mother’s underlying hypertension rather than the medications. [27]
Angiotensin II receptor antagonists/blockers are not used during pregnancy, because they have a mechanism of action that is similar to that of ACE inhibitors. Diuretics do not cause fetal malformations but are generally avoided in pregnancy, as they prevent the physiologic volume expansion seen in normal pregnancy. They may be used in states of volume-dependent hypertension, such as renal or cardiac disease.
A healthy fetus depends on a healthy mother, so medications should be used when clear benefit to the mother exists. The US Food and Drug Administration (FDA) categorization for drug use during pregnancy is simplistic and sometimes misleading. To quote the FDA descriptions, any medication in class A through D may be used "when the potential benefit justifies the potential risk."
Available data suggest that all studied agents are excreted into human breast milk, but most are excreted to a negligible degree. All antihypertensive medications are believed to be compatible with breastfeeding, but using medications with a well-established record is reasonable.
Consultations
Most internists do not have extensive exposure to diagnosing and treating medical disorders during pregnancy and therefore feel some discomfort doing so. Women with chronic hypertension in pregnancy should be monitored by an obstetrician. Women with moderate or severe hypertension may benefit from referral to an experienced internist (obstetric medicine specialist), hypertension subspecialist, and/or a specialist in maternal-fetal medicine (perinatologist). The experience of these experts allows them to assess quickly which treatments offer the best risk-benefit ratio. In most situations, the benefit of maximizing maternal well-being with the usual therapies outweighs potential adverse effects on the fetus.
Diagnosis of secondary hypertension during pregnancy can be difficult; an internal medicine consultation may be useful in the care of these women, as well as women with target organ damage due to chronic hypertension and women in whom preeclampsia causes significant organ failure.
Chronic hypertension
Women with mild chronic hypertension often do not require antihypertensive therapy during most of pregnancy. Pharmacologic treatment of mild hypertension does not reduce the likelihood of developing preeclampsia later in gestation and increases the likelihood of intrauterine growth restriction. If maternal blood pressure exceeds 160/100 mm Hg, however, drug treatment is recommended.
Three treatment options are available in cases of mild chronic hypertension in pregnancy. Antihypertensive medication may be withheld or discontinued, with subsequent close observation of blood pressure. Because blood pressure drops during normal pregnancy and no data support the use of medication in patients with blood pressures less than 160/100 mm Hg, the authors recommend this option most often.
If a woman is on pharmacologic treatment with an agent not recommended for use in pregnancy, she may be switched to an alternative antihypertensive agent preferred for use in pregnancy. If a woman is on pharmacologic treatment with an agent acceptable for use in pregnancy, she may continue her current antihypertensive therapy.
Women with chronic hypertension in pregnancy should be monitored for the development of worsening hypertension and/or the development of superimposed preeclampsia (the risk is approximately 25%). Laboratory investigations for preeclampsia should be repeated if the patient's blood pressure increases or if she develops signs or symptoms of preeclampsia (see Routine Tests).
Preeclampsia
Women with suspected, mild, or diagnosed preeclampsia remote from term or labile blood pressures due to chronic hypertension and/or gestational hypertension should be hospitalized for close observation, bed rest, and frequent fetal monitoring. The severity of any abnormalities on admission dictates the frequency of blood work. When diagnosed with preeclampsia, delivering the baby is always in the mother's best interest. Any delay in delivery should be due to uncertainty about the diagnosis or immaturity of the fetus.
Daily examination should include a funduscopic examination for retinal spasm or edema, lung examination for signs of volume overload, cardiac examination for gallop rhythms, abdominal examination for hepatic tenderness, extremities/sacrum examination for increasing edema, and neurologic examination for clonus.
Women with preeclampsia remote from term (ie, < 34-36 weeks' gestation) should be promptly transferred to a facility with adequate resources to care for premature newborn infants. This is essential because worsening preeclampsia disease activity may require urgent delivery at any time.
