Background
Neurogenic pulmonary edema (NPE) is a relatively rare form of pulmonary edema caused by an increase in pulmonary interstitial and alveolar fluid. Any acute central nervous system (CNS) insult can result in pulmonary edema. The most common causes are subarachnoid hemorrhage, [1, 2, 3, 4] cerebral hemorrhage, [5] traumatic brain injury (TBI), [6] and seizures. [7]
Neurogenic pulmonary edema most commonly develops within a few hours after a neurologic insult, and is characterized by dyspnea, bilateral basal pulmonary crackles, and the absence of cardiac failure. [8] However, a delayed form of NPE that develops 12 to 24 hours after the CNS insult has been reported. [9] Symptoms often spontaneously resolve within 24 to 48 hours; however, in patients with ongoing brain injury and elevated intracranial pressure (ICP), the NPE often persists.
No specific laboratory study confirms the diagnosis of neurogenic pulmonary edema (NPE). NPE is a diagnosis of exclusion, [9, 10] and diagnosis requires exclusion of other causes of pulmonary edema (eg, high-altitude pulmonary edema).
The management of NPE is focused on treating the underlying neurologic condition. Treatment efforts to reduce ICP, including decompression and clot evacuation, osmotic diuretics, anti-epileptics, tumor resection, and steroids have all been associated with improvements in oxygenation.
For patient education resources, see the Brain and Nervous System Center and Stroke.
Pathophysiology
General
The pathogenesis of neurogenic pulmonary edema (NPE) is not completely understood. [8] Because the most common neurological events are associated with increased intracranial pressure, intracranial hypertension is considered a key etiologic factor.
Within the central nervous system, the sites responsible for the development of neurogenic pulmonary edema are not fully elucidated. Animal studies suggest that hypothalamic lesions, stimulation of the vasomotor centers of the medulla, elevated intracranial pressure, and activation of the sympathetic system have potential roles. [11, 12] Cervical spinal cord nuclei also may have a role. Both hypothalamic lesions (paraventricular and dorsomedial nuclei) and stimulation of the vasomotor centers of the medulla (A1 and A5, nuclei of solitary tract, and area postrema, medial reticulated nucleus, and the dorsal motor vagus nucleus in the medulla oblongata) can increase output along the sympathetic trunk. Neurogenic pulmonary edema trigger zones may exist in these structures, with specific neurologic foci or centers producing massive sympathetic discharges that lead to neurogenic pulmonary edema. [13]
Neuroanatomic structures
The medulla is believed to activate sympathetic components of the autonomic nervous system. Experimentally, bilateral lesions of the nuclei in the medulla produce profound pulmonary and systemic hypertension and pulmonary edema. Alpha-adrenergic blockade (with phentolamine) and spinal cord transection at the C7 level prevent the formation of neurogenic pulmonary edema, suggesting an important role for sympathetic activation.
An acute neurological crisis, accompanied by a marked increase in intracranial pressure, may stimulate the hypothalamus and the vasomotor centers of the medulla. This, in turn, initiates a massive autonomic discharge mediated by preganglionic centers within the cervical spine.
Mechanism of edema formation
A central nervous system event produces a dramatic change in Starling forces, which govern the movement of fluid between capillaries and the interstitium. Both hemodynamic (cardiogenic) and nonhemodynamic (noncardiogenic) components contribute to edema formation. Factors leading to the development of edema in patients with subarachnoid hemorrhage are illustrated in the flowchart below; however, these can be extrapolated to other types of central nervous system insults.
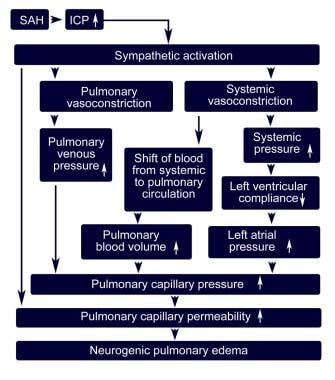 Factors leading to the development of neurogenic pulmonary edema in patients with subarachnoid hemorrhage.
Factors leading to the development of neurogenic pulmonary edema in patients with subarachnoid hemorrhage.
Changes in capillary hydrostatic pressure
Alterations in pulmonary vascular pressures appear to be the most likely Starling force to influence the formation of neurogenic pulmonary edema. Experimental observations suggest the following mechanisms by which pulmonary capillary hydrostatic pressures can be increased acutely:
-
An increase in left atrial pressure may occur because of increases in sympathetic tone and venous return. Left ventricular performance may deteriorate secondary to the direct effects of catecholamines and other mediators, as well as transient systemic hypertension.