When preeclampsia develops remote from term (ie, < 34-36 weeks' gestation), attempts are often made to prolong the pregnancy to allow for further fetal growth and maturation. In this setting, both maternal and fetal status must be very closely monitored in a high-risk obstetric center. Fetal testing should be performed at least twice weekly, using a combination of biophysical profiles and nonstress testing supervised by an obstetrician (see Fetal Monitoring). Facilitated delivery should occur if either maternal or fetal deterioration is noted, with the mode of delivery decided by obstetric indications.
Treating hypertension secondary to preeclampsia with medications may reassure the clinician falsely but does not slow progression of the process; therefore, if treatment with antihypertensives is undertaken, clinicians must remain vigilant for all other symptoms, signs, and laboratory evidence of worsening preeclampsia. Other symptoms and signs of worsening preeclampsia must be sought routinely and delivery facilitated if the maternal or fetal condition worsens.
Patients who are diagnosed with HELLP syndrome are typically delivered after corticosteroids have been completed for fetal benefit. Occasionally, the patient may be too unstable to wait for the full benefit of steroids, and immediate delivery should be considered.
Long-Term Monitoring
Women with preeclampsia require follow-up after hospital discharge to ensure normalization of blood pressure and any noted laboratory abnormalities. This follow-up may be undertaken via an internal medicine specialist (obstetric internist) and obstetrician or a family physician.
Hypertension due to preeclampsia may worsen or even present in the postpartum period. After delivery, women with preeclampsia require ongoing close blood pressure monitoring. Blood pressure sustained greater than 160/110 mm Hg should be urgently treated with IV antihypertensives. Oral antihypertensive therapy should be undertaken for sustained pressures above 155/105 mm Hg. As vasospasm resolves, these women may be weaned off their antihypertensive therapy.
Blood pressure changes due to preeclampsia usually resolve within days to weeks after delivery but may persist for 3 months. Persistent hypertension beyond this point probably represents chronic hypertension.
Laboratory abnormalities related to preeclampsia (eg, proteinuria, thrombocytopenia, liver enzyme elevations) should be followed until the abnormalities return to the reference range. Failure to normalize warrants an evaluation for other acute or chronic medical disorders with potential long-term consequences.
Preeclampsia and related disorders identify women at increase risk for future cardiovascular disease. [28] These women should be screened for cardiovascular risk factors, including cigarette smoking, glucose intolerance, low high-density lipoprotein cholesterol, elevated triglycerides, and obesity. The presence of any of these risk factors should be addressed with appropriate treatment and counseling regarding smoking cessation, diet, exercise, glucose control, weight loss, and appropriate medical treatment.
Deterrence/Prevention of Preeclampsia
Pharmacologic treatment and normalization of chronic hypertension does not reduce the risk of developing superimposed preeclampsia. Other therapies that have been tried include low-dose acetylsalicylic acid (ASA), [29] supplemental calcium, [30] salt restriction, [31] supplemental magnesium, [32] and fish oil therapy. [33] Although well-designed randomized trials of ASA in high-risk populations showed no benefit in reducing the frequency of preeclampsia, a meta-analysis reported an approximate 15% reduction in preeclampsia among pregnant women taking low-dose ASA when women began taking it before 16 weeks' gestation. [34, 35] This therapy appears very safe and might be considered in high-risk women. None of the other therapies have demonstrated any significant preventive benefit.
Multiple dietary interventions and supplements have been investigated for a role in preventing preeclampsia, but none has shown any consistent beneficial effect. One trial demonstrated some preventive benefit to supplemental antioxidants (vitamins C and E), but a 2008 review found that the evidence did not support routine use of antioxidants for this purpose. [36] In 2010, Roberts et al reported the outcome data for nearly 1000 nulliparous women in which no significant differences between vitamin and placebo groups were observed in reducing the rate of adverse maternal or perinatal outcomes related to pregnancy-associated hypertension. [37] The study was a multicenter, randomized, double-blind trial of nulliparous women at low risk for preeclampsia.
Complications of Gestational Hypertension
Several complications that affect different organ systems need to be considered in gestational hypertension.
Life-threatening complications in preeclampsia
Superimposed preeclamptic disorders on hypertension during pregnancy may lead to severe maternal complications, including eclamptic seizures, intracerebral hemorrhage, pulmonary edema (due to capillary leak, myocardial dysfunction, excess IV fluid administration), acute renal failure (due to vasospasm, acute tubular necrosis [ATN], or renal cortical necrosis), proteinuria greater than 4-5 g/d, HELLP syndrome (microangiopathic hemolysis, elevated liver enzymes, and thrombocytopenia [platelets < 100/µL]), hepatic swelling with or without liver dysfunction, hepatic infarction/rupture and subcapsular hematoma (which may lead to massive internal hemorrhage and shock), DIC and/or consumptive coagulopathy (rare). Consumptive coagulopathy is usually associated with placental abruption and is uncommon as a primary manifestation of preeclampsia.
Fetal complications include abruptio placentae, intrauterine growth restriction, premature delivery, and intrauterine fetal death.
Acute fatty liver of pregnancy
Although a distinct and rare disorder, acute fatty liver has some clinical features similar to, and often overlapping with, severe preeclampsia.
Thrombotic thrombocytopenic purpura and hemolytic-uremic syndrome
Although unrelated to preeclampsia, consider TTP and HUS important disorders in the setting of presumed severe HELLP syndrome.
Special Concerns
Most patients enter pregnancy with the expectation that their pregnancy and delivery will involve nothing but happiness. When severe complications occur, patients often feel scared, angry, and helpless. The best approach is to discuss all issues with patients. Take all possible steps to help the patient and her family understand the complications and treatment. Begin the discussion by providing the diagnosis and reassure the pregnant woman that, in most cases, the complications are not due to her actions or failure to act. Follow with discussion of plans for evaluation and treatment, providing her an opportunity to ask questions. Empower the patient by involving her in the decision-making process.
Patients ask very important questions. Physicians should feel comfortable being honest and telling patients and families when they do not have all of the answers. Physicians should let patients know that they will work to find the answers. This honesty and thoroughness solidifies the physician's reputation as a caring and competent doctor. Consultation with experienced clinicians helps the physician care for the patient and reassure her that all avenues of treatment are being explored.
Many reference texts and articles are available regarding the treatment of medical disorders during pregnancy. Becoming educated about these topics helps physicians feel more comfortable treating and counseling patients.
Guidelines
American College of Obstetricians and Gynecologists
In 2015 and 2017, the American College of Obstetricians and Gynecologists Committee on Obstetric Practice issued updated guidelines regarding the emergency treatment of acute onset severe hypertension during pregnancy, including the following [4, 5, 6] :
-
Acute-onset, severe hypertension that is accurately measured using standard techniques and is persistent for 15 minutes or longer is considered a hypertensive emergency.
-
Intravenous (IV) labetalol and hydralazine have long been considered first-line medications for the management of acute-onset, severe hypertension in pregnant women and women in the postpartum period. Available evidence suggests that oral nifedipine also may be considered as a first-line therapy.
-
Parenteral labetalol should be avoided in women with asthma, heart disease, or congestive heart failure.
-
When urgent treatment is needed before the establishment of IV access, the oral nifedipine algorithm can be initiated as IV access is being obtained, or a 200-mg dose of labetalol can be administered orally. The latter can be repeated in 30 minutes if appropriate improvement is not observed.
-
Magnesium sulfate is not recommended as an antihypertensive agent, but magnesium sulfate remains the drug of choice for seizure prophylaxis in severe preeclampsia and for controlling seizures in eclampsia.
-
Sodium nitroprusside should be reserved for extreme emergencies and used for the shortest amount of time possible because of concerns about cyanide and thiocyanate toxicity in the mother and fetus or newborn, and increased intracranial pressure with potential worsening of cerebral edema in the mother.