-
Pulmonary venoconstriction occurs with sympathetic stimulation, which may increase the capillary hydrostatic pressure and produce pulmonary edema without affecting left atrial or pulmonary capillary wedge pressures.
Changes in pulmonary capillary permeability
An increase in capillary permeability can result in neurogenic pulmonary edema without elevation of pulmonary capillary hydrostatic pressure, because causative hemodynamic alteration is inconsistent. However, evidence shows that alpha-adrenergic blockade can protect against neurogenic pulmonary edema. Epinephrine, norepinephrine, and even a release of secondary mediators may directly increase pulmonary vascular permeability. Whether the capillary leak is produced by pressure-induced mechanical injury because of the elevated capillary hydrostatic pressure or because of some direct nervous system control over the pulmonary capillary permeability remains uncertain.
An initial and rapid rise in pulmonary vascular pressure due to pulmonary vasoconstriction or pulmonary blood flow can lead to pulmonary microvascular injury. Consequently, an increase in vascular permeability results in edema formation, as suggested by the frequent observation of pulmonary hemorrhage in neurogenic pulmonary edema (ie, blast theory). [14, 15, 16]
Etiology
Any acute central nervous system (CNS) insult can result in pulmonary edema. The most common causes of neurogenic pulmonary edema (NPE) are subarachnoid hemorrhage, [1, 2, 3, 4] cerebral hemorrhage, [5] traumatic brain injury (TBI), [6, 17] COVID-19, [18] and seizures. [7] Other conditions, including nonhemorrhagic stroke, [19] medication overdose, arteriovenous malformation, meningitis/encephalitis, [20, 21] and spinal cord infarction, have been reported and linked to the formation of NPE.
Epidemiology
Neurogenic pulmonary edema is an underdiagnosed condition. [22] Patients with neurologic events often have multiple other comorbidities, which may obscure or mimic the diagnosis of neurogenic pulmonary edema. The lack of a standardized definition for neurogenic pulmonary edema also makes defining its epidemiology difficult. [17]
As many as one third of patients with status epilepticus may have evidence of neurogenic pulmonary edema. [7] More than half the patients with severe, blunt, or penetrating head injury have associated neurogenic pulmonary edema. Approximately 71% of fatal cases of subarachnoid hemorrhage are complicated by neurogenic pulmonary edema. Neurogenic pulmonary edema may complicate subarachnoid and intracerebral hemorrhage in 30-70% of patients and may recur after initial resolution. [23, 24]
A series of 457 patients with subarachnoid hemorrhage reported a 6% prevalence of severe neurogenic pulmonary edema. [25] Solenski et al reported in 1995 that increased age and a worse clinical grade of subarachnoid hemorrhage were associated with neurogenic pulmonary edema.
No data suggest differences in the international incidence of neurogenic pulmonary edema compared with the experience in the United States. However, note that epidemiologic data on this entity in general are very sparse because of the difficulties in recognition and diagnosis and lack of a standardized definition.
Age is not a specific risk factor for neurogenic pulmonary edema, other than the increased risk for neurologic events and cardiovascular abnormalities associated with increasing age.
Prognosis
Data regarding morbidity and mortality following neurogenic pulmonary edema (NPE) have not been well documented, given the relatively low prevalence and likely underdiagnosis. Neurogenic pulmonary edema usually is generally well tolerated by the patient, although some patients require ventilatory support. Neurogenic pulmonary edema resolves within 48-72 hours in the majority of affected patients.
Morbidity related to neurogenic pulmonary edema is reported to be in the range of 40-50%, and reported mortality from neurogenic pulmonary edema is low, at approximately 7%. Overall, patient outcome is usually determined by the underlying neurological insult that led to neurogenic pulmonary edema unless significant respiratory complications develop.
Complications include but are not limited to the following:
-
Prolonged hypoxic respiratory failure
-
Hemodynamic instability
-
Nosocomial infections (ie, related to prolonged mechanical ventilation and hospitalization)
-
Neurogenic pulmonary edema in a patient with a subdural hematoma.
-
Progression of neurogenic pulmonary edema in the same patient in the image above, with subdural hematoma (day 2).
-
Factors leading to the development of neurogenic pulmonary edema in patients with subarachnoid hemorrhage.