-
There is a need for adoption of standardized, evidence-based clinical guidelines for managing patients with preeclampsia. Individuals and institutions should have mechanisms in place to initiate the prompt administration of medication when a patient presents with a hypertensive emergency.
Hypertension Canada and Society of Obstetricians and Gynaecologists of Canada
Women should have their BP measured using a standardized protocol after a period of rest in a quiet environment and be in a sitting position with their arm at the level of the heart using an appropriately sized cuff (ie, length 1.5 times the circumference of the arm).
The arm with higher BP values should be used for hypertension diagnosis and BP monitoring.
Nonsevere elevated BP should be remeasured at the same visit, with at least a gap of 15 minutes from the first measurement.
More than 50% of women with a first BP reading of ≥140/90 mm Hg have white-coat effect.
Hypertension in pregnancy is defined as an SBP ≥140 mm Hg and/or a DBP ≥90 mm Hg (average of at least 2 measurements taken at least 15 minutes apart).
Severity of hypertension in pregnancy is considered on the basis of the presence of target organ involvement (ie, maternal or the fetus itself) as well as the actual BP level.
BP levels between 140/90 mm Hg and < 160/110 mm Hg are considered nonsevere hypertension in pregnancy.
A BP level of ≥160/110 mm Hg is associated with increased risk of maternal stroke in pregnancy and is therefore considered the diagnostic threshold of severe hypertension in pregnancy.
Antihypertensive therapy is recommended for average SBP measurements of ≥140 mm Hg or DBP measurements of ≥90 mm Hg in pregnant women with chronic hypertension, gestational hypertension, or preeclampsia.
Initial antihypertensive therapy should be monotherapy from the following first-line drugs: oral labetalol, oral methyldopa, long-acting oral nifedipine, or other oral β-blockers (acebutolol, metoprolol, pindolol, and propranolol).
Other antihypertensive drugs can be considered as second-line drugs, including clonidine, hydralazine, and thiazide diuretics.
ACE inhibitors and angiotensin receptor blockers should not be used in pregnant women.
A DBP of 85 mm Hg should be targeted for pregnant women receiving antihypertensive therapy with chronic hypertension or gestational hypertension. A similar target could be considered for pregnant women with preeclampsia.
Additional antihypertensive drugs should be used if target BP levels are not achieved with standard-dose monotherapy. Add-on drugs should be from a different drug class chosen from first-line or second-line options.
Women with severe hypertension with SBP ≥160 or DBP ≥110 mm Hg in pregnancy require urgent antihypertensive therapy because it is considered an obstetric emergency.
Questions & Answers
Overview
What are the four categories of hypertensive disorders during pregnancy?
How is chronic hypertension during pregnancy defined?
What is the prevalence of chronic hypertension during pregnancy?
What is the pathogenesis of preeclampsia?
How does the prevalence of preeclampsia vary among different age groups and races?
What are maternal risk factors for preeclampsia?
What are medical risk factors for preeclampsia?
Which placental/fetal factors increase the risk for preeclampsia?
What is gestational hypertension?
What is the prognosis of hypertensive disorders during pregnancy?
How are the types of hypertensive disorders during pregnancy differentiated?
What is the role of gestational age in the diagnosis of hypertensive disorders during pregnancy?
What are the signs and symptoms of preeclampsia?
Which cardiovascular findings suggest preeclampsia?
Which ophthalmologic findings suggest preeclampsia?
Which GI findings suggest preeclampsia?
Which CNS findings suggest preeclampsia?
Which signs and symptoms suggest a secondary medical cause of chronic hypertension during pregnancy?
Which signs suggest end-organ damage from chronic hypertension during pregnancy?
How are hypertensive disorders diagnosed during pregnancy?
What is the role lab testing in the workup of hypertensive disorders during pregnancy?
When during pregnancy should base line lab tests be performed for woman with chronic hypertension?
What is the screening algorithm for preeclampsia/gestational hypertension in the UK?
What is the role of blood tests in the evaluation of hypertensive disorders during pregnancy?
What is the role of urinalysis in the evaluation of hypertensive disorders during pregnancy?
What is the role of hepatic testing in the evaluation of hypertensive disorders during pregnancy?
When are imaging studies contraindicated for evaluation of hypertensive disorders during pregnancy?
What is the role of chest radiography in the evaluation of hypertensive disorders during pregnancy?
What is the role of CT scanning in the evaluation of hypertensive disorders during pregnancy?
What is the role of liver imaging during the evaluation of hypertensive disorders during pregnancy?
What is the role of MRI in the evaluation of hypertensive disorders during pregnancy?
Which findings on MRI are characteristic of preeclampsia?
What is the role of cardiac testing in the evaluation of hypertensive disorders during pregnancy?
What is the role of renal scanning in the evaluation of hypertensive disorders during pregnancy?
What is the role of fetal monitoring in women with preeclampsia?
Which histologic findings characteristic of preeclampsia?
What is the ACOG recommended treatment for acute severe hypertension during pregnancy?
What are the goals of pharmacologic treatment of hypertensive disorders during pregnancy?
What is the role of beta-blocking agents in the treatment of hypertensive disorders of pregnancy?
What is the role of Nifedipine in the treatment of chronic hypertension during pregnancy?
Which medications are contraindicated for the treatment of hypertensive disorders during pregnancy?
What are FDA recommendations for use of medications for hypertensive disorders during pregnancy?
What are the treatment options for mild chronic hypertension during pregnancy?
What are the treatment options for preeclampsia due to chronic hypertension?
What is the treatment for women with HELLP syndrome?
What monitoring is needed for women with preeclampsia following delivery?
What is the role of dietary interventions and supplements in the prevention of preeclampsia?
What are the risks of gestational hypertension?
What are the complications of superimposed preeclamptic disorders on hypertension during pregnancy?
Which disorder has clinical features that overlap with preeclampsia?
Which disorders should be considered in the presence of severe HELLP syndrome?
What education should be given to patients with hypertensive disorders during pregnancy?
-
Nonenhanced computed tomography scan of a woman's brain following an eclamptic seizure, showing hypodense areas involving white matter of the occipital lobes and the high frontal/parietal lobes. Courtesy of Aashit K Shah, MD.
-
Axial T2-weighted magnetic resonance images of the brain of a woman with eclampsia, showing abnormal areas (hyperintense lesions) affecting the pons, cerebral peduncles, and internal capsules. Courtesy of Aashit K Shah, MD.
-
Noncardiogenic pulmonary edema in a patient with preeclampsia. This is due to a capillary leak that can be a primary component of preeclampsia. The radiograph demonstrates a diffuse increase in lung markings without the cephalization or vascular redistribution that is seen in patients with pulmonary edema from systolic dysfunction. This patient had rapid clinical improvement after only 10 mg of intravenous furosemide.
Tables
What would you like to print?
- Overview
- Chronic Hypertension
- Differential Diagnosis
- Preeclampsia
- Gestational Hypertension
- Evaluation
- Diagnostic Overview
- Routine Tests
- Preeclampsia/Gestational Hypertension Screening
- Hematologic Evaluation
- Renal and Hepatic Evaluation
- Chest Radiography
- CT Scanning of the Brain and Liver
- Magnetic Resonance Studies of the Brain
- Ultrasonography
- Echocardiography and Electrocardiography
- Electroencephalography
- Renal Scanning
- Fetal Monitoring
- Histologic Findings
- Medical Therapy
- Deterrence/Prevention of Preeclampsia
- Complications of Gestational Hypertension
- Special Concerns
- Guidelines
- Questions & Answers
- Show All
- Media Gallery
- References






